Abstract
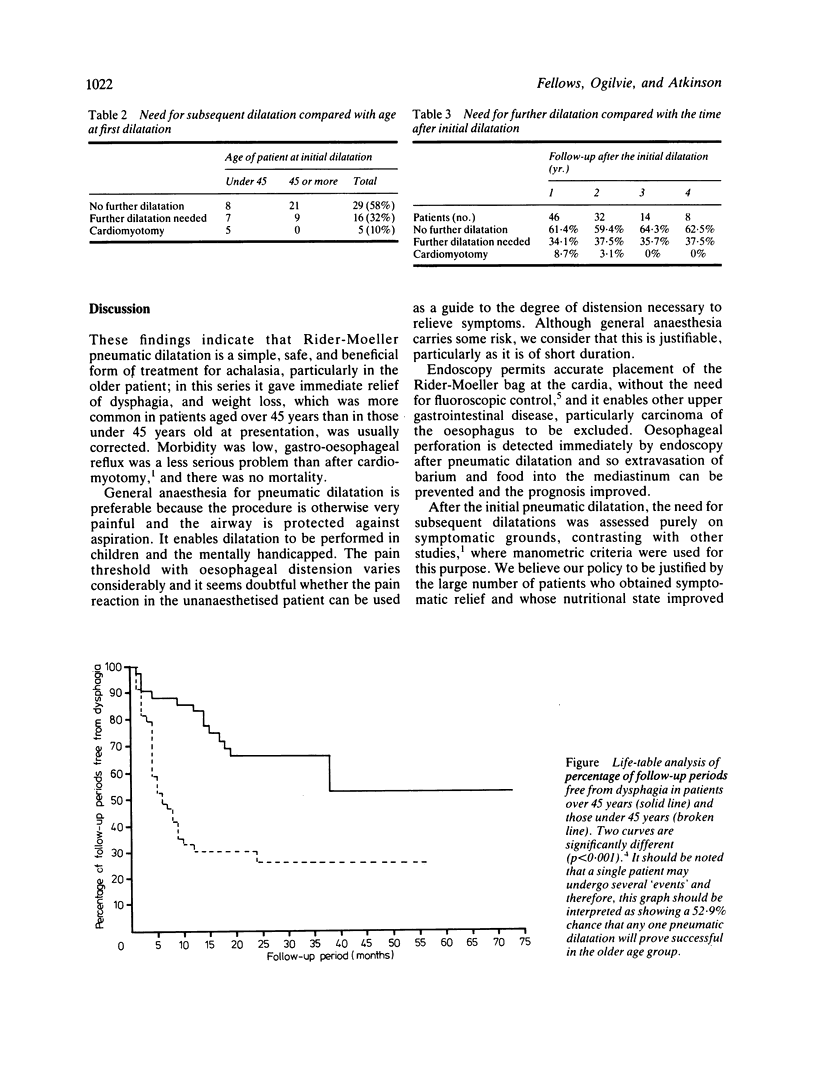
To assess the value of pneumatic dilatation of the cardia, 63 patients with achalasia have undergone a total of 107 Rider-Moeller dilatations over the last six years. There was a marked improvement in swallowing immediately after dilatation in all but two patients, there were no deaths attributable to the procedure and serious complications were rare (1.6% of patients). The first 50 cases have been followed from nine to 73 months after their initial dilatation (mean follow-up 29.7 months). Twenty nine patients (58%) have not required a further dilatation, 19 patients (38%) required between one and three further dilatations and two patients (4%) required four more dilatations. Continuing need for further dilatation was significantly greater in those patients aged under 45 years than in those aged 45 or more at the time of their initial dilatation (p less than 0.001). Cardiomyotomy was necessary in five patients (10%), because of poor response to pneumatic dilatation; all five cases were under 45 years old at their initial dilatation. Pneumatic dilatation is a safe and effective treatment for achalasia, particularly in the older patient, and in our opinion should be the initial treatment for all patients with achalasia, reserving surgical cardiomyotomy for those who do not respond to several dilatations.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Black J., Vorbach A. N., Collis J. L. Results of Heller's operation for achalasia of the oesophagus. The importance of hiatal repair. Br J Surg. 1976 Dec;63(12):949–953. doi: 10.1002/bjs.1800631215. [DOI] [PubMed] [Google Scholar]
- Castell D. O. Achalasia and diffuse esophageal spasm. Arch Intern Med. 1976 May;136(5):571–579. [PubMed] [Google Scholar]
- Csendes A., Velasco N., Braghetto I., Henriquez A. A prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Gastroenterology. 1981 Apr;80(4):789–795. [PubMed] [Google Scholar]
- Lishman A. H., Dellipiani A. W. Management of achalasia of the cardia by forced pneumatic dilatation. Gut. 1982 Jun;23(6):541–544. doi: 10.1136/gut.23.6.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobello R., Edwards D. A., Gummer J. W., Stekelman M. The anti-reflux mechanism after cardiomyotomy. Thorax. 1978 Oct;33(5):569–573. doi: 10.1136/thx.33.5.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okike N., Payne W. S., Neufeld D. M., Bernatz P. E., Pairolero P. C., Sanderson D. R. Esophagomyotomy versus forceful dilation for achalasia of the esophagus: results in 899 patients. Ann Thorac Surg. 1979 Aug;28(2):119–125. doi: 10.1016/s0003-4975(10)63767-8. [DOI] [PubMed] [Google Scholar]
- Peto R., Pike M. C., Armitage P., Breslow N. E., Cox D. R., Howard S. V., Mantel N., McPherson K., Peto J., Smith P. G. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer. 1977 Jan;35(1):1–39. doi: 10.1038/bjc.1977.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rider J. A., Moeller H. C., Puletti E. J., Desai D. C. Diagnosis and treatment of diffuse esophageal spasm. Arch Surg. 1969 Oct;99(4):435–440. doi: 10.1001/archsurg.1969.01340160015004. [DOI] [PubMed] [Google Scholar]
- Vantrappen G., Hellemans J. Treatment of achalasia and related motor disorders. Gastroenterology. 1980 Jul;79(1):144–154. [PubMed] [Google Scholar]
- Yon J., Christensen J. An uncontrolled comparison of treatments for achalasia. Ann Surg. 1975 Dec;182(6):672–676. doi: 10.1097/00000658-197512000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]


