Figure 1.
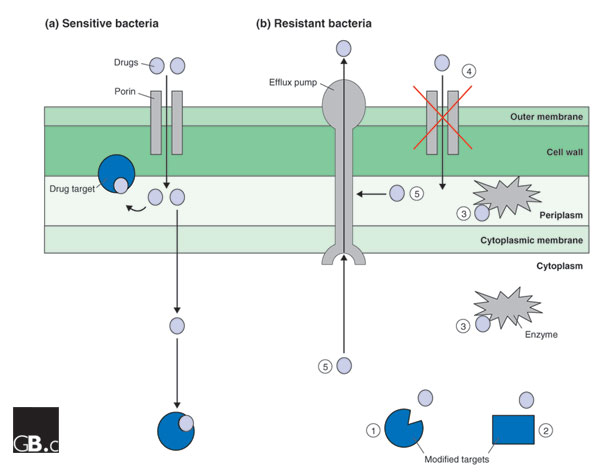
Antimicrobial drug-resistance mechanisms. A typical Gram-negative bacterial cell envelope is shown, consisting of the outer membrane, the peptidoglycan cell wall, the periplasm, which contains enzymes required to synthesize the cell wall, and the cytoplasmic membrane. (a) The entry point and targets of antimicrobial drugs in a non-resistant bacterium. Drugs enter the periplasm through porins in the outer membrane, and some drugs exert their effect in the periplasm; for example, ampicillin and the other β-lactams interfere with the synthesis of the cell wall. Other drugs cross the cytoplasmic membrane and inhibit cytoplasmic targets. (b) Possible resistance mechanisms: (1) Mutation of a target so that it is no longer inhibited by the drug; (2) acquisition, for example on a plasmid, of a novel target that is not sensitive to the actions of the drug; (3) enzymatic destruction or modification of the drug either in the cytoplasm, for example, the inactivation of gentamicin by aminoglycoside-modifying enzymes, or in the periplasm, for example, the destruction of β-lactams by β-lactamase; (4) reduction of the cytoplasmic, and usually periplasmic, concentration of the drug through reduction in the expression of porin genes or loss-of-function mutations in porin genes; (5) removal of drugs from the periplasm or cytoplasm by efflux pumps. In some cases, drug resistance is due to a combination of these mechanisms.
