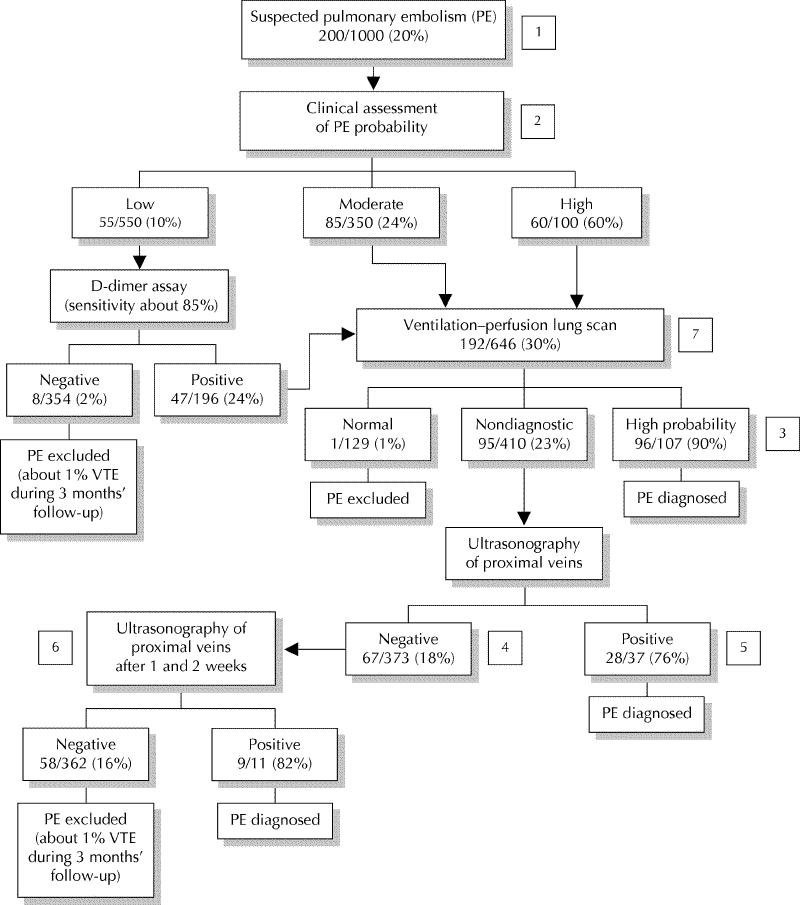
Fig. 1: A diagnostic algorithm for pulmonary embolism (estimated frequencies of test results and associated prevalences of pulmonary embolism for a hypothetical cohort of 1000 outpatients) [1]. If a very sensitive D-dimer assay is used, it can be the first test performed: a negative result excludes pulmonary embolism regardless of clinical assessment category and a positive test can be followed by a ventilation–perfusion scan [2]. A ventilation–perfusion scan can be performed as the initial test without using clinical assessment of the probability of pulmonary embolism as part of the diagnostic process [3]. Pulmonary angiography or helical CT may be considered if the clinical assessment of pulmonary embolism probability is low, particularly if a D-dimer test has not been done [4]. Additional testing (e.g., helical CT, bilateral venography) may be considered if overall assessment suggests a high probability of pulmonary embolism (e.g., 50%–80%), symptoms are severe or cardiopulmonary reserve is poor [5]. Venography should be considered if there is an increased risk of a false-positive ultrasound result (e.g., previous venous thromboembolism, equivocal ultrasound findings, preceding findings suggest low probability of pulmonary embolism [e.g., ≤ 10%]) [6]. It is reasonable not to repeat ultrasound testing, or to do only 1 more ultrasound after 1 week, if preceding findings suggest a low probability of pulmonary embolism (e.g., ≤ 10%) [7]. If helical CT is used in place of ventilation–perfusion lung scanning: (i) intraluminal filling defects in segmental or larger pulmonary arteries are generally diagnostic for pulmonary embolism; (ii) all other findings (i.e., a normal CT scan or intraluminal filling defects confined to the subsegmental pulmonary arteries) are nondiagnostic and can be managed as shown for a nondiagnostic lung scan.
