A pressure ulcer is defined by the European Pressure Ulcer Advisory Panel as an area of localised damage to the skin and underlying tissue caused by pressure, shear, or friction, or a combination of these. Pressure ulcers are caused by a local breakdown of soft tissue as a result of compression between a bony prominence and an external surface.
They usually develop on the lower half of the body: two thirds around the pelvis and a third on the lower limbs, with heel ulceration becoming more common. Elderly people are the most likely group to have pressure ulcers; this is especially true for those older than 70, up to a third of whom will have had surgery for a hip fracture. Those with spinal injuries form another distinct group, in whom the prevalence is 20%-30% one to five years after injury.
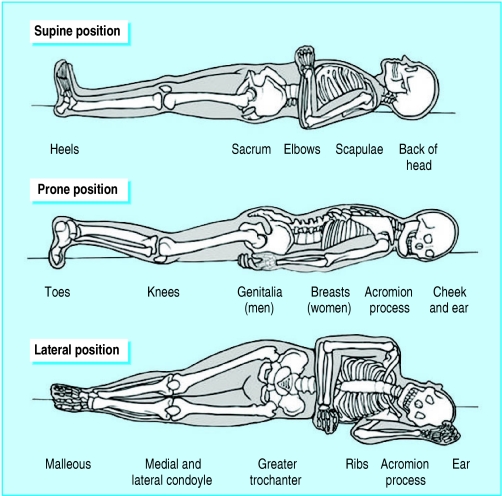
Figure 1.
Common sites of pressure ulceration in individuals at risk of ulceration
Most pressure ulcers arise in hospital, where the prevalence among inpatients is 3%-14%, although it can be as high as 70% in elderly inpatients with orthopaedic problems. The incidence of pressure ulcers in hospitals is 1%-5%. In patients who are confined to bed or to a chair for more than one week, the incidence rises to almost 8%. In long term healthcare facilities 1.5%-25% of patients develop pressure ulcers. Almost a fifth of pressure ulcers develop at home and a further fifth in nursing homes. The prevalence of pressure ulcers in nursing homes is not much higher than in hospitals. Pressure ulceration in elderly patients is associated with a fivefold increase in mortality, and in-hospital mortality in this group is 25%-33%. Estimates of the cost of pressure ulceration to the NHS range from £180m ($318m; €265m) to nearly £2bn a year.
Pathogenesis
The four main factors implicated are interface pressure, shear, friction, and moisture.
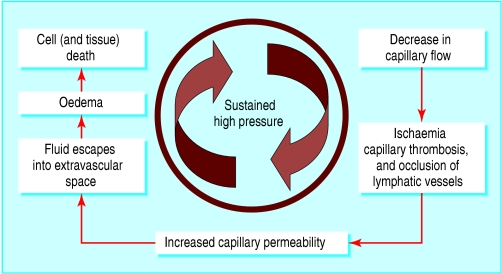
When pressure of short duration is relieved, tissues demonstrate reactive hyperaemia, reflecting increased blood flow to the area. However, sustained high pressure leads to decreased capillary blood flow, occlusion of blood vessels and lymphatic vessels, and tissue ischaemia.
Figure 2.
Pathophysiology of pressure ulceration
These changes are ultimately responsible for necrosis of muscle, subcutaneous tissue, dermis and epidermis, and consequent formation of pressure ulcers. An external pressure of 50 mm Hg may rise to over 200 mm Hg at a bony prominence, leading, with time, to deep tissue destruction, which may not be evident on the surface of the skin. Regular relief from high pressures in the at-risk patient is essential to prevent pressure ulceration.
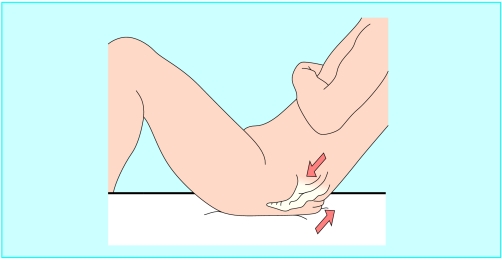
Shear force is generated by the motion of bone and subcutaneous tissue relative to the skin, which is restrained from moving due to frictional forces (for example, when a seated patient slides down a chair or when the head of a bed is raised more than 30°). In such circumstances the pressure needed to occlude the blood vessels is greatly reduced. In elderly patients, a reduced amount of elastin in the skin predisposes to the adverse effects of shear.
Figure 3.
Shear force generated—for example, when a patient slides down a bed
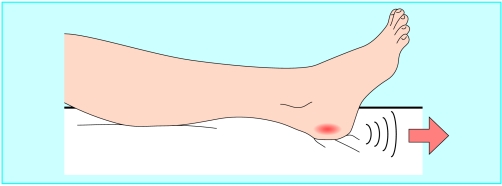
Friction opposes the movement of one surface against another. Frictional forces may lead to the formation of intraepidermal blisters, which in turn lead to superficial skin erosions, initiating or accelerating pressure ulceration. Such forces occur, for example, when a patient is dragged across a bed sheet or as a result of ill fitting prosthetic devices or footwear.
This is the fourth in a series of 12 articles
Most pressure ulcers are avoidable
An excessively moist environment caused, for example, by perspiration, urinary or faecal incontinence, or excessive wound drainage increases the deleterious effects of pressure, friction, and shear. It also causes maceration of the surrounding skin, which compounds these factors. Friction and moisture exert their greatest effects in areas of high pressure: the effects of friction are up to five times worse if moisture is present.
Figure 4.
Friction forces generated—for example, when a patient is dragged across a surface
Classification
Among the various classification schemes for pressure ulceration, the one developed by the European Pressure Ulcer Advisory Panel (EPUAP) uses a simple, four grade classification. No “ideal” classification system exists; the EPUAP's grade 1 ulceration, for example, may be difficult to detect in people with darkly pigmented skin. Eschar (dried, black, hard, necrotic tissue) covering a pressure ulcer prevents accurate grading. Undermining of adjacent tissue, and sinus wounds, commonly occur and can affect grading as well as healing.
Figure 5.




From top left, clockwise: Grade 1 pressure ulcer over greater trochanter; grade 2 pressure ulcers on a below-knee amputation stump due to an ill fitting prosthesis; grade 4 pressure ulcer over the sacrum (with grade 2 pressure ulcers over buttocks); grade 3 pressure ulcer over lateral aspect of calcaneum
Table 1.
Classification of pressure ulcers by grade*
| Grade 1—Non-blanchable erythema of intact skin. Discoloration, warmth, induration, or hardness of skin may also be used as indicators, particularly in people with darker skin |
| Grade 2—Partial-thickness skin loss, involving epidermis, dermis, or both. The ulcer is superficial and presents clinically as an abrasion or blister |
| Grade 3—Full-thickness skin loss involving damage to or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia |
| Grade 4—Extensive destruction, tissue necrosis or damage to muscle, bone, or supporting structures, with or without full-thickness skin loss |
As defined by the European Pressure Ulcer Advisory Panel
Prevention and treatment of pressure ulcers
Risk factors
Age alone is not a risk factor; rather, it is the problems common in elderly people that are associated with pressure ulceration. These include hip fractures, faecal and urinary incontinence, smoking, dry skin, chronic systemic conditions, and terminal illness. The effects of all risk factors should be minimised through their optimal management.
Figure 6.

Eschar covering calcaneal pressure ulcer preventing accurate grading
Table 2.
Risk factors for pressure ulceration*
| Acute illness—Increased metabolic rate and demand for oxygen compromising tissues |
| Age—Chronic disease, cerebrovascular accident, impaired nutrition, confined to chair or bed, faecal incontinence, fractured neck of femur |
| Level of consciousness—Acute or chronic illness, medication (sedatives, analgesics, anaesthetics) |
| Limited mobility or immobility—Cerebrovascular accident, spinal cord injury (hemiparesis, paraparesis, quadriplegia), spasticity, arthritis, orthopaedic problems (especially fracture neck of femur), patients confined to chair or bed |
| Sensory impairment—Neuropathies (for example, diabetes), decreased conscious levels, medication, spinal cord injury |
| Severe chronic or terminal disease—Diabetes, chronic obstructive pulmonary disease, chronic cardiovascular disease, terminal illness |
| Vascular disease—Smoking, diabetes, peripheral vascular disease, anaemia, anti-hypertensives |
| Malnutrition or dehydration |
| History of pressure damage |
Based on NICE guidelines for prevention of pressure ulcers
Immobility (the inability to reposition without help) and limited activity are probably the major risk factors for pressure ulcers and may occur for various reasons. Elderly people are particularly prone to such problems. Sensory deficits give rise to altered ability to perceive the pain and discomfort associated with persistent local pressure, and this leads to reduced frequency of repositioning.
Being confined to bed or to a chair significantly increases the risk of pressure ulceration; appropriate pressure relieving surfaces should be provided. Individuals with increased limb tone (spasticity) may benefit from interventions such as physiotherapy, muscle relaxants (for example, baclofen), nerve block, or surgery. Care should be taken with the use of sedatives, analgesics, and drugs that cause alteration in skin blood flow, such as antihypertensives.
A correlation exists between the degree of malnutrition and the extent and severity of pressure ulceration. In addition, malnutrition slows the healing of pressure ulcers. Measures of nutritional status predictive of pressure ulceration include a recent decrease in body weight, decreased triceps skin-fold thickness, and lymphocytopenia (< 1.8×109). Serum albumin concentration may be used as a surrogate marker, though its relatively long half life does not provide an accurate reflection of nutritional status. More sensitive markers include serum prealbumin and transferrin concentrations; testing for these, however, is not routinely available.
Table 3.
Nutritional support
| • Nutritional support is critical in preventing and managing pressure ulcers |
| • Patients at high risk and those with established ulceration should be assessed and reviewed by a dietitian |
| • Supplementary feeding, either assisted or enteral (via a nasogastric tube or a percutaneous endoscopic gastrostomy (PEG) tube) may be necessary |
| • Supplementation with vitamins and trace elements should also be considered |
| • Adequate hydration is essential |
Risk assessment
A systematic evaluation of risk factors will help to identify patients at risk of pressure ulceration. These individuals should be assessed regularly, and the risk assessment scales should be used as an adjunct to, not a substitute for, clinical judgment. Several risk assessment scales are currently used but vary in the risk factors assessed. The guidelines from the UK National Institute for Health and Clinical Excellence (NICE) state, however, that the provision of pressure relieving devices should also be based on cost considerations and an overall assessment of the individual, not only on risk assessment scores.
Table 4.
Minimum components of risk assessment scales*
| • Age | • Nutrition |
| • Mobility | • Continence |
| • Activity | • Skin status |
| • Level of consciousness | • Illness severity |
Based on NICE recommendations, 2003
Pressure relief
Regular inspection of the skin of patients at risk of pressure ulcers should focus particularly on areas around bony prominences. Excess moisture from, for example, urinary or faecal incontinence, perspiration, or wound drainage should be minimised. Patients confined to bed should be turned at least every two hours, the frequency reflecting the type of support surface used and the degree of risk.
Figure 7.



Left to right: Standard hospital mattress; Low tech (Repose) mattress overlay; static mattress
Table 5.
NICE recommendations for holistic assessment of patient needing pressure relieving device
| • Identified level of risk |
| • Skin assessment |
| • Comfort |
| • General health state |
| • Lifestyle and abilities |
| • Critical care needs |
| • Acceptability of the pressure relieving equipment to patient and carer |
Most patients are nursed on a standard hospital mattress. However, those at risk may need to be nursed on a “static” pressure relieving mattress or mattress overlay, which should not be able to “bottom out”—that is, the mattress should not provide less than 2.5 cm of support).
Figure 8.


Left: Dynamic mattress. Right: Air-fluidised mattress
Table 6.
Components of three risk assessment scales*
| Risk factor | Norton | Waterlow | Braden |
|---|---|---|---|
| Mobility | Yes | Yes | Yes |
| Activity | Yes | No | Yes |
| Nutritional status | No | Yes | Yes |
| Mental status | Yes | No | Yes |
| Incontinence/moisture | Yes | Yes | Yes |
| General physical condition | Yes | Yes | No |
| Skin appearance | No | Yes | No |
| Medication | No | Yes | No |
| Friction/shear | No | No | Yes |
| Weight | No | Yes | No |
| Age | No | Yes | No |
| Specific predisposing diseases | No | Yes | No |
| Prolonged pressure | No | Yes | No |
Data from Flanagan M (J Wound Care 1993;2:215-8)
Dynamic mattresses, air-fluidised mattresses, and dynamic overlays provide alternating pressure relief in a cyclical fashion. They are suited to patients at high risk, including those in whom contact of the pressure with the mattress is unavoidable, those with very large or several ulcers, and those with non-healing ulcers.
Figure 9.

Low tech (Repose) foot protector
Direct (“kissing”) contact of bony prominences such as the knees and ankles should be avoided by use of cushions or foam wedges. Excess abnormal pressure on the heels should be off-loaded using pressure relieving devices. The patient should not be positioned on the femoral trochanter. Pressure and friction should be minimised by maintaining the head of the bed at less than 30° and using appropriate lifting devices rather than dragging patients during transfer and repositioning.
When sitting in a chair or wheelchair, a patient at risk of pressure ulcers should use a pressure relieving cushion to reduce pressure, ensure good sitting balance, and provide comfort. The patient should be encouraged to shift position every 15-30 minutes. If they are unable to do this independently they should be repositioned at least hourly. “Doughnut” or ring cushions should not be used as they may exacerbate rather than prevent the risk of ulceration.
Debridement and dressings
Necrotic or sloughy pressure ulcers should be debrided to promote healing and to enable the stage of the ulcer to be assessed accurately. Devitalised tissue can be removed at the bedside by sharp debridement with a scalpel; local anaesthetic may be needed. Formal surgical debridement may be necessary for extensive grade 3 or 4 pressure ulcers. These ulcers may also require plastic surgery to reconstruct the area. Dressings are the mainstay of treatment of pressure ulcers. Other treatments, including larval and vacuum assisted closure therapies, may be beneficial (see penultimate article in the series).
Figure 10.




Pressure relieving cushions
Table 7.
Dressing types suitable for the treatment of pressure ulcers pressure ulcer grade
| Grade | Dressing type |
|---|---|
| Grade 1, minimally exuding grade 2 | Semipermeable film |
| Low to moderately exuding, non-infected grades 2-3 | Foams |
| Low to moderately exuding grades 2-4 | Hydrogels |
| Low to moderately exuding grades 3-4 | Hydrocolloids |
| Moderate to highly exuding grades 2-4 | Alginates |
| Moderate to highly exuding grades 2-4 | Hydrofibres |
Complications
All pressure ulcers will be colonised with bacteria. Only signs of clinical infection should prompt bacterial culture to confirm the organism and antibiotic sensitivities. Secondary bacteraemia or septicaemia may complicate pressure ulceration, and each of these conditions is associated with increased mortality. Antibiotics are often started empirically, reflecting the site and depth of the pressure ulcer. A chronic, indolent, non-healing wound may reflect the development of underlying osteomyelitis, the flora of which is often Gram negative or anaerobic (treatment of infection is discussed in a later article). Rarely, amyloidosis or malignancy may arise as a result of chronic pressure ulceration.
The three figures on p 472 and the figure at the top of p 473 are adapted from Grey JE, Harding KG. Principles and practice of geriatric medicine. 4th ed. Chichester: Wiley (in press).
The ABC of wound healing is edited by Joseph E Grey (joseph.grey@cardiffandvale.wales.nhs.uk), consultant physician, University Hospital of Wales, Cardiff and Vale NHS Trust, Cardiff, and honorary consultant in wound healing at the Wound Healing Research Unit, Cardiff University, and by Keith G Harding, director of the Wound Healing Research Unit, Cardiff University, and professor of rehabilitation medicine (wound healing) at Cardiff and Vale NHS Trust. The series will be published as a book in summer 2006.
Competing interests: For series editors' competing interests, see the first article in this series.
Further reading and resources
- • European Pressure Ulcer Advisory Panel. Pressure ulcer prevention guidelines. www.epuap.org/glprevention.html
- • Pressure relieving devices. Clinical guidelines. 2003. www.nice.org.uk.
- • Pressure ulcer management. Clinical guidelines. 2005. www.nice.org.uk
- • Cherry GW, Hughes MA, Ferguson MWJ, Leaper DJ. Wound healing. In: Morris DJ, Woods WC, eds. Oxford textbook of surgery. 2nd ed. Oxford: Oxford University Press, 2001.
- • Clark RAF. The molecular and cellular biology of wound repair. 2nd ed. New York: Plenum Press, 1998.
- • Glat PM, Longaker MT. Wound healing. In: Aston SJ, Beasley RW, Thorne CHM, eds. Grabb and Smith's plastic surgery. 5th ed. Philadelphia, PA: Lippincott-Raven, 1997.
- • Brem H, Lyder C. Protocol for the successful treatment of pressure ulcers. Am J Surg 2004;188(Suppl 1A): 9-17. [DOI] [PubMed] [Google Scholar]
- • Brem H, Jacobs T, Vileikyte L, Weinberger S, Gibber M, Gill K, et al. Wound-healing protocols for diabetic foot and pressure ulcers. Surg Technol Int (2003);11: 85-92. [PubMed] [Google Scholar]
- • Cullum N, McInnes E, Bell-Syer SE, Legood R. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev 2004;(3):CD001735. [DOI] [PubMed]
- • Langer G, Schloemer G, Knerr A, Kuss O, Behrens J. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev 2003;(4):CD003216. [DOI] [PubMed]