Abstract
Objective To review the characteristics of public-private mix projects in India and their effect on case notification and treatment outcomes for tuberculosis.
Design Literature review.
Data sources Review of surveillance records from Indian tuberculosis programme project, evaluation reports, and medical literature for public-private mix projects in India.
Data extraction Project characteristics, tuberculosis case notification of new patients with sputum smear results positive for acid fast bacilli, and treatment outcome.
Data synthesis Of 24 identified public-private mix projects, data were available from 14 (58%), involving private practitioners, corporations, and non-governmental organisations. In all reviewed projects, the public sector tuberculosis programme provided training and supervision of private providers. Among the five projects with available data on historical controls, case notification rates were higher after implementation of a public-private mix project. Among seven projects involving private practitioners, 2796 of 12 147 (23%) new patients positive for acid fast bacilli were attributed to private providers. Corporate based and non-governmental organisations served as the main source for tuberculosis programme services in seven project areas, detecting 9967 new patients positive for acid fast bacilli. In nine of 12 projects with data on treatment outcomes, private providers exceeded the programme target of 85% treatment success for new patients positive for acid fast bacilli.
Conclusions Public-private mix activities were associated with increased case notification, while maintaining acceptable treatment outcomes. Collaborations between public and private providers of health care hold considerable potential to improve tuberculosis control in India.
Introduction
More cases of tuberculosis occur in India than in any other country in the world. An estimated 1.79 million new cases of tuberculosis and 352 000 tuberculosis related deaths occurred in 2003, representing one fifth of the global burden of incident cases of tuberculosis and mortality.1 The Indian Revised National Tuberculosis Control Programme began large scale nationwide implementation of the World Health Organization's global tuberculosis control strategy (DOTS) in 1998 and has since expanded rapidly. Country-wide coverage is anticipated by April 2006. However, almost half of patients with tuberculosis in India may initially seek help from the private healthcare sectors, where diagnosis, treatment, and reporting practices often do not meet national or international standards for tuberculosis.2-4 Subsequent delays in diagnosis and inadequate treatment may result in extended infectiousness, acquired drug resistance, treatment failure, and high rates of relapse—all of which may impair efforts for tuberculosis control in India. Collaborations between the public and private health sectors, or public-private mix, may be an important solution.
Public-private mix has been defined by WHO as strategies that link all healthcare entities within the private and public sectors (including health providers in other governmental ministries) to national tuberculosis programmes for expansion of DOTS activities.5 Published reports of public-private mix projects indicate that the approach is feasible and effective, but previous evaluations are largely limited to local and individual experiences.6-9 India has the largest collection of such experiences of public-private mix, few of which to date have been reported.10-13 We describe the effect of a series of pilot public-private mix projects in India on case notification of tuberculosis and treatment outcomes and discuss the potential role of public-private mix in improving tuberculosis control in India.
Methods
After early experiences showed the potential value of public-private mix activities,10,14 the Indian Revised National Tuberculosis Control Programme developed formal guidelines to help local programmes structure collaborations with private healthcare providers and non-governmental organisations.15,16 These guidelines offered a diverse group of plans for the community of private providers, with options to participate in the referral, diagnosis, or treatment of patients with tuberculosis. The Indian tuberculosis programme also made financial incentives available for local programmes to distribute to cooperating providers, although these incentives were not always used.
For our review we included all collaborations between the Indian Revised National Tuberculosis Control Programme and private health providers listed in the programme's surveillance records. To allow focus on private practitioners and non-governmental organisations, we excluded collaborations with medical colleges and government health facilities outside the authority of the Indian ministry of health.17 We reviewed only collaborations with non-governmental organisations in which tuberculosis care was delivered to an area with a population of at least 500 000.
For each project the evaluation period was the time frame for which case notification or treatment data were available. These data were collected for each project site in quarterly (three month) increments from the Indian tuberculosis programme surveillance records and WHO public-private mix project evaluation reports. If available we also collected project area case notification data from the Indian tuberculosis programme before the introduction of a public-private mix project. In some areas data on tuberculosis surveillance before the start of a public-private mix project were not available because projects were started from the onset of expansion of the Indian tuberculosis programme into the region. Since patients who are positive for acid fast bacilli on the basis of a sputum smear test are generally considered to be the main source of Mycobacterium tuberculosis transmission, we limited data collection to new cases whose sputum tested positive for acid fast bacilli.
We defined a private sector notified patient as a patient diagnosed as having tuberculosis or referred by the private health sector, who was subsequently recorded (registered) by the Indian tuberculosis programme as a tuberculosis case. All other patients registered as having tuberculosis were defined as public sector notified patients. We defined private provider administered DOT as the administration of directly observed antituberculosis treatment to a patient registered as having tuberculosis by a private health provider (including community volunteers supervised by private providers). Public sector administered DOT was defined as the administration of directly observed antituberculosis treatment to a patient registered as having tuberculosis by the public sector tuberculosis programme. We used standard WHO definitions for treatment outcomes.18 A treatment success was defined as a new patient with sputum positive for acid fast bacilli who achieved cure or completed treatment.
For each public-private mix project we calculated quarterly case notification rates by dividing the number of new case notifications of sputum positive for acid fast bacilli by the estimated population of the project area. To calculate the mean annual case notification rate for each project, quarterly rates were multiplied by 4 and averaged. Population estimates were taken from the 2001 census, or local government estimates if census data were unavailable.
Results
As of February 2004, 24 public-private mix projects met our inclusion criteria (see bmj.com), and we were able to collect data from 14 (58%) of the 24 projects (table 1)—six of eight (75%) collaborations with private practitioners, one of five (20%) collaborations with large corporate based practitioners, and seven of 11 (64%) collaborations with large non-governmental organisations. In all projects, the Indian tuberculosis programme provided training for private providers to synchronise laboratory, diagnostic, and treatment practices with national guidelines. Costs of training were uniformly borne by local or state tuberculosis programmes.
Table 1.
Characteristics of selected public-private mix (PPM) pilot projects in India (as of August 2004)
|
Areas with existing government health infrastructure
|
Areas without government health infrastructure
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Kerala
|
Maharashtra
|
New Delhi
|
Tamil Nadu
|
|||||||||||
| Project characteristic | Delhi LRS (New Delhi) | Kannur | Kollam | Mumbai | Thane | Thane Rural | Mahavir (Andhra Pradesh) | Tea Estates (Assam and West Bengal) | SHIS (West Bengal) | Falah-e-Am (Uttar Pradesh) | NDTB | RK Mission | Leprosy Rural Relief | St Mary's Leprosy |
| Population | 0.1 | 2.4 | 2.6 | 4.0 | 1.2 | 1.6 | 0.5 | 4.6 | 1.2 | 0.5* | 0.2* | 0.6* | 0.5 | 0.5 |
| Primarily urban or rural area served by project | Urban | Mixed | Mixed | Urban | Urban | Rural | Mixed | Rural | Rural | Urban | Urban | Urban | Rural | Urban |
| Supplemental funding | GOI | No | No | WHO | No | No | No | No | No | No | No | No | No | No |
| Third party coordinating organisation | DMA | None | IMA | NGO | None | None | None | ITA | None | None | None | None | None | None |
| No of collaborating private providers: | ||||||||||||||
| Referring private providers | Unknown | Unknown | Unknown | 1018 | 95 | 94 | 334 | 226 | 35 | Unknown | Unknown | Unknown | 15 | 21 |
| Microscopy centres | 3 | 31 | 25 | 0 | 2 | 1 | 6 | 3 | 5 | 1 | 1 | 1 | 1 | 1 |
| DOTS treatment providers | 3 | 33 | Unknown | 192 | 98 | 138 | 36 | 222 | 625 | 2 | Unknown | Unknown | 400 | 493 |
| Medical colleges | 0 | 1 | 0 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Service charges to patients by private providers: | ||||||||||||||
| Sputum acid fast bacilli microscopy | Free | Charge | Charge | Free | Charge | Charge | Free | Free | Free | Free | Free | Free | Free | Free |
| Drugs for DOTS treatment | Free | Free | Free | Free | Free | Free | Free | Free | Free | Free | Free | Free | Free | Free |
| Primary supervision of private providers: | ||||||||||||||
| Private microscopy centres
|
RNTCP and DMA
|
RNTCP
|
RNTCP
|
RNTCP
|
RNTCPRNTCP
|
NGO and private providers
|
RNTCP
|
NGO
|
NGO
|
NGO
|
NGO
|
NGO
|
NGO
|
|
| PPM DOTS treatment providers | RNTCP and DMA | RNTCP | RNTCP | RNTCP and NGO | RNTCPRNTCP | NGO and private providers | Corporate and private providers | NGO | NGO | RNTCP and NGO | NGO | RNTCP and NGO | RNTCP and NGO | |
Population in millions according to 2000 census.
LRS=Lala Ram Sarup Institute of Tuberculosis and Respiratory Diseases; SHIS=Southern Health Improvement Samity; NDTB=New Delhi Tuberculosis Centre; RK=Ramakrishanan; RNTCP=Revised National Tuberculosis Control Programme; NGO=non-governmental organisation; DMA=Delhi Medical Association; IMA=Indian Medical Association; ITA=Indian Tea Association; GOI=Government of India.
Estimated.
The public-private mix projects used a variety of methods to link the Indian tuberculosis programme and private providers. Projects in Kannur and Kollam (Kerala) provided training and support for private laboratories and encouraged referral of patients with sputum smears positive for acid fast bacilli to public sector facilities for treatment.19 Other projects relied on private providers to refer patients with suspected tuberculosis to public sector facilities for smear microscopy. In 10 (71%) of the 14 reviewed projects, private laboratories provided free smear microscopy, and the Indian tuberculosis programme partially reimbursed these laboratories by providing free slides and reagents. Professional societies, such as the Indian Medical Association, were also essential partners in bringing together public and private providers.
Although patients were generally referred to the public sector for treatment, private providers sometimes acted as treatment providers. Treatment providers were responsible for administering directly observed treatment regimens (intermittent dosing, three times a week) supplied by the Indian tuberculosis programme. Staff of the Indian tuberculosis programme routinely supervised all treatment providers, and programme staff were responsible for attempts to restart tuberculosis treatment among patients who interrupted therapy.
Contribution of public-private mix projects to case notification under DOTS
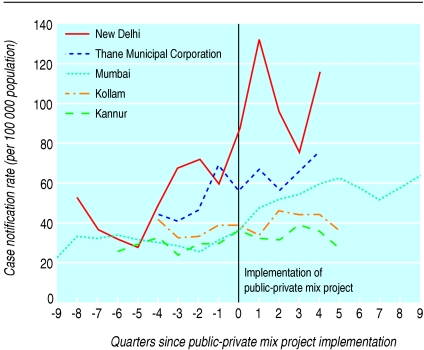
The six public-private mix projects that primarily involved private practitioners were evaluated for a median of 18 months (range 15-30 months). During this time, 10 985 new cases of tuberculosis on the basis of sputum smears positive for acid fast bacilli were reported in the project areas, of which 1631 (15%) were from the private sector (table 2). This represented 2-26% of case notifications for each of those individual projects. In each of the five projects involving private practitioners with data available from before and after implementation of a public-private mix project, the average quarterly number of positive case notifications increased by between 12% and 98% after initiation of the project (figure).
Table 2.
New case notifications of tuberculosis on basis of sputum smears positive for acid fast bacilli among public-private mix pilot projects in India, 1999-2004
|
Before public-private mix project
|
After public-private mix project
|
Public-private mix contribution to case notification in project areas
|
|||||
|---|---|---|---|---|---|---|---|
| Public-private mix project (state) | Evaluation period | Mean (95% CI) tuberculosis case notification rate* | Evaluation period | Mean (95% CI) tuberculosis case notification rate* | % change in mean case notification rate | Total No of new case notifications | No (%) of new case notifications from private sector |
| Private practitioners | |||||||
| Delhi LRS (New Delhi) | Jan 1999 to Dec 2000 | 51.3 (34.8 to 64.2) | Jan 2001 to Mar 2002 | 101.6 (83.0 to 120) | 98.0 | 127 | 28 (22) |
| Kannur (Kerala) | Jan 2000 to Jun 2001 | 28.3 (25.0 to 31.7) | July 2001 to Dec 2002 | 33.8 (30.5 to 37.1) | 19.4 | 1225 | 307 (25) |
| Kollam (Kerala) | Jul 2001 to Jun 2002 | 36.6 (31.0 to 42.2) | July 2002 to Dec 2003 | 41.0 (36.4 to 45.5) | 11.9 | 1588 | 264 (17) |
| Mumbai (Maharashtra) | Jan 1999 to Jun 2001 | 29.7 (25.3 to 34.1) | July 2001 to Dec 2003 | 54.3 (50.1 to 58.5) | 82.7 | 3544 | 910 (26) |
| Thane Municipal (Maharashtra) | Jan to Dec 2001 | 50.5 (38.3 to 62.7) | Jan 2002 to Mar 2003 | 64.7 (53.9 to 75.6) | 28.0 | 971 | 61 (6) |
| Thane Rural (Maharashtra) | NA† | Jul 2001 to Jun 2003 | 41.6 (31.0 to 46.0) | NA | 3530 | 64 (2) | |
| Corporate and non-governmental organisation | |||||||
| Mahavir (Andhra Pradesh) | NA† | Jan 1999 to Dec 2003 | 46.5 (41.8 to 51.2) | NA | 1162 | 1162 | |
| Tea Estates (Assam and West Bengal) | NA† | Jan 2001 to Jun 2003 | 66.6 (58.0 to 72.7) | NA | 3327 | 3327 | |
| SHIS (West Bengal) | NA† | Jul 2003 to Mar 2004 | 31.6 (24.5 to 38.8) | NA | 285 | 285 | |
| Falah-e-Am (Uttar Pradesh) | NA† | Jan 2001 to Jun 2003 | 101.6 (79.1 to 124.1) | NA | 1270 | 1270 | |
| NDTB (New Delhi) | NA† | Jan 1999 to Dec 2003 | 105.8 (88.0 to 123.6) | NA | 1058 | 1058 | |
| RK Mission (New Delhi) | NA† | Jan 1999 to Dec 2003 | 80.6 (73.5 to 87.7) | NA | 2417 | 2417 | |
| Leprosy Rural Relief (Tamil Nadu) | NA† | Oct 2000 to Dec 2003 | 42.1 (34.1 to 50.2) | NA | 722 | 722 | |
| St Mary's Leprosy (Tamil Nadu) | NA† | Jul 2000 to Dec 2003 | 44.7 (41.2 to 54.5) | NA | 888 | 888 | |
NA=not available. See table 1 for other definitions.
Mean annual case notification rate over evaluation period.
Tuberculosis surveillance data not available before public-private mix evaluation period, as local Indian tuberculosis programme not yet implemented.
Figure 1.
Tuberculosis case notification rate before and after implementation of public-private mix project, for collaborations with private practitioners in India, 1999-2004. Projects represented are those with data available before implementation of public-private mix project
The eight public-private mix projects that involved collaborating partners from the corporate sector or non-governmental organisations were evaluated for a median of 30 months (range 9-48 months). During this time 11 129 new cases positive for acid fast bacilli were notified in these areas. Since public-private mix projects were the sole source of Indian tuberculosis programme services here, all case notifications were attributed to the private sector. As local data for tuberculosis surveillance were not available before these projects, no comparison could be made between notification rates before the start of the project.
Treatment outcomes with private provider administered directly observed treatment
In nine (75%) of 12 public-private mix projects with available data on treatment outcome, private provider administered directly observed treatment met or exceeded the Indian tuberculosis programme target of 85% treatment success (table 3). In two projects where treatment outcomes of public sector administered and private provider administered directly observed treatment were compared, no significant differences were found.12,19
Table 3.
Treatment outcomes of new patients with sputum smear positive for acid fast bacilli treated by private practitioner administered directly observed treatment in public-private mix pilot projects, India 2000-02
| Public-private mix project (state) | Evaluation period* | Total No of new case notifications | Cured (%) | Completed treatment (%) | Died (%) | Failed treatment (%) | Defaulted (%) | Transferred (%) | Treatment success (%)† |
|---|---|---|---|---|---|---|---|---|---|
| Private practitioners | |||||||||
| Delhi LRS (New Dehli) | Jan to Mar 2001 | 20 | 18 (90) | 0 | 0 | 1 (5) | 1 (5) | 0 | 90 |
| Kannur (Kerala) | Jan 2001 to Jun 2002 | 85 | 78 (92) | 0 | 2 (2) | 1 (1) | 4 (5) | 0 | 92 |
| Mumbai (Maharashtra) | Apr to Dec 2002 | 296 | 181 (61) | 58 (20) | 7 (2) | 15 (5) | 35 (12) | 0 | 81 |
| Thane Municipal (Maharashtra) | Jan 2001 to Mar 2002 | 215 | 168 (78) | 0 | 10 (5) | 14 (7) | 22 (10) | 1 (0) | 78 |
| Thane Rural (Maharashtra) | Jul 2001 to Jun 2002 | 63 | 55 (87) | 0 | 4 (6) | 0 (0) | 3 (5) | 1 (2) | 87 |
| Corporate and non-governmental organisation | |||||||||
| Mahavir (Andhra Pradesh) | Jan 1995 to Dec 1999 | 161 | 143 (89) | 1 (0) | 3 (2) | 6 (4) | 8 (5) | 0 | 90 |
| Tea Estates (Assam and West Bengal) | Jan 2001 to Mar 2002 | 1925 | 1604 (83) | 17 (1) | 126 (7) | 99 (5) | 77 (4) | 2 (0) | 84 |
| Falah-e-Am (Uttar Pradesh) | Jul 2001 to Jun 2002 | 1040 | 979 (94) | 4 (0) | 26 (3) | 2 (0) | 30 (3) | 0 | 94 |
| NDTB (New Dehli) | Jan 1999 to Dec 2001 | 584 | 508 (87) | 1 (0) | 14 (2) | 29 (5) | 28 (5) | 4 (1) | 87 |
| RK Mission (New Delhi) | Jan 1999 to Dec 2001 | 1429 | 1217 85) | 0 | 40 (3) | 64 (4) | 68 (5) | 40 (3) | 85 |
| Leprosy Rural (Tamil Nadu) | Jul 2000 to Dec 2002 | 472 | 420 (89) | 0 | 28 (6) | 16 (3) | 4 (1) | 4 (1) | 89 |
| St Mary's Leprosy (Tamil Nadu) | Jul 2000 to Dec 2002 | 623 | 514 (82) | 49 (8) | 51 (8) | 4 (1) | 4 (1) | 0 | 91 |
See table 1 for definitions.
Patients included if notification as case of tuberculosis and initiation of treatment occurred in specified evaluation period.
Proportion of patients documented as cured or completed treatment.
Discussion
Collaboration between the Indian Revised National Tuberculosis Control Programme and private practitioners in India improved the case notification of tuberculosis while maintaining good treatment outcomes. Compared with historical surveillance data from the same project areas in a limited number of projects involving private practitioners, higher mean case notification rates were observed after implementation of the public-private mix project. Furthermore, limited data from non-governmental organisations and private industry medical services showed their ability to work with the Indian tuberculosis control programme and successfully diagnose and treat large numbers of patients with tuberculosis. A strong public sector tuberculosis control programme proved critical for provision of necessary advocacy, training, and supervision. These findings highlight the feasibility of building public-private collaborations and the considerable potential they hold for improving tuberculosis control in India.
Concomitant efforts by the Indian tuberculosis programme to increase case detection through educational campaigns and improvement of public sector clinical services likely also played a part. Indeed, national case notification rates from areas without public-private mix projects increased over the same general period as the evaluated projects, as would be expected in the setting of an expanding tuberculosis programme making active efforts to improve case detection. Even accounting for this limitation, to the Indian tuberculosis programme the benefits of public-private mix have proved sufficiently substantive to warrant inclusion into the overall Indian tuberculosis control strategy.
Local tuberculosis programmes made substantial investments in the training and supervision of private providers. These investments may be justified, as recent economic analyses of public-private mix projects in Hyderabad and New Delhi support the perception that public-private mix is cost effective.20 Furthermore, public-private mix reduces treatment costs for patients, as drugs are provided free of charge by the Indian tuberculosis programme. Programmes should, however, avoid diverting resources from public sector tuberculosis control for public-private mix, as any erosion in effectiveness from public sector tuberculosis control might neutralise the positive benefits of public-private mix activities.
As a result of India's active engagement with these public-private mix projects, the scene is set for a broad scale-up of public-private mix into routine practice for tuberculosis programmes. Policies and operational guidelines are in place to guide local programmes and private providers in implementing such public-private mix activities. At the central government level, the Indian tuberculosis programme has pursued and formalised agreements with other large government institutions. The programme has also sponsored national workshops and developed specific procedures for collaboration with medical colleges, which treat large numbers of patients with tuberculosis and play a crucial part in the management of complicated cases.17 Consensus recommendations have been developed for the management of tuberculosis in adults and children in partnership with professional societies, medical colleges, and international experts.21,22 Urban areas tend to have large numbers of private providers and hence are being targeted for intensified public-private mix scale-up. Plans are under way for expansion and replication of strategies associated with sustained success.
Tuberculosis programmes should recognise public-private mix as a public health intervention within their control mandate and engage both public and private healthcare providers to ensure equitable availability of services.23 Providers who treat patients with tuberculosis should recognise that they have a responsibility to patients and their communities to adhere to standards of care, including prompt and accurate diagnosis, reporting, and effective treatment in accordance with DOTS.24 Furthermore, coalitions with third party coordinating organisations may also promote ongoing involvement of the community; here public-private mix projects using third party interface organisations showed particularly large contributions to tuberculosis case detection.
The diverse public-private mix projects we describe highlight the feasibility and challenges of implementing public-private collaboration in tuberculosis control. Similarly, these public-private mix concepts could be applied to other diseases of public health importance, including HIV and malaria, which increasingly require linkages between governments, private providers, and community based organisations. The lessons of Indian public-private mix projects have been and continue to be instrumental in shaping the global agenda for public-private mix activities in DOTS expansion, and may accelerate the achievement of goals for global tuberculosis control.
What is already known on this topic
India has almost one fifth of the world's burden of tuberculosis, and as many as half of patients with tuberculosis see private providers first
Collaboration between public tuberculosis programmes and private healthcare sectors is an important strategy to ensure equitable access to quality tuberculosis diagnosis, treatment, and care
What this study adds
In a series of pilot projects in India, tuberculosis case notification improved after implementation of public-private collaboration
The Indian tuberculosis programme is scaling up efforts to collaborate with private providers and improve access to directly observed treatment, particularly in urban areas
Supplementary Material
 Projects are listed on bmj.com
Projects are listed on bmj.com
RG is technical adviser and programme officer for the Office of the US Global AIDS Coordinator, Washington DC, USA.
Contributors: All authors developed the idea for this article. PD produced the first draft of the article, and all authors prepared the final draft. PD is guarantor.
Funding: None.
Competing interests: KL and MU work with the public-private mix for DOTS initiative in the WHO's Stop TB Department.
Ethical approval: Not required.
Amendment
This is Version 2 of the paper. In this version Dr Chauhan's first name has been correctly spelt as Lakhbir [not Lakbir as in previous version].
References
- 1.World Health Organization. Global tuberculosis control 2005: surveillance, planning, financing. Geneva: WHO, 2005. Report No WHO/HTM/TB/2005.349. www.who.int/entity/tb/publications/global_report/2005/pdf/Full.pdf (accessed 1 Oct 2005).
- 2.Prasad R, Nautiyal RG, Mukherji PK, Jain A, Singh K, Ahuja RC. Treatment of new pulmonary tuberculosis patients: what do allopathic doctors do in India? Int J Tuberc Lung Dis 2002;6: 895-902. [PubMed] [Google Scholar]
- 3.Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis 1998;2: 324-9. [PubMed] [Google Scholar]
- 4.World Health Organization. The behaviour and interaction of TB patients and private for-profit health care providers in India: a review. Geneva: WHO, 1997. Report No WHO/TB/97.223. http://whqlibdoc.who.int/hq/1997/WHO_TB_97.223.pdf (accessed 11 Jan 2005).
- 5.World Health Organization. Public-private mix for DOTS: report of the second meeting of the PPM subgroup for DOTS expansion. Geneva: WHO; 2004. Report No WHO/HTM/TB/2004.338. http://whqlibdoc.who.int/hq/2004/WHO_HTM_TB_2004.338.pdf (accessed 11 Jan 2005).
- 6.Klein SJ, Naizby BE. Creation of a tuberculosis directly observed therapy provider network in New York City: a new model of public health. J Public Health Manag Pract 1995;1: 1-6. [PubMed] [Google Scholar]
- 7.Quy HT, Lan NT, Lonnroth K, Buu TN, Dieu TT, Hai LT. Public-private mix for improved TB control in Ho Chi Minh city, Vietnam: an assessment of its impact on case detection. Int J Tuberc Lung Dis 2003;7: 464-71. [PubMed] [Google Scholar]
- 8.Newell JN, Pande SB, Baral SC, Bam DS, Malla P. Control of tuberculosis in an urban setting in Nepal: public-private partnership. Bull World Health Organ 2004;82: 92-8. [PMC free article] [PubMed] [Google Scholar]
- 9.Mantala MJ. Public-private mix DOTS in the Philippines. Tuberculosis (Edinb) 2003;83: 173-6. [DOI] [PubMed] [Google Scholar]
- 10.Murthy KJ, Frieden TR, Yazdani A, Hreshikesh P. Public-private partnership in tuberculosis control: experience in Hyderabad, India. Int J Tuberc Lung Dis 2001;5: 354-9. [PubMed] [Google Scholar]
- 11.Rangan SG, Juvekar SK, Rasalpurkar SB, Morankar SN, Joshi AN, Porter JD. Tuberculosis control in rural India: lessons from public-private collaboration. Int J Tuberc Lung Dis 2004;8: 552-9. [PubMed] [Google Scholar]
- 12.Arora VK, Lonnroth K, Sarin R. Improved case detection of tuberculosis through a public-private partnership. Indian J Chest Dis Allied Sci 2004;46: 1-17. [PubMed] [Google Scholar]
- 13.Ambe G, Lonnroth K, Dholakia Y, Copreaux J, Zignol M, Borremans N, et al. Every provider counts: effect of a comprehensive public-private mix approach for TB control in a large metropolitan area in India. Int J Tuberc Lung Dis 2005;9: 562-8. [PubMed] [Google Scholar]
- 14.Uplekar MW, Rangan S. Private doctors and tuberculosis control in India. Tuber Lung Dis 1993;74: 332-7. [DOI] [PubMed] [Google Scholar]
- 15.Government of India. Involvement of non-governmental organizations in the revised national tuberculosis programme. New Delhi: Central Tuberculosis Division, Government of India, 1998. www.tbcindia.org/ngo.pdf (accessed 11 Jan 2005).
- 16.Government of India. Involvement of private practitioners in the revised national tuberculosis programme. New Delhi: Central Tuberculosis Division, Government of India; 2002. www.tbcindia.org/Private%20Practitioners.pdf (accessed 11 Jan 2005).
- 17.Tonsing J, Mandal PP. Medical colleges' involvement in the RNTCP: current status. J Indian Med Assoc 2003;101: 164-6. [PubMed] [Google Scholar]
- 18.World Health Organization. Treatment of tuberculosis: guidelines for national programmes. 3rd ed. Geneva: WHO; 2003. Report No WHO/CDS/TB/2003.313. www.who.int/docstore/gtb/publications/ttgnp/PDF/2003.313.pdf (accessed 11 Jan 2005).
- 19.Kumar MK, Dewan PK, Nair PK, Frieden TR, Sahu S, Wares F, et al. Improved tuberculosis case detection through public-private partnership and laboratory-based surveillance, Kannur District, Kerala, India, 2001-2002. Int J Tuberc Lung Dis 2005;9: 870-6. [PubMed] [Google Scholar]
- 20.Floyd K. Cost and cost-effectiveness of public-private mix DOTS: evidence from two pilot projects in India. Geneva: WHO, 2004. Report No WHO/HTM/TB/2004.337. http://whqlibdoc.who.int/hq/2004/WHO_HTM_TB_2004.337.pdf (accessed 11 Jan, 2005).
- 21.Government of India. Management of pediatric TB under the Revised National Tuberculosis Control Programme (RNTCP): a joint statement of the Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, and experts from Indian Academy of Pediatrics. New Delhi, India: Central Tuberculosis Division, Government of India, 2003. www.tbcindia.org/ (accessed 11 Jan 2005).
- 22.Government of India. Recommendations: second meeting of the national task force for involvement of medical colleges in the RNTCP, New Delhi, 22 Nov 2003. New Delhi, India: Central Tuberculosis Division, Government of India, 2003. www.tbcindia.org/Recomm%202nd%20NTF%20ws%20Nov03%20FINAL.pdf (accessed 11 Jan 2005).
- 23.Lonnroth K, Uplekar M, Arora VK, Juvekar S, Lan NT, Mwaniki D, et al. Public-private mix for DOTS implementation: what makes it work? Bull World Health Organ 2004;82: 580-6. [PMC free article] [PubMed] [Google Scholar]
- 24.Hopewell PC, Pai M. Tuberculosis, vulnerability, and access to quality care. JAMA 2005;293: 2790-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.