Abstract
Objective:
The objective of this study was to investigate the effect of American College of Surgeons (ACS) trauma center designation and trauma volume on outcome in patients with specific severe injuries.
Background:
Trauma centers are designated by the ACS into different levels on the basis of resources, trauma volume, and educational and research commitment. The criteria for trauma center designation are arbitrary and have never been validated.
Methods:
The National Trauma Data Bank study, which included patients >14 years of age and had injury severity score (ISS) >15, were alive on admission and had at least one of the following severe injuries: aortic, vena cava, iliac vessels, cardiac, grade IV/V liver injuries, quadriplegia, or complex pelvic fractures. Outcomes (mortality, intensive care unit stay, and severe disability at discharge) were compared among level I and II trauma centers and between centers within the same level designation but different volumes of severe trauma (<240 vs ≥240 trauma admissions with ISS >15 per year). The outcomes were adjusted for age (<65 ≥65), gender, mechanism of injury, hypotension on admission, and ISS (≤25 and >25).
Results:
A total of 12,254 patients met the inclusion criteria. Overall, level I centers had significantly lower mortality (25.3% vs 29.3%; adjusted odds ratio [OR], 0.81; 95% confidence interval [CI], 0.71–0.94; P = 0.004) and significantly lower severe disability at discharge (20.3% vs 33.8%, adjusted OR, 0.55; 95% CI, 0.44–0.69; P < 0.001) than level II centers. Subgroup analysis showed that cardiovascular injuries (N = 2004) and grades IV–V liver injuries (N = 1415) had a significantly better survival in level I than level II trauma centers (adjusted P = 0.017 and 0.023, respectively). Overall, there was a significantly better functional outcome in level I centers (adjusted P < 0.001). Subgroup analysis showed level I centers had significantly better functional outcomes in complex pelvic fractures (P < 0.001) and a trend toward better outcomes in the rest of the subgroups. The volume of trauma admissions with ISS >15 (<240 vs ≥240 cases per year) had no effect on outcome in either level I or II centers.
Conclusions:
Level I trauma centers have better outcomes than lower-level centers in patients with specific injuries associated with high mortality and poor functional outcomes. The volume of major trauma admissions does not influence outcome in either level I or II centers. These findings may have significant implications in the planning of trauma systems and the billing of services according to level of accreditation.
American College of Surgeons designated level I trauma centers had significantly better survival and functional outcomes than level II centers. The volume of severe trauma admissions (<240 or ≥240 patients with Injury Severity Score >15 per year) did not influence outcomes.
Trauma centers are designated by the American College of Surgeons (ACS) into one of 4 levels on the basis of resources, trauma volume, and educational and research commitment. The criteria for trauma center designation are arbitrary and have never been validated. The purpose of the present study is to compare outcomes between the various levels centers and validate trauma volume as a criterion for level I center designation.
PATIENTS AND METHODS
Data for this study was obtained from the National Trauma Data Bank (NTDB), which is maintained by the American College of Surgeons. This ongoing project represents the largest trauma registry ever assembled and currently contains over one million prospectively collected patient records. The database contains information on patient demographics, prehospital care, diagnoses and injury severity scoring, inpatient care and complications, as well as outcomes.
In addition to the patient-specific data, information for each admission was collected regarding the treating hospital. The ACS trauma level designation for each facility was categorized as level I, level II, or other. The number of admissions of patients with an ISS greater than 15 per year was also collected for each participating center.
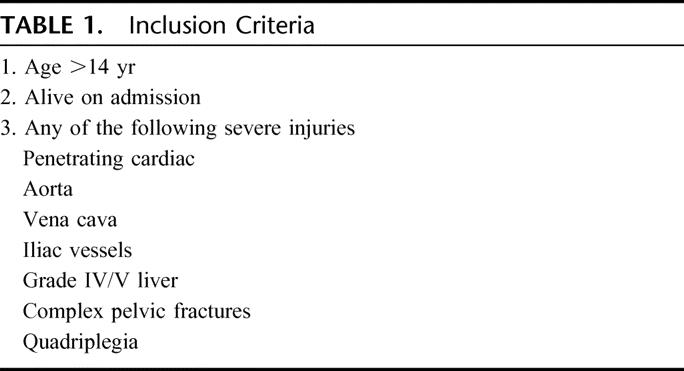
The study included trauma patients older than 14 years of age who were alive on admission to the hospital and had at least one of the following severe injuries: aortic, vena cava, iliac vessels, grade IV/V liver injuries, penetrating cardiac injuries, quadriplegia, or complex pelvic fractures (Table 1) during the period 1996 through 2003. The following data were included in a computerized spreadsheet and analyzed using SPSS 12.0 Windows (SPSS Inc, Chicago, Illinois) for the purpose of the study: age; gender; mechanism of injury (blunt or penetrating); hypotension on admission (systolic blood pressure ≤90 mm Hg or >90 mm Hg); abbreviated injury score (AIS) for head, chest, abdomen, and extremities; injury severity score (ISS); severe liver trauma (International Classification of Diseases, 9th Revision codes 864.04, 864.09, 864.14, 864.19); penetrating cardiac injuries (861.03, 861.12); aortic injuries (901.0, 902.0); vena cava injuries (901.2, 902.0); iliac vascular injuries (902.53, 902.54, 902.50); quadriplegia (806.01, 806.06, 806.11, 806.16); and complex pelvic fractures (808.43, 808.53).
TABLE 1. Inclusion Criteria
Outcomes (mortality, intensive care unit stay, and severe disability at discharge) were compared among level I and II trauma centers and among centers within the same level designation but different volumes of severe trauma (<240 versus ≥240 trauma admissions with ISS >15 per year). The degree of functional disability among survivors at discharge was assessed using the functional independence measure (FIM) score. This rating system evaluates the degree of functional disability in 3 major areas: feeding, locomotion, and expression. Patients are given a score for each area ranging from one (requires total assistance) to 4 (able to perform activity independently). The total FIM score is the sum of the scores for the 3 areas with a maximum possible score of 12 indicating complete functional independence at discharge. For the purposes of the study, we defined severe functional disability as a total FIM score (FIMtot) of less than 9. The outcomes were adjusted for age (<65 and ≥65 years), gender, mechanism, hypotension on admission, and ISS (≤25 and >25). Univariate statistical analysis was performed using the unpaired Student t test or Mann-Whitney rank-sum test for continuous variables and chi-squared with Yates correction for categorical variables. Univariate analysis was performed, which included age, gender, mechanism of injury, first Glasgow Coma score, first systolic blood pressure, first respiratory rate (assisted or unassisted), ISS, and AIS scores for head, chest, abdomen, and extremity. Those variables with P value <0.2 were entered into the multivariate analysis. Multivariate logistic regression models were created to examine the effect of ACS designation on mortality after adjusting for the following variables, which were identified after the univariate analysis: age, gender, injury mechanism (blunt or penetrating), injury severity score, and hypotension on admission (systolic blood pressure <90 mm Hg). Adjusted odds ratios with 95% confidence intervals were calculated from the regression analysis and statistical significance was set at P < 0.05.
RESULTS
Epidemiologic Characteristics
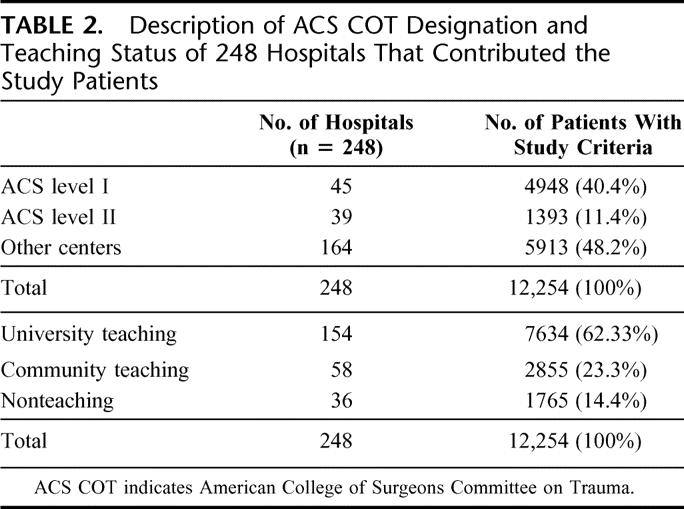
The NTDB included 1,130,093 trauma patients, 12,254 (1.1%) of whom were older than 14 years, had at least one of the severe injuries required in the inclusion criteria, and were alive on admission. These 12,254 cases formed the basis of the present study. Table 2 shows the description of the 248 hospitals that contributed the cases according to ACS designation and teaching status. Overall, 48 level I and II trauma centers admitted 240 or more patients with ISS >15 per year. The rest of the centers admitted fewer than 240 patients with severe trauma (ISS ≤15) per year.
TABLE 2. Description of ACS COT Designation and Teaching Status of 248 Hospitals That Contributed the Study Patients
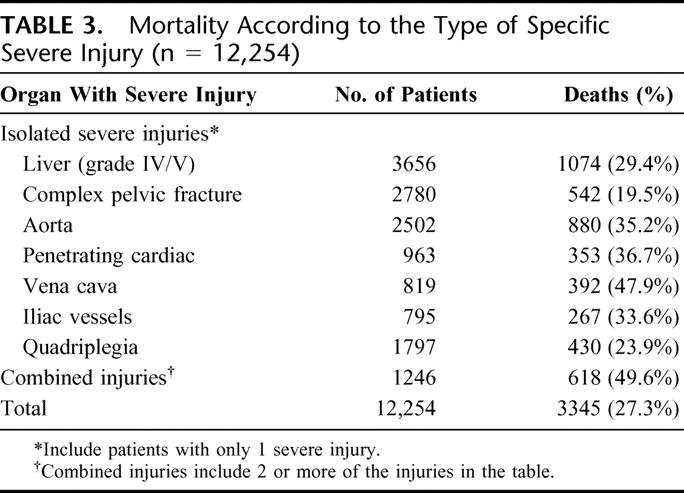
Overall, blunt trauma accounted for 9313 (76%) and penetrating trauma for 2941 (24%) of the cases included in the study. Grade IV/V liver injuries were the most common severe injuries, followed by complex pelvic fractures and aortic injuries. Approximately 10% of the study cases had more than one severe injury (Table 3).
TABLE 3. Mortality According to the Type of Specific Severe Injury (n = 12,254)
Approximately half of the study patients (5882 or 48%) were taken from the emergency room to the operating room, 37% (4534 patients) were dispositioned to the intensive care unit, and 3% (368 patients) died in the emergency room. The remaining 12% (1470 patients) were dispositioned to other areas or centers.
Overall Outcomes
The overall mortality was 27.3% (3345 deaths). The mortality according to specific severe organ injury is shown in Table 3. The highest mortality occurred in patients with vena cava injuries (47.9%), followed by penetrating cardiac injuries (36.7%) and aortic injuries (35.2%). Details of the mortalities by organ injury are shown in Table 3. The overall mean hospital stay was 16.2 ± 21.1 day, the intensive care unit stay 8.8 ± 13.8 days, and ventilator days 14.3 ± 52.
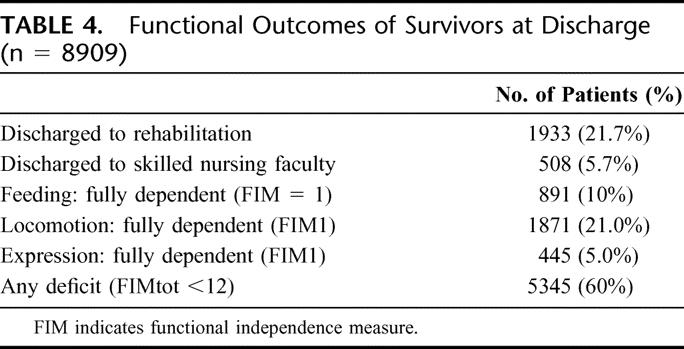
Overall, 21.7% of survivors (1933) were discharged to a rehabilitation facility and 5.7% (508) to a skilled nursing facility. Details of functional outcomes on discharge are shown in (Table 4).
TABLE 4. Functional Outcomes of Survivors at Discharge (n = 8909)
Outcomes According to Level of Trauma Center Designation
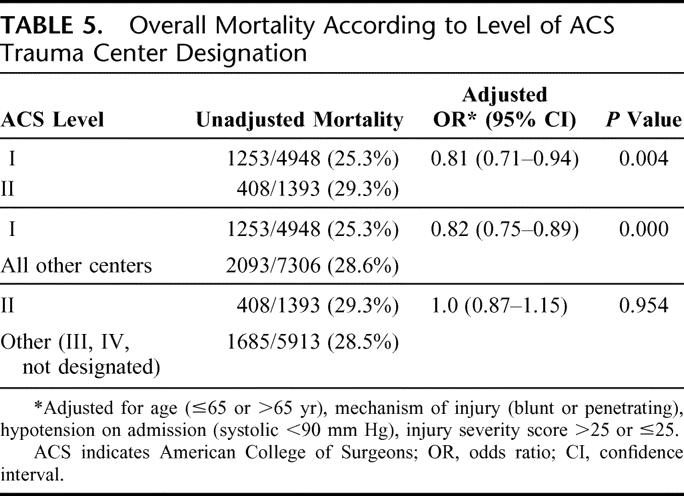
There were 4948 patients treated in level I centers and the overall mortality was 25.3%. Level II centers treated 1393 patients with an overall mortality was 29.3%. The remaining 5913 patients were treated in level III or IV centers or non-ACS-designated trauma centers and the mortality was 28.6%. Multivariate analysis adjusting for age (≤65 and >65 years), mechanism of injury (blunt and penetrating), hypotension on admission (systolic pressure <90 mm Hg), and ISS >25 showed that the adjusted mortality in level I trauma centers was significantly lower than in level II trauma centers (adjusted odds ratio [OR], 0.81; 95% confidence interval [CI], 0.71–0.94; P = 0.004) or all other centers (levels II, III, IV, nondesignated) (adjusted OR, 0.82; 95% CI, 0.75–0.89; P = 0.000). Comparison between level II with lower-level or nondesignated centers showed no difference in survival outcome (adjusted OR, 1.0; 95% CI, 0.87–1.15; P = 0.954) (Table 5).
TABLE 5. Overall Mortality According to Level of ACS Trauma Center Designation
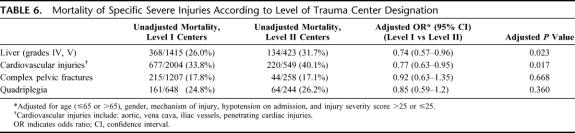
The mortality of specific injuries according to ACS trauma center designation (level I or II) is shown in Table 6. Patients with severe liver injuries (grades IV–V) or cardiovascular injuries had a significantly better survival if treated in level I centers than level II centers (adjusted P values 0.023 and 0.017, respectively). There was no difference in survival of patients with quadriplegia or complex pelvic fractures between level I and II centers (Table 6).
TABLE 6. Mortality of Specific Severe Injuries According to Level of Trauma Center Designation
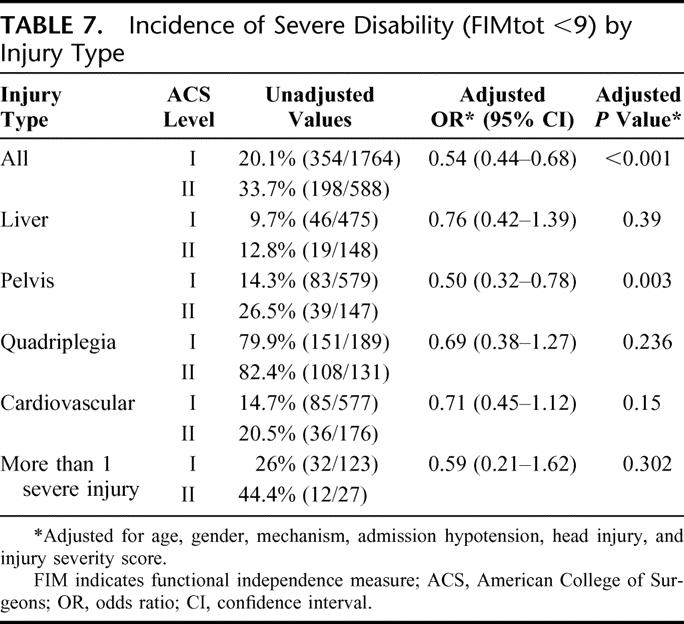
Overall, level I centers had significantly better functional outcomes at discharge. The overall incidence of severe disability (FIM tot <9 [FIM tot: total functional independence]) in survivors was 20.3% in level I centers and 33.8% in level II centers (adjusted OR, 0.54; 95% CI, 0.44–0.68; P < 0.001). There was a trend for better functional outcome in level I centers in all subgroups of specific injuries, reaching statistical significance in complex pelvic fractures (adjusted OR, 0.50; 95% CI, 0.32–0.78; P = 0.003) (Table 7). The intensive care unit length of stay was 9.1 ± 14.5 days for level I and 9.3 ± 13.5 days for level II centers (adjusted OR, −0.03; 95% CI, −0.96–−0.88; P = 0.94).
TABLE 7. Incidence of Severe Disability (FIMtot <9) by Injury Type
Outcomes According to Level of Severe Trauma Admissions
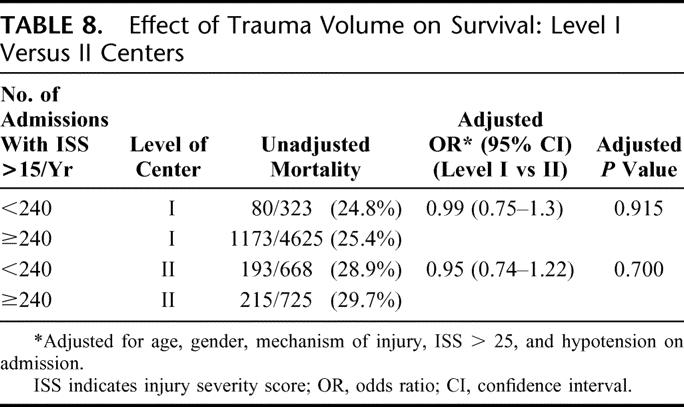
The effect of the number of admissions of patients with severe trauma (ISS >15) on outcome was studied in both level I and II centers. According to the ACS “Resources for Optimal Care of the Injured Patient,” one of the criteria for level I trauma center designation is volume performance, with a minimum of 240 severe trauma (ISS >15) admissions per year.
Multivariate analysis adjusting for age, gender, mechanism of injury, hypotension on admission, and ISS >25 or ≤25 showed that in level I centers, the volume of severe trauma (<240 vs ≥240 per year) did not have any effect on mortality. The crude mortality in level I centers with <240 admissions per year was 24.8%, and in centers with ≥240 admission per year, it was 25.4%. The adjusted OR was 0.99 (95% CI, 0.75–1.3; P = 0.915). Similarly, in level II centers, the trauma volume did not have any effect on mortality (28.9% vs 29.7%; adjusted OR, 0.95; 95% CI, 0.74–1.22; P = 0.70). Level I centers consistently had a significantly better outcome than level II centers irrespective of trauma volume (Table 8).
TABLE 8. Effect of Trauma Volume on Survival: Level I Versus II Centers
DISCUSSION
The creation of trauma centers and trauma programs has been shown to have a positive effect on outcomes in severely injured patients.1–3 The designation of trauma centers by the American College of Surgeons Committee on Trauma (ACS-COT) is a hospital resource-consuming and expensive process. The ACS-COT “Resources for Optimal Care of the Injured Patient” sets the numerous standards and requirements for the designation of a center in one of 4 levels.4 Identification of which of the required criteria for trauma center designation have an impact on the outcome in severely injured patients will improve care and possibly reduce costs.
To show significant outcome differences, it is essential to study patients with severe trauma who are at high risk of death or serious complications. Including a large number of patients with fairly minor or moderate severity injuries may obscure significant benefits to a much smaller group of critical injuries. This is a significant problem with many studies that have used all trauma registry patients or all patients with ISS >15 for outcome comparisons. To avoid this pitfall, the current study included only specific critical injuries that are associated with a very high mortality or disability.
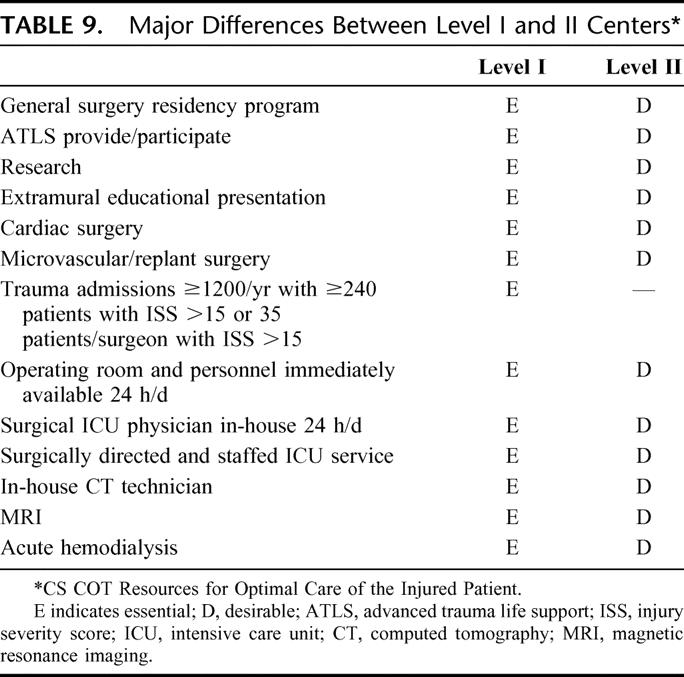
The criteria for level I trauma center designation are significantly more demanding than those for level II centers (Table 9). However, it is unknown if this designation has any effect on outcomes. There are 2 studies in the English literature that analyzed the impact of level of designation on outcome, and both suggested that the level of designation has no effect on survival. Pasquale et al5 analyzed the impact of level I or II trauma center designation, in the Pennsylvania trauma system, in 9 types of injuries (head, neck, chest, lung, liver, spleen, thoracic aorta, and vena cava). Logistic regression analysis failed to show that level of accreditation had an impact on survival, except in splenic injuries. Even this benefit was not conferred by the odds ratio analysis. A major criticism of the study is the use of the predicted survival with the ASCOT (A Severity Characterization of Trauma) method for comparisons. There is significant evidence that none of the current methods of predicting survival is reliable, especially in patients with severe trauma. Using these modalities for comparison of outcomes between trauma centers may be very misleading and may favor small centers that admit a small number of critical injuries. In a comparison of outcomes between a large level I and a small level II trauma center in Los Angeles, using the TRISS probability of survival and Z scores, Demetriades et al6 found a significantly better outcome in the small level II center. However, when all the patients from the small level II center were matched (age, gender, ISS, Glasgow Come score, head AIS, blood pressure, prehospital respiratory assistance, and transport mode) with an equal number of patients from the level I center, there was no difference in predicted outcome.6 The study highlighted the major pitfalls in using survival-predicting models for comparison of outcomes between trauma centers.
TABLE 9. Major Differences Between Level I and II Centers
Another study by Helling et al7 compared the mortalities of liver injuries between 2 level I and 4 level II trauma centers. The overall mortality in level I centers was 16% and in level II centers 15%. The mortality in 43 patients with liver injuries grade IV–V treated in level I centers was 51%, and in 14 patients treated in level II centers, it was 71% (P = 0.184). The authors concluded that level of designation does not have any effect on survival in liver injuries. However, these conclusions cannot be justified on the basis of only such a small number of cases with severe liver trauma.
The present study used observed survival outcomes in a large number of patients with critical injuries associated with a very high mortality for comparisons between centers with different designations. The study demonstrated clearly that in level I trauma centers, patients with specific critical injuries had a significantly better chance of survival and good functional outcomes than level II centers. This significant superiority of level I centers has never been shown before and may have major implications in the planning of trauma systems or billing of services according to level of accreditation.
It is difficult to identify the specific variables that are responsible for better outcomes in level I centers. Pasquale et al,5 using the ASCOT methodology for predicting survival, found that the presence of a general surgery residency program, which is a requirement for level I but not level II centers, was associated with significantly higher observed survival than predicted by ASCOT in 7 of the 9 injury categories studied, whereas centers without a general residency program were better than predicted by ASCOT in 5 of the 9 injury types.5 The pitfalls of using predictive models for comparing outcomes between centers have already been discussed.
Other required criteria for level I centers such as cardiac and microvascular/replant programs are unlikely to have made any difference in the outcomes of the studied specific injuries in the present study. Operating room availability and in-house operating room personnel 24 hours a day are expected requirements for level I but not level II trauma centers. The immediate availability of these resources may be critical in the survival of some injuries such as cardiac, vascular, or grade IV or V liver injuries. In a review of 2648 hospital trauma deaths from a level I center in Los Angeles, 17% of deaths resulting from severe chest trauma and 11% of deaths resulting from severe abdominal trauma, in victims reaching the hospital alive, occurred within 60 minutes of admission.8 Time to definitive care for these patients is of paramount importance, and the immediate availability of an operating room and operating personnel may play an important role in survival.
Other required criteria for level I but not level II centers that may play a role for the superior survival and functional outcomes include the in-house surgical intensive care unit physician and computed tomography scan technician. The effect of these variables on outcome is not known and is difficult to be assessed.
It is also possible that level I trauma centers attract more qualified and experienced trauma surgeons and surgical intensivists. Finally, research in the field of trauma in level I centers may improve outcomes by modifying practices and protocols.9
The effect of trauma volume on outcome is not clear, and there are conflicting reports. There is evidence that in other fields of complex surgery such as cardiac, vascular, neurosurgical, and oncologic procedures higher patient volumes result in better outcomes.10–13 However, the volume benefit is not applicable to less complex procedures associated with a low risk for serious complication or death such as cholecystectomy or operations for hip fractures.14 On the basis of this experience, the ACS-COT has set trauma volume criteria for the designation of level I centers. This volume criteria requires a minimum of 240 trauma admissions with ISS >15 per year.4 There has been significant controversy regarding this specific volume criterion. Smith et al15 analyzed the outcomes in 1643 severe injuries in level I trauma centers in the Chicago trauma system and reported that patient volume accounted for 30% to 40% of the observed variation in mortality rates. The mortality odds ratio of low-volume centers (<140 severe injuries per year) was 1.3 when compared with high-volume centers (>200 cases per year) (P = 0.00).15
Nathens et al16 also reported an inverse relationship between trauma volume and mortality. In a study that included 32 academic level I or II trauma centers, the authors reported that patients with penetrating abdominal trauma admitted with shock or multisystem blunt trauma who were admitted in coma had significantly better survival and shorter length of stay if treated in high-volume centers (>650 cases with ISS >15 per year) than low-volume centers (≤650 cases per year). There was no difference in outcomes between high- and low-volume centers in penetrating abdominal injuries not in shock or multitrauma patients not in coma. The authors stressed that fairly minor trauma with a low mortality is unlikely to benefit from the resources of a high-volume level trauma center.
Another study from 39 California trauma hospitals analyzed outcomes in 4352 patients in the age group 16–64 years and 47,656 elderly patients (>65 years) admitted with ISS > 9.17 The authors concluded that in the age group >65 years, higher annual trauma volume was associated with lower mortality (OR, 0.79 for each 100 admissions; 95% CI, 0.71–0.87).
Other publications have challenged the inverse relationship between high trauma volume and mortality. Cooper et al,18 in an analysis of trauma outcomes from the New York State trauma centers, reported that the overall mortality in low-volume (<240 patients with ISS >15) was 7.62% versus 5.25% in the high-volume centers. The authors concluded that volume criteria should not be used in the designation of trauma centers. However, as pointed out by Nathens,16 only patients at high risk of death may benefit from the experience and resources of a high-volume center. The low mortality in Cooper's study indicates that a large number of minor injuries were included in the analysis. In addition, the study excluded patients who were alive on admission but died in the emergency room. This exclusion may favor small centers with inadequate resources and slow responses in which patients may die in the emergency room instead of being transferred to the operating room.
In another study from Los Angeles, Margulies et al19 analyzed 1754 trauma patients with ISS >15 from 5 level I centers. Logistic regression analysis showed that institutional volume correlated negatively with survival. The study included patients admitted with no vital signs, which may be in favor of smaller centers that do not see a large number of penetrating trauma victims reaching the hospital without vital signs and undergo unsuccessful resuscitative thoracotomies.
Glance et al20 performed a NTDB study of 7371 patients with ISS ≥15 who were alive on admission. Logistic regression analysis failed to demonstrate any association between trauma volume and outcome in both blunt and penetrating trauma. The authors suggested that ACS volume criteria for level I trauma centers need to be reevaluated. In another study from 38 level I and II centers, London et al21 suggested that trauma volume was not a significant predictor of death or length of hospital stay in patients with ISS <15 or ISS >15. Some critics discussing the study express concerns about using the ISS alone as a marker of the severity of an injury.21
The present study has shown clearly that the existing volume criteria for level I trauma centers cannot be supported, at least in the studied subgroups of patients with specific critical injuries.
Intuitively, one would expect an inverse relationship between trauma volume and outcomes because of the experience gained by the trauma program in the management of complex injuries.
It is possible that the high standards required by the ACS for level I designation compensate adequately for the relative lack of high-volume experience. It is also possible that the optimal volume is different from the 240 patients set by the ACS-COT. Irrespective of the reasons for this finding, the existing evidence does not support the use of the current volume criteria for accreditation purposes.
In conclusion, the current study, has provided strong evidence that ACS-designated level I trauma centers have significantly better survival and functional outcomes than level II or other trauma centers for select severe injuries. This finding may have practical implications in the planning of trauma systems, triage of patients to trauma centers, and financial compensation of services according to level of center accreditation.
ACKNOWLEDGMENTS
This study was made possible by the National Trauma Data Bank of the Committee on Trauma of the American College of Surgeons.
Discussions
Dr. L.D. Britt (Norfolk, Virginia): The purpose of this study was to investigate the effect of the ACS trauma center verification and trauma volume in patients with specific injuries and to validate the trauma volume as a criterion for Level I verification.
The authors have made some sweeping conclusions based on the retrospective analysis of the data from the National Trauma Data Bank, which included patients greater than 14 years of age, ISS greater than 15, and patients who had at least an aortic iliac vessel cardiac grade 4–5 hepatic injury, quadriplegia, and complex fractures. Over 12,000 patients met these inclusion criteria.
Although the authors state that univariate analyses were performed in order to make comparisons between Level I and Level II cases, nowhere in the manuscript that I received are these comparisons discussed, and not one of the 8 tables summarizing these compasons e contned ithe sociated P values. The only P values contained in the tables derived from the multivariate logistic regression analysis.
And considering that the comparisons in this sort of setting usually are made based on univariate analysis which determine independent variables that are actually to be used, I guess I have to ask the authors: How did they come up with these variables? Can I assume that these variables were chosen arbitrarily? Could more variables have been used? And even if the findings remained the same after more stringent statistical analysis, what are the specific implications of your conclusions? What would be the proposed changes in a given trauma system? What would be the likelihood logistical concerns about regionalization?
When one compares the essentials needed for Level I as compared to Level II, as you did, a lot of the Level II centers still have, although it is desired, they still have the components that you highlighted in Level I. If that is the case, why would there be a difference? What would be the specific component of Level I which would give it superiority as you concluded in your study? Finally, at the end of the day, even if your conclusions are correct, logistically speaking there are not enough Level I trauma centers to obviously supply the whole United States. How do you feel that we should implement your findings?
I really enjoyed this. As always, Dr. Demetriades and his colleagues have led the way with respect to making substantial contributions to our discipline.
Dr. Demetrios Demetriades (Los Angeles, California): Thank you, Dr. Britt. First I want to assure you that the conclusions are valid and solely based on good statistical analysis.
In the statistical analysis we used univariate logistic regression models using forced entry criteria to examine the effect of ACS designation on mortality after adjusting for age, gender, injury mechanism (blunt or penetrating), injury severity score, and hypotension on admission (systolic blood pressure <90).
Which characteristics could have lead to better outcomes in Level I centers? I am not sure. We couldn't identify which ones could have contributed to the different outcomes. There are some possibilities:
Number 1, in Level I trauma centers it is compulsory that you have 24-hour OR availability with OR staff in-house. In this study, 50% of these patients were transferred from the emergency room to the operating room. Would the immediate availability of the OR make a difference? I think yes. In another analysis of about 2600 deaths from Los Angeles, a large number of deaths due to abdominal or chest trauma, occurred within 1 hour of admission. In this group of patients OR availability might have made a significant difference. Another factor which might be significant in explaining the different outcomes is the academic status of Level I trauma centers, which usually attract better qualified people. Another variable, which in my mind might play a critical role, is research. Research might identify weaknesses or problems in a program, which can be corrected with the appropriate action and result in improved outcomes. We have shown this in elderly trauma patients.
So what is the practical implication of this study? As I mentioned, when you plan a trauma system you need to designate Level I and Level II trauma centers in strategic places. If in a particular area there are both, Level I and Level II trauma centers, perhaps certain groups of critically injured patients might be better served by spending a extra few minutes, bypass a Level II and transfer them to a Level I trauma center.
Dr. Lewis M. Flint, Jr. (Tampa, Florida): I have a couple of comments.
You have made some recommendations and some conclusions regarding trauma systems by comparing results from trauma centers. And I am not sure you can necessarily make the leap from the trauma center comparison to characteristics of trauma systems.
We recently completed a study of the state trauma system here in Florida. Florida has a mature trauma system that is more than 20 years old. More than 90% of its citizens of Florida are covered by advanced life support, prehospital care, EMS systems. We have 21 trauma centers in the state, 7 Level I centers and the rest are Level II and specifically designated children's centers.
We used a case-matching strategy where we matched cases that were triaged to trauma centers for diagnostic characteristics with cases that were triaged to nontrauma centers. We found that there is an 18% survival advantage for being triaged to a trauma center in Florida. So we confirmed that the trauma system in Florida confers a survival advantage. But we also found a disturbing gap between the results of patients who were triaged to Level I centers and patients who were triaged to Level II centers.
I am not sure that you can take data out of the National Trauma Data Bank and make statements about trauma systems because you don't know what the capability of prehospital care system is for those hospitals, you don't know what the individual hospital capability is.
Nonetheless, I do believe that our study does support your observations that there is a distinct survival advantage for patients who are triaged to trauma centers.
Dr. Demetrios Demetriades (Los Angeles, California): Thank you, Dr. Flint, for that very good comment. I am very pleased and excited that you had more or less similar results with our study regarding Level I versus Level II trauma centers.
When I talk about changes in trauma systems, I refer to the geographic location of the centers and the triage to Level I or Level II trauma centers. It might be appropriate that for certain types of trauma, such as penetrating injuries to the chest or abdomen with hypotension, the paramedics bypass a Level II center in favor of a Level I center. These are the kinds of changes I had in mind.
Dr. Ronald V. Maier (Seattle, Washington): I congratulate the authors for using the NTDB to initiate discussions and to make us question what we do. I have a couple of quick questions and a comment.
In our state, like in many states, the Level IIs are dropping out and becoming Level IIIs because they can't find a neurosurgeon or they can't find this or that, and it is just easier to drop back to being a Level III. One of the issues that comes out of your presentation is that you have given them support. Why spend the extra money, because as a Level II they are no better than a Level III anyhow. Could you comment on that effect and the impact it is going to have on system development and stability that is being challenged in many areas of the country?
The authors used the cut point that is in the COT document of 240 patients for a low-volume versus high-volume trauma center. The number we showed with an analysis of national outcomes of statewide trauma system development actually defines high volume as greater than 500 and not 240. I wondered why you tested the number as a dichotomous variable rather than a continuous variable and with a line through the 0.05 value you could have told us what the number of patients required was and contributed to our knowledge and definition for the future.
However, more than argue an absolute one number to fit all, I think what your data show and support, and I would like your comment on this, as we heard from our president this morning in his Presidential Address, is rather than use arbitrary numbers of volume to determine good and bad, we need to focus on process of quality care, which is what you have also identified in your paper.
The Level I trauma centers, that have optimized the process of care of the injured patient and made the institutional commitments to that care, are actually able to produce the best outcomes. So by monitoring process rather than arbitrary numbers, we may be able to achieve the best quality for our patients.
Dr. Demetrios Demetriades (Los Angeles, California): For this particular group of patients, Level II versus III, or not designated centers, did not make any difference. But I want to be very clear. I am talking about this very specific group of injuries. Perhaps in other injuries, less severe injuries, Level II trauma centers might make a significant difference. So I am very careful with that.
Why did we use the magic number of 240? Because this is what is used in the Optimal Resources for the Care of the Injured Patient by the Committee on Trauma of the American College of Surgeons. This is a very controversial and emotional issue. A lot of centers do not meet these criteria and get very upset about this arbitrary number.
Dr. J. Wayne Meredith (Winston-Salem, North Carolina): I wanted to ask a continuous variable question. But I will answer Dr. Maier's question, which is: How do we come up with the number of 240? I think he described it pretty well. We got a group of people in the room and we argued over a number until there was only 1 person standing. I believe that Ron, as a matter of fact, was the last person standing. Let me ask you these 2 questions.
One is with regard to the volume performance criteria. I strongly support the notion of measuring what the right number is and then looking at that. The other is the lack of performance of that 240 criterion – greater than 15 due to overloading of the current trauma centers, so that we are now at a point where these very high volume centers have a fall-off in their mortality, a fall-off in the survival rates because they are being overwhelmed.
The other question is, can you look at or did you look at the volume of these specific injuries so that it is not a generic volume of trauma patients? But is there any evidence that the frequency of these very specific injuries, which you have selected? It seems to me these injuries are very amenable to highly skilled and available surgeons, more than being amenable to a well-functioning overall system, is there any relationship between volume of the center for these injuries?
Dr. Demetrios Demetriades (Los Angeles, California): Yes, you are right, we used the criterion of >240 patients with ISS >15. We tried to analyze according to numbers of specific severe injuries. However, the numbers became too small for any further meaningful analysis, calculate 12,000 patients divided by 248 centers.
Finally, I agree with you that the issue of the ideal number of major trauma admissions has not been resolved yet.
Footnotes
Reprints: Demetrios Demetriades, MD, PhD, FACS, Director, Trauma and Critical Care, LAC+USC Healthcare Network, 1200 N. State Street, Room 1105, Los Angeles, CA 90033. E-mail: demetria@usc.edu.
REFERENCES
- 1.Sampalis JS, Lavoie A, Bookas S, et al. Trauma center designation: initial impact on trauma-related mortality. J Trauma. 1995;39:232–239. [DOI] [PubMed] [Google Scholar]
- 2.Baker CC, Degutis LC, DeSantis J, et al. Impact of a trauma service on trauma care in a university hospital. Am J Surg. 1985;149:453–458. [DOI] [PubMed] [Google Scholar]
- 3.Demetriades D, Berne TV, Belzberg H, et al. The impact of a dedicated trauma program on outcome in severely injured patients. Arch Surg. 1995;130:216–220. [DOI] [PubMed] [Google Scholar]
- 4.Committee on Trauma, American College of Surgeons. Resources for Optimal Care of the Injured Patient. 1999.
- 5.Pasquale MD, Peitzman AB, Bednarski J, et al. Outcomes analysis of Pennsylvania trauma centers: Factors predictive of non-survival in seriously injured patients. J Trauma. 2001;50:465–474. [DOI] [PubMed] [Google Scholar]
- 6.Demetriades D, Chan L, Velmahos G, et al. TRISS methodology: an inappropriate tool for comparing outcomes between trauma centers. J Am Coll Surg. 2001;193:250–2541. [DOI] [PubMed] [Google Scholar]
- 7.Helling TS, Morse G, Mcnabney WK, et al. Treatment of liver injuries at level I and level II centers in a multi-institutional metropolitan trauma system. The Midwest Trauma Society Liver Trauma Study Group. J Trauma. 1997;42:1091–1096. [DOI] [PubMed] [Google Scholar]
- 8.Demetriades D, Murray J, Charalambides K, et al. Trauma fatalities: time and location of hospital deaths. J Am Coll Surg. 2004;198:20–26. [DOI] [PubMed] [Google Scholar]
- 9.Demetriades D, Karaiskakis M, Velmahos G, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg. 2002;89:1319–1322. [DOI] [PubMed] [Google Scholar]
- 10.Birkmeyer JD, Finlayson SR, Tosteson AN, et al. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery. 1999;125:250–256. [PubMed] [Google Scholar]
- 11.Solomon RA, Mayer SA, Tarmey JJ. Relationship between the volume of craniotomies for cerebral aneurysm performed at New York hospitals and in-hospital mortality. Stroke. 1996;27:13–17. [DOI] [PubMed] [Google Scholar]
- 12.Begg CB, Cramer CD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–1751. [DOI] [PubMed] [Google Scholar]
- 13.Hannan EL, Popp AJ, Tranmer B, et al. Relationship between provider volume and mortality for carotid endarterectomies in New York state. Stroke. 1998;29:2292–2297. [DOI] [PubMed] [Google Scholar]
- 14.Luft HS, Bunker JP, Enthoren AC. Should operations be regionalized. The empirical relation between surgical volume and mortality? N Engl J Med. 1979;301:1364–1369. [DOI] [PubMed] [Google Scholar]
- 15.Smith RF, Frateschi L, Sloan EP, et al. The impact of volume on outcome in seriously injured patients: two years’ experience of the Chicago trauma system. J Trauma. 1990;30:1066–1076. [DOI] [PubMed] [Google Scholar]
- 16.Nathens AB, Jurovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285:1164–1171. [DOI] [PubMed] [Google Scholar]
- 17.Marcin JP, Romano P. Impact of between-hospital volume and within-hospital volume on mortality and readmission rates for trauma patients in California. Crit Care Med. 2004;32:1477–1483. [DOI] [PubMed] [Google Scholar]
- 18.Cooper A, Hannan EL, Bessey PQ, et al. An examination of the volume–mortality relationship for New York state trauma centers. J Trauma. 2000;48:16–24. [DOI] [PubMed] [Google Scholar]
- 19.Marguilies DR, Cryer HG, McArthur DL, et al. Patients volume per surgeon does not predict survival in adult level I trauma centers. J Trauma. 2001;50:597–603. [DOI] [PubMed] [Google Scholar]
- 20.Glance GL, Osler TM, Dick A, et al. The relationship between trauma center outcome and volume in the national Trauma Data Bank. J Trauma. 2004;56;682–690. [DOI] [PubMed] [Google Scholar]
- 21.London JA, Bastistella FD. Is there a relationship between trauma center volume and mortality? J Trauma. 2003;54:16–24. [DOI] [PubMed] [Google Scholar]