Abstract
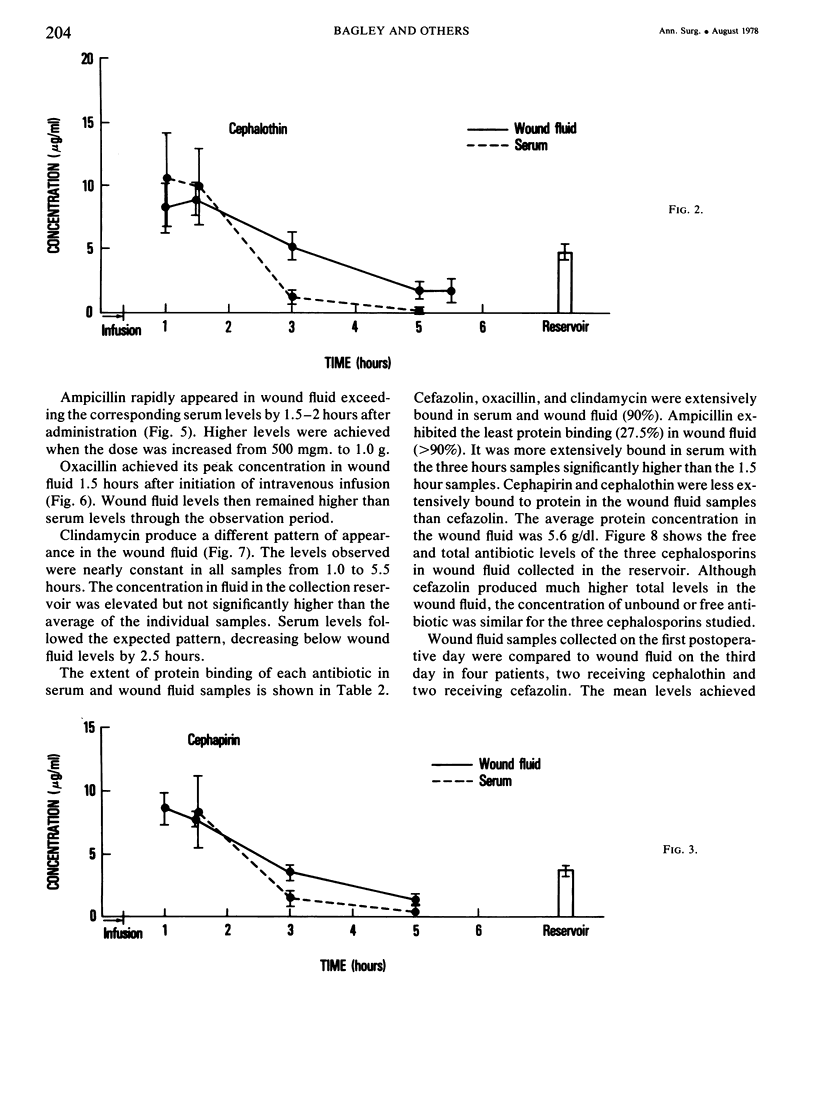
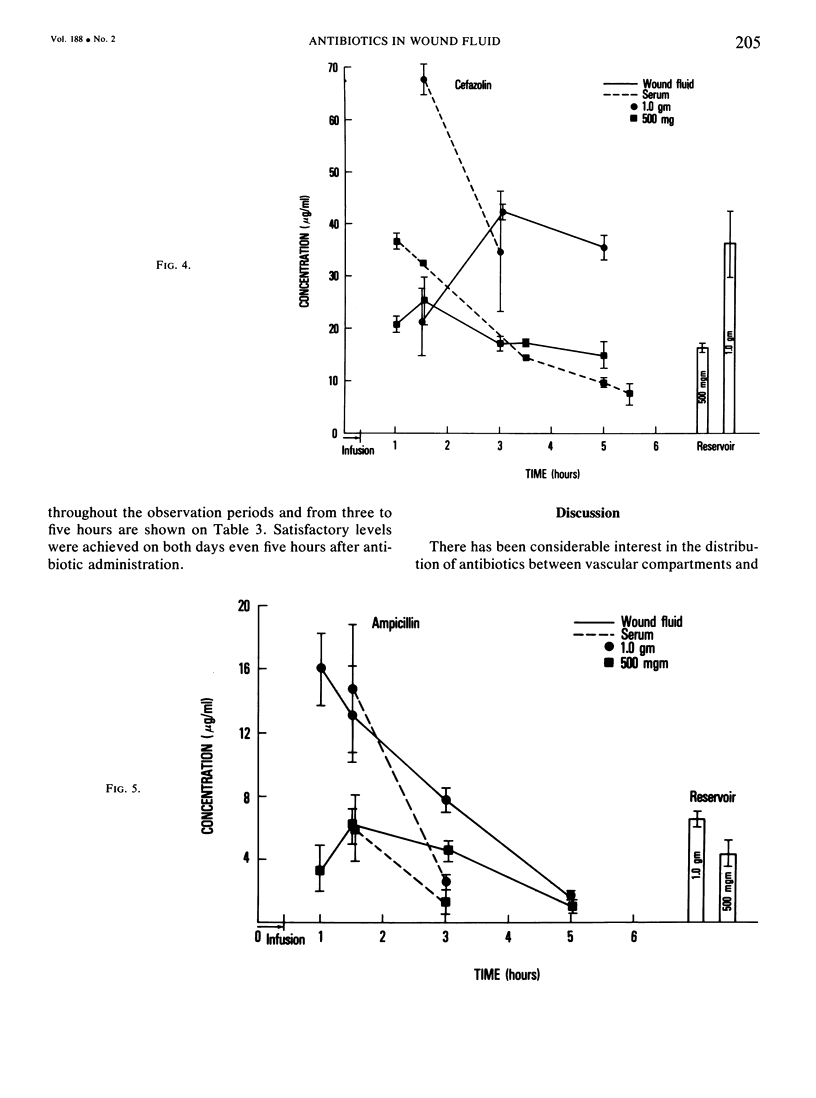
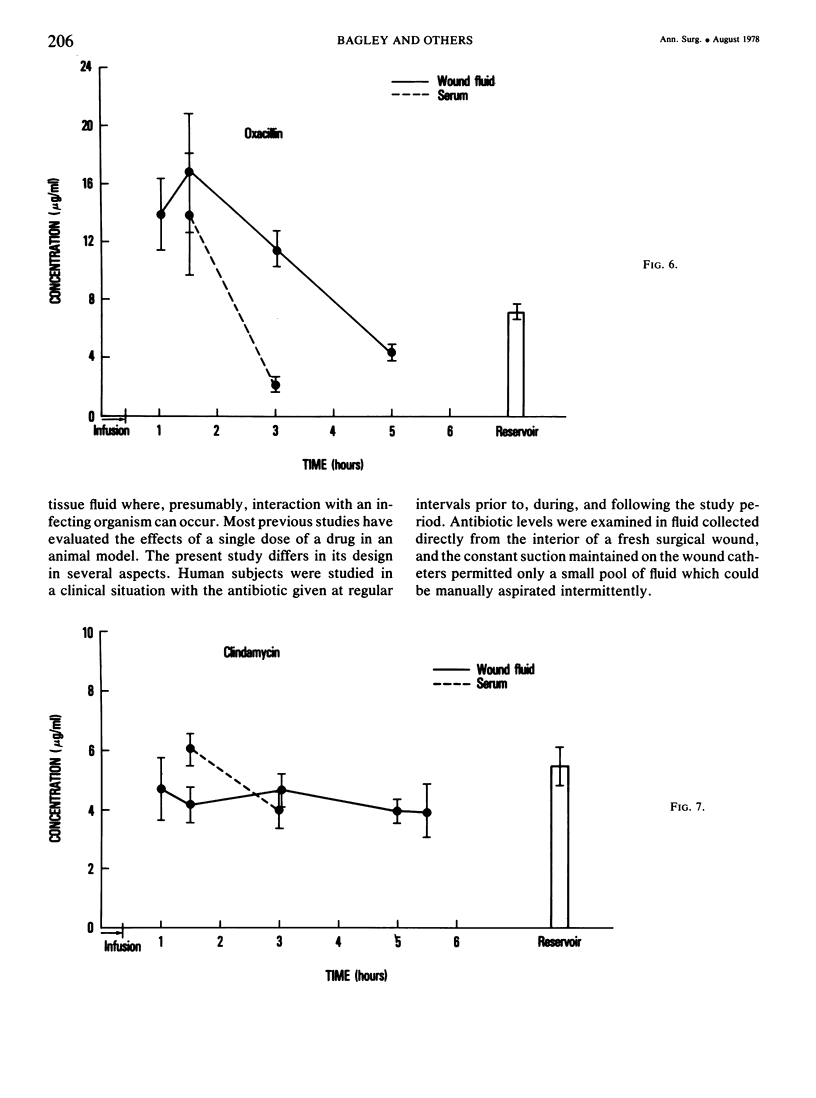
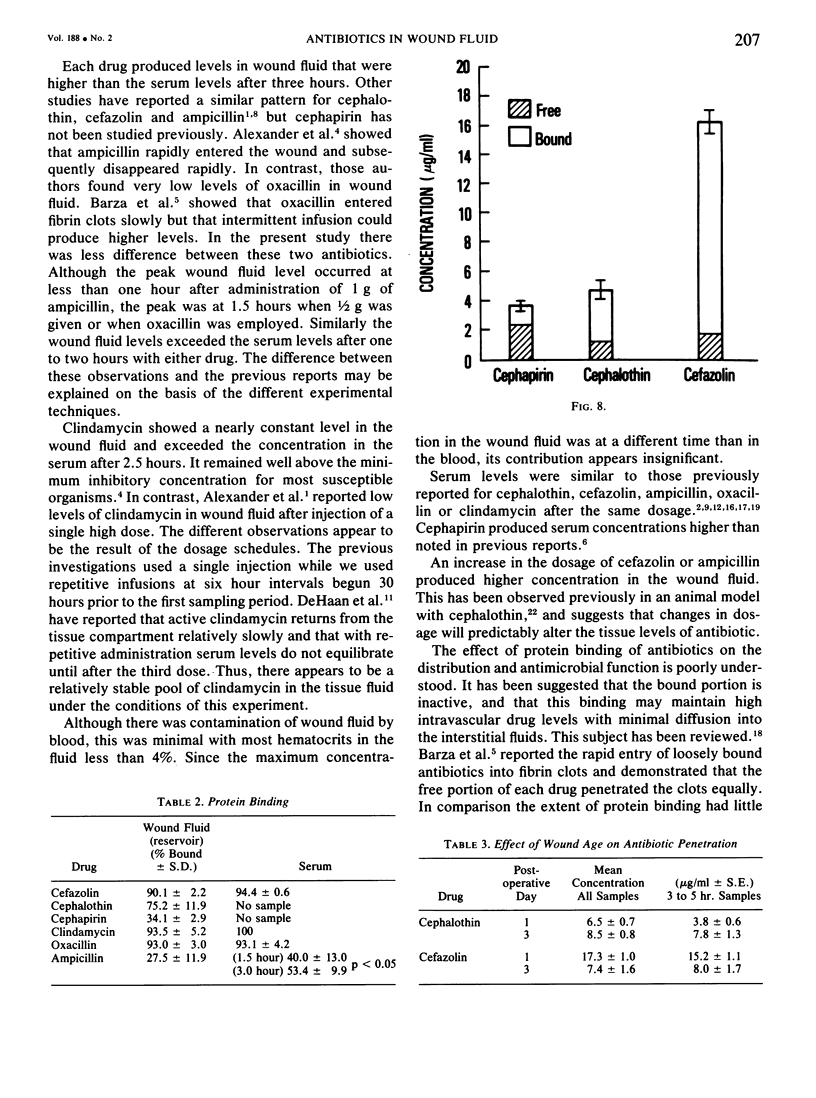
Since the wound is the most common focus of infection in the surgical patient, adequate levels of antibiotic within the wound ar essential. This study examines the concentrations of antibiotic achieved in human wounds. Fluid was collected at timed intervals on the first postoperative day from the wounds of 56 patients receiving antibiotics after regional lymph node dissection. Antibiotic concentration was determined by bioassay. Six antibiotics were studied: cephalothin, cefazolin, cephapirin, oxacillin, ampicillin and clindamycin. The cephalosporins and penicillins showed similar patterns of appearance in the wound fluid. The peak level occurred early (1--1 1/2 hours) with subsequent slow decrease. Clindamycin produced nearly constant levels in wound fluid. The concentration of each antibiotic in wound fluid surpassed the serum levels after 2.5 hours. At the dosages studied each antibiotic produced wound fluid concentrations greater than the MIC for most susceptible organisms. Higher doses provided higher wound fluid levels. The rate of appearance and the levels achieved should be considered in the choice of antibiotics in the surgical subject.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander J. W., Sykes N. S., Mitchell M. M., Fisher M. W. Concentration of selected intravenously administered antibiotics in experimental surgical wounds. J Trauma. 1973 May;13(5):423–434. doi: 10.1097/00005373-197305000-00004. [DOI] [PubMed] [Google Scholar]
- Baker G., Hung T. K. Pencillin concentrations in experimental wounds. Am J Surg. 1968 Apr;115(4):531–534. doi: 10.1016/0002-9610(68)90199-2. [DOI] [PubMed] [Google Scholar]
- Bartlett J. G., Sutter V. L., Finegold S. M. Treatment of anaerobic infections with lincomycin and clindamycin. N Engl J Med. 1972 Nov 16;287(20):1006–1010. doi: 10.1056/NEJM197211162872002. [DOI] [PubMed] [Google Scholar]
- Chisholm D. R., Leitner F., Misiek M., Wright G. E., Price K. E. Laboratory studies with a new cephalosporanic acid derivative. Antimicrob Agents Chemother (Bethesda) 1969;9:244–246. [PubMed] [Google Scholar]
- Chisholm G. D., Waterworth P. M., Calnan J. S., Garrod L. P. Concentration of antibacterial agents in interstitial tissue fluid. Br Med J. 1973 Mar 10;1(5853):569–573. doi: 10.1136/bmj.1.5853.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeHaan R. M., Metzler C. M., Schellenberg D., Vandenbosch W. D. Pharmacokinetic studies of clindamycin phosphate. J Clin Pharmacol. 1973 May-Jun;13(5):190–209. doi: 10.1002/j.1552-4604.1973.tb00208.x. [DOI] [PubMed] [Google Scholar]
- EICKHOFF T. C., KISLAK J. W., FINLAND M. SODIUM AMPICILLIN: ABSORPTION AND EXCRETION OF INTRAMUSCULAR AND INTRAVENOUS DOSES IN NORMAL YOUNG MEN. Am J Med Sci. 1965 Feb;249:163–171. [PubMed] [Google Scholar]
- Fare L. R., Actor P., Sachs C., Phillips L., Joloza M., Pauls J. F., Weisbach J. A. Comparative serum levels and protective activity of parenterally administered cephalosporins in experimental animals. Antimicrob Agents Chemother. 1974 Aug;6(2):150–155. doi: 10.1128/aac.6.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hottendorf G. H., Price K. E., Van Harken D. R. Comparative plasma bactericidal activity of cephapirin and cefazolin. Curr Ther Res Clin Exp. 1975 Aug;18(2):364–370. [PubMed] [Google Scholar]
- KETCHAM A. S., BLOCH J. H., CRAWFORD D. T., LIEBERMAN J. E., SMITH R. R. The role of prophylactic antibiotic therapy in control of staphylococcal infections following cancer surgery. Surg Gynecol Obstet. 1962 Mar;114:345–352. [PubMed] [Google Scholar]
- Kirby W. M., Kind A. C. Clinical pharmacology of ampicillin and hetacillin. Ann N Y Acad Sci. 1967 Sep 27;145(2):291–297. doi: 10.1111/j.1749-6632.1967.tb50226.x. [DOI] [PubMed] [Google Scholar]
- Kunin C. M., Craig W. A., Kornguth M., Monson R. Influence of binding on the pharmacologic activity of antibiotics. Ann N Y Acad Sci. 1973 Nov 26;226:214–224. doi: 10.1111/j.1749-6632.1973.tb20483.x. [DOI] [PubMed] [Google Scholar]
- Nicholas P., Meyers B. R., Hirschman S. Z. Pharmacology of cefazolin in human volunteers. J Clin Pharmacol. 1973 Aug-Sep;13(8):325–331. doi: 10.1002/j.1552-4604.1973.tb00219.x. [DOI] [PubMed] [Google Scholar]
- Tan J. S., Trott A., Phair J. P., Watanakunakorn C. A method for measurement of antibiotics in human interstitial fluid. J Infect Dis. 1972 Nov;126(5):492–497. doi: 10.1093/infdis/126.5.492. [DOI] [PubMed] [Google Scholar]
- Waterman N. G., Kastan L. B. Interstitial fluid and serum antibiotic concentrations. Arch Surg. 1972 Aug;105(2):192–196. doi: 10.1001/archsurg.1972.04180080046008. [DOI] [PubMed] [Google Scholar]