Abstract
Objective
To examine trends in patient and procedural variables and outcomes associated with autogenous lower extremity arterial reconstruction (LER) in a single center during a period of two decades.
Summary Background Data
Surgical arterial reconstruction is of proven value in the therapy of patients with critical ischemia of the lower extremities. Changing demographics and increasing comorbidity are resulting in an increasing prevalence and associated complexity of peripheral vascular disease. The effect of these variables on the types and outcomes of surgical reconstructions is not known.
Methods
The authors performed a retrospective analysis of all autogenous LER procedures performed at their institution from 1978 to 1997. Procedures were divided into 5-year intervals: group 1, 1978 to 1982; group 2, 1983 to 1987; group 3, 1988 to 1992; group 4, 1993 to 1997. Categorical parameters were compared using chi-square analysis; rates were computed by the life-table method and compared using Mantel-Cox log-rank analysis.
Results
A total of 1,642 autogenous LER procedures were performed in 1,274 patients. A significant increase in age, female gender, diabetes mellitus, renal failure, and prior coronary artery bypass grafting was noted in group 4. Increased technical complexity in this group was reflected by a greater incidence of tissue necrosis as the indication for LER, the use of ectopic or composite vein, and more distal levels of outflow. The surgical death rate remained unchanged (2%) throughout. Patient survival, primary and secondary graft patency, and limb salvage at 5 years for the entire cohort were 70 ± 2%, 63 ± 2%, 73 ± 1%, and 85 ± 1%, respectively. Hospital length of stay was reduced 25% from a mean of 15.7 ± 0.8 days in group 3 to 11.7 ± 0.4 days in group 4.
Conclusion
In a tertiary practice setting, patients requiring LER present an increasingly complex medical and surgical challenge compared with the previous decade. Excellent outcomes may still be achieved by an aggressive approach relying on autogenous vein conduit.
The past two decades have witnessed a progressive decline in cardiovascular disease-specific death rates in the United States population. 1 This fact, combined with a demographic trend of growth in the older segment of the population most at risk for atherosclerosis, is likely to have a substantial impact on the treatment of lower extremity arterial occlusive disease by vascular specialists. More aggressive management of atherosclerotic risk factors as well as end-organ (cardiac, renal, cerebral) dysfunction may be expected to lead to both a growth in demand and a shift in the profile of patients undergoing lower extremity arterial reconstruction (LER). Although the efficacy and durability of LER for both limb salvage and disabling claudication have been well established, 2–4 the potential effects of shifting demographics and comorbidities on surgical outcomes, quality of life, workload, and costs are important for vascular surgeons and the national healthcare system.
In addition to national trends in the demographics and prevalence of peripheral atherosclerosis, numerous local factors, including referral patterns, institutional treatment biases, marketplace forces, and socioeconomic profiles, exert a profound influence on the practice of vascular surgery. For many tertiary-care medical centers, the changes in healthcare economics have resulted in an increase in case-mix complexity, a phenomenon often referred to as cost-shifting. This, in turn, may lead to a higher proportion of adverse outcomes, prolonged hospital stays, greater resource utilization, and increased costs. The effects of such changes in a referral population on the outcome of interventions must be carefully evaluated to maintain the appropriate delivery of quality care. Also, as reimbursement continues to decline, the effects of a shift in case complexity on both the in-hospital and the outpatient practice of vascular surgery may be profound.
Since the early 1980s, the preferred approach to LER in our institution has relied on autogenous vein conduit. 5,6 This preference is supported by the excellent results reported from many centers, using autogenous vein in a variety of configurations for infrainguinal bypass. In our local environment, we have observed an increasing trend of patient comorbidity, case complexity, and volume of services required for the management of infrainguinal arterial occlusive disease during the past decade. The current study was undertaken to determine the magnitude of these perceived shifts and their impact on the short-term and long-term surgical outcomes for patients undergoing autogenous LER.
METHODS
We conducted a retrospective review of patients who had undergone LER using autogenous vein at Brigham and Women’s Hospital between January 1, 1978, and December 31, 1997. Data were retrieved from a UNIX-based computerized registry in which demographics, risk factors, procedure variables, and follow-up information have been prospectively entered for all vascular surgery patients at our institution since 1975. Patients were divided into four intervals for analysis: group 1, 1978 to 1982; group 2, 1983 to 1987; group 3, 1988 to 1992; and group 4, 1993 to 1997.
The techniques used for autogenous LER have been reported elsewhere and generally included both preoperative and completion arteriography, a surgical team composed of a staff surgeon and either a vascular fellow or senior resident, loupe magnification, and standard anastomotic techniques. Specific technical aspects of conduit preparation for in situ 7 or nonreversed 8 greater saphenous vein grafts have been previously described by our group.
A uniform approach to postoperative graft surveillance was not applicable to the entire 20-year period. In general, follow-up examinations occurred within the first month of surgery, then at roughly 3-month intervals for the first year and annually thereafter. Duplex scanning progressively replaced noninvasive hemodynamic studies (ankle–brachial index) as the primary method for detecting occult graft lesions in the last two intervals. A return of symptoms, focal increase in graft velocity (ratio > 3.5:1), decreased overall graft velocity (<45 cm/s), or a decrease in the ankle–brachial index of greater than 0.1 between visits were considered evidence of significant lesions and usually mandated arteriography.
Minor amputations were defined as those resulting in a walkable foot. Limb salvage was correspondingly defined as freedom from major amputation. Primary and secondary patency were defined per the suggested reporting standards of the SVS/ISCVS Ad Hoc Committee. 9 Survival, graft patency, and limb salvage rates were calculated by the life-table method. Standard errors were calculated by the Greenwood method, 10 and comparisons between groups were made by Mantel-Cox log-rank analysis. Categorical variables were compared using chi-square analysis. P < .05 was considered to represent statistical significance.
RESULTS
A total of 1,642 autogenous vein LER procedures were performed in 1,274 patients between 1978 and 1997. Overall, follow-up was complete in 70% of patients for a mean of 968 (range 0–6,922) days. The proportion of patients lost to follow-up in each of the four intervals, in sequence, was 44%, 32%, 37%, and 18%.
Figure 1 shows the numbers of procedures performed in each group. The proportion of secondary (redo) bypass grafts remained fairly constant at approximately 20% of total autogenous reconstructions (Table 1). During the same period, 323 prosthetic LER procedures were performed, 80% between 1978 and 1987. The proportion of all LER procedures performed with a prosthetic conduit was 35%, 24%, 5%, and 7% in the four sequential intervals. Figure 1 also shows the frequency of both primary major amputation and minor amputations in the intervals. Although the number of primary amputations remained relatively constant over the entire period, a significant increase in associated minor amputations was found in group 4.
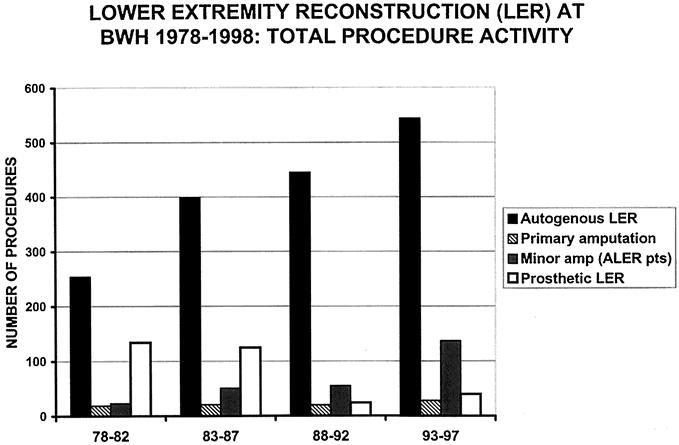
Figure 1. Total numbers of lower extremity arterial reconstruction (LER) procedures performed in each of the four 5-year intervals. Minor amputations shown were performed in patients who had also undergone LER.
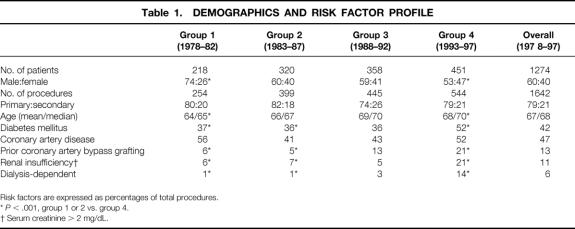
Table 1. DEMOGRAPHICS AND RISK FACTOR PROFILE
Risk factors are expressed as percentages of total procedures.
*P < .001, group 1 or 2 vs. group 4.
† Serum creatinine > 2 mg/dL.
Demographics and Risk Factors
Table 1 summarizes the demographic and risk factor profile for the patients. A significant increase in age and female gender was found in group 4 compared with the earliest interval. Of the numerous risk factors tracked in the registry database, several showed significant trends. In particular, the frequency of diabetes mellitus, prior coronary artery bypass grafting, and renal failure were all significantly increased in group 4 compared with earlier intervals. Smoking, hypertension, coronary artery disease, stroke, and chronic obstructive pulmonary disease showed no significant changes in incidence during the entire period.
Procedural Variables
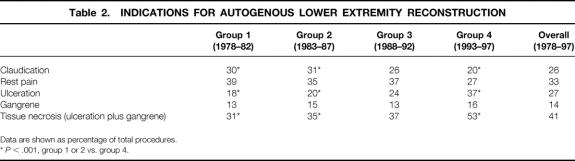
Table 2 lists the frequency of each of the indications for LER. We found a progressive decrease in procedures for claudication and a significant increase in patients undergoing LER for tissue necrosis (ulceration or gangrene) in group 4 compared with earlier intervals.
Table 2. INDICATIONS FOR AUTOGENOUS LOWER EXTREMITY RECONSTRUCTION
Data are shown as percentage of total procedures.
*P < .001, group 1 or 2 vs. group 4.
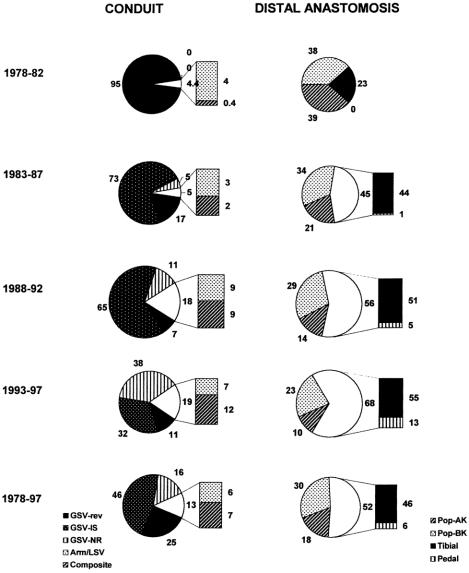
Figure 2 illustrates conduit usage and distal anastomotic sites for all grafts. Although reversed greater saphenous vein grafts represented 95% of the autogenous LER procedures in group I, a marked preference for the in situ greater saphenous vein was apparent from 1983 through 1992. In comparing groups 3 and 4 with the earlier periods, a trend toward increasing use of nonreversed greater saphenous vein and ectopic (arm, lesser saphenous) or composite vein grafts was evident (P < .001 for groups 1, 2 vs. group 4). The frequency of ectopic/composite vein use increased in a fashion parallel to the incidence of prior coronary artery bypass grafting. In group 4 patients, ectopic/composite vein was required in 37% of procedures in patients with a history of prior coronary artery bypass, compared with 14% of bypass grafts in patients who had not undergone prior coronary artery bypass (P < .001).
Figure 2. Changing patterns of autogenous lower extremity arterial reconstruction during a 20-year period. Types of conduit used are shown in pie charts on the left; the unshaded area indicates the total of all ectopic (arm, lesser saphenous vein, composite) grafts. Breakdown of distal anastomotic sites is illustrated in the pie charts on right, with the unshaded area representing total infrageniculate outflow sites (tibial plus pedal). GSV-rev, reversed greater saphenous vein, GSV-IS, in-situ greater saphenous vein, GSV-NR, nonreversed greater saphenous vein, ARM/LSV, either arm vein or lesser saphenous vein; composite, composite vein, Pop-AK, above-knee popliteal artery; Pop-BK, below-knee popliteal artery.
Also shown in Figure 2 is the progressively distal levels of LER performed during the intervals. There was a significant increase in tibial/pedal outflow sites in group 4 (68%) compared with groups 1 (23%) and 2 (45%, P < .001). The common femoral and superficial femoral arteries provided inflow for 89% of all grafts in the series. A significant increase in use of the popliteal artery for inflow was noted in group 4 (15%) compared with earlier intervals (group 1, 3%; group 2, 5%; group 3, 9%).
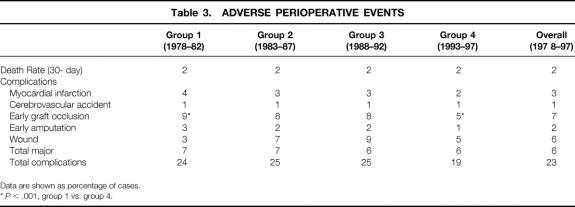
Perioperative Events
The frequency of adverse perioperative events is listed in Table 3. The 30-day death rate remained constant at 2% for all four intervals, as did virtually all major and minor complication rates. The occurrence of early postoperative graft occlusion was significantly decreased in group 4 (5%) compared with group 1 (9%, P < .02).
Table 3. ADVERSE PERIOPERATIVE EVENTS
Data are shown as percentage of cases.
*P < .001, group 1 vs. group 4.
Patient Survival and Graft Patency
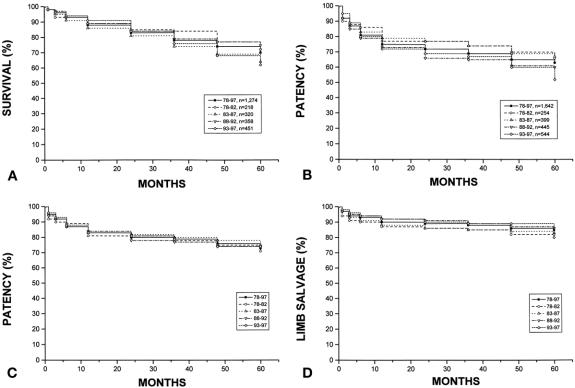
Cumulative patient survival, graft patency, and limb salvage rates are summarized in Figure 3 and Table 4. For the entire cohort in each interval, there were no significant differences noted between groups for survival; primary, primary revised, or secondary patency; or limb salvage at 5 years. Overall survival was 70 ± 2% at 5 years, with secondary graft patency of 73 ± 1% and limb salvage of 85 ± 1%.
Figure 3. Life-table plots of patient survival (A), patency (primary [B] and secondary [C]), and limb salvage (D) for all autogenous lower extremity arterial reconstructions during each of the four 5-year intervals and overall (1978–1997).
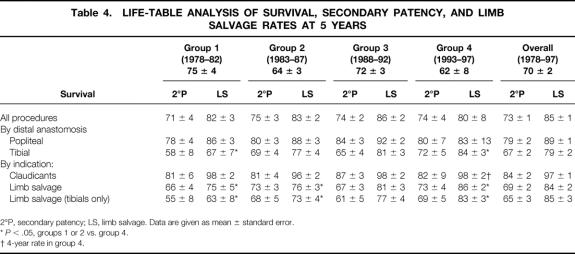
Table 4. LIFE-TABLE ANALYSIS OF SURVIVAL, SECONDARY PATENCY, AND LIMB SALVAGE RATES AT 5 YEARS
2°P, secondary patency; LS, limb salvage. Data are given as mean ± standard error.
*P < .05, groups 1 or 2 vs. group 4.
† 4-year rate in group 4.
Improved results were noted in patients undergoing distal reconstructions and limb salvage procedures. A significant improvement in 5-year limb salvage rates for tibial bypass grafts was noted in group 4 (84 ± 3%) compared with group 1 (67 ± 7%, P < .02). A trend toward improved secondary patency for tibial grafts was noted, but it did not reach statistical significance (P < .06). Similarly, in evaluating results for LER procedures performed exclusively for limb salvage indications, we found improved limb preservation (86 ± 2% in group 4 vs. 75 ± 5% in group 1 at 5 years) in the more recent intervals. Figure 4 illustrates secondary patency and limb salvage rates for the subgroup of tibial bypass grafts performed for limb salvage indications during the entire period. Again, significant improvement in the long-term limb salvage rate was found, with a trend toward improved secondary patency (55 ± 8% in group 1 vs. 69 ± 5% in group 4, P < .06) as well.
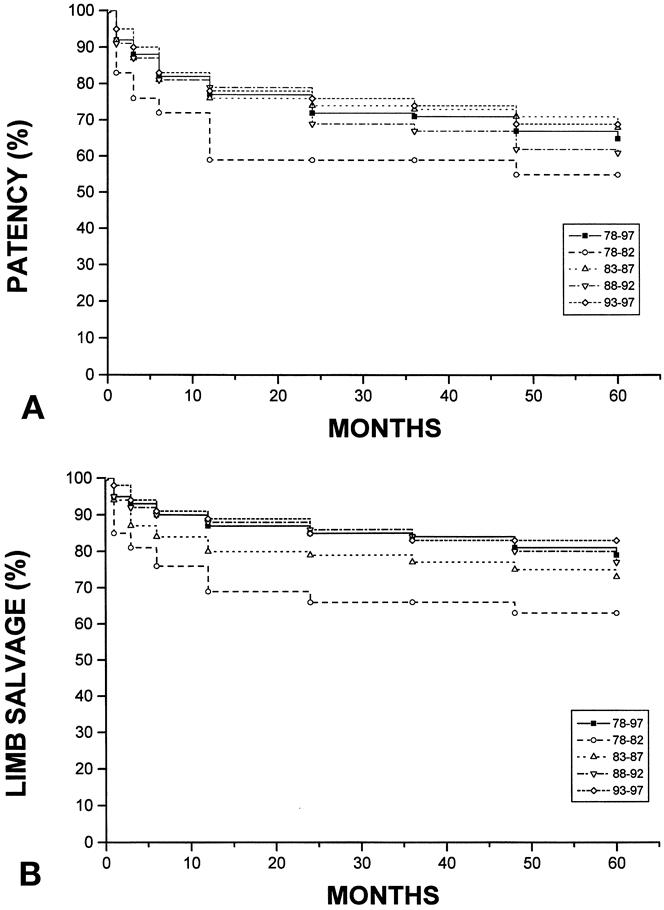
Figure 4. Cumulative secondary patency (A) and limb salvage (B) rates for tibial bypass grafts performed for limb salvage indications during a 20-year period.
Length of Stay
Length of stay (LOS) data were available for comparison in the last two intervals. Figure 5 shows an overall 25% reduction in LOS for group 4 (mean 11.7 ± 0.4 days, median 9) compared with group 3 (mean 15.7 ± 0.8, median 11;P < .001). The improvement was seen across virtually all subgroups but was particularly pronounced for procedures undertaken for tissue necrosis (mean LOS 14.6 ± 0.7 vs. 21.2 ± 1.8 days, group 4 vs. group 3;P < .001). Among patients in the most recent cohort (group 4), mean LOS was also significantly affected by dialysis-dependent renal failure (15 days for dialysis patients vs. 11 days, P < .001) and the level of the distal anastomosis (10 days for below-knee popliteal grafts vs. 13 days for tibial grafts, P < .01). Age was not a significant modifier of LOS.
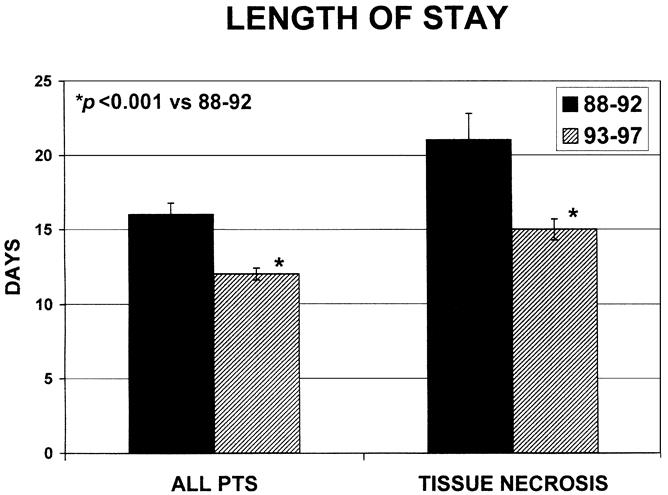
Figure 5. Mean hospital length of stay for patients undergoing autogenous lower extremity arterial reconstruction during the last two consecutive 5-year intervals. The tissue necrosis subgroup is composed of patients with ulceration, gangrene, or both.
DISCUSSION
Our results showed that despite a changing patient population with increased comorbidity, more advanced ischemia, and a need for greater technical complexity, the safety, durability, and effectiveness of autogenous LER are maintained. In our institution, autogenous LER remains the benchmark against which all other interventions for infrainguinal occlusive disease are measured.
Our data showed an unequivocal shift in patients undergoing LER in our practice, characterized by increasing age, an increased proportion of women, and a higher prevalence of diabetes mellitus and renal disease. Of these comorbid factors, we and others have previously observed a negative impact of renal insufficiency on outcomes of LER. 11 Although the literature is consistent regarding a lack of significant effect of diabetes and advanced age on LER results, the question of gender-based differences in outcome remains controversial. 12,13 In a prior report, we found no significant association between gender and major adverse events. 3 The reasons for the observed changes in the population treated at our institution are likely to be multifactorial and remain speculative. Nationwide trends of an increasing prevalence of type 2 diabetes and an associated increase in the prevalence of diabetic nephropathy have been documented. 14 Of particular interest is the increased proportion of patients with tissue necrosis, in whom additional procedures and a prolonged hospital stay are generally necessary to achieve limb salvage.
Despite a clear trend of increasing surgical complexity in older patients with more frequent comorbidities, the perioperative death rate remained low (2%) and unchanged throughout the two decades of study. During these two decades, the strategies for preoperative evaluation and perioperative management in our institution have undergone considerable evolution. Currently, the emphasis of preoperative cardiac evaluation is a careful clinical assessment, with a minority of LER patients undergoing provocative testing or cardiac catheterization. Pharmacotherapy with beta-adrenergic blocking agents for control of blood pressure and heart rate is a cornerstone of medical management in all patients who do not have specific contraindications. Virtually all patients are receiving antiplatelet therapy, usually aspirin, before surgery. Both general and regional anesthetic techniques are commonly used, with hemodynamic monitoring in selected patients. Postoperative anticoagulation is rarely prescribed in the absence of other indications, and dextran therapy is used infrequently in our practice.
The type of autogenous conduit used showed significant variations depending on the surgical preference of the particular period and, increasingly, lack of available greater saphenous vein. Whereas reversed greater saphenous vein represented 95% of vein grafts in group 1, a local preference for the in situ configuration was clear in the intervals from 1983 to 1992. More recent trends have included an increased reliance on nonreversed greater saphenous vein (38% in group 4) and an increase in ectopic and composite vein grafts to nearly 20% of all cases in the last interval. The increase in ectopic/composite vein grafts is particularly notable in light of the fact that the proportion of redo procedures remained approximately 20% throughout all four intervals; hence, this does not simply reflect an increase in secondary bypass grafts. Although we did not specifically determine the reason for the use of ectopic/composite vein in these cases, the nearly parallel increase in frequency of prior coronary artery bypass grafting suggests that this is likely to be at least one important contributing factor. Because the overall patency rates were not significantly different throughout the four intervals, these data may be considered to support the concept that graft configuration (i.e., reversed vs. in situ, vs. nonreversed, translocated) is of relatively minor importance compared with other patient and procedural variables.
In addition to an increased requirement for ectopic and composite vein grafts, patients in group 4 more frequently required bypass to distal (tibial, pedal) outflow sites in the setting of advanced ischemia and tissue necrosis. This reflects an increasing confidence in the outcomes of distal bypass for limb salvage when autogenous conduit is available. Indeed, despite this growing proportion of tibial grafts to nearly 70% in group 4, patency and limb salvage rates were maintained overall and improved in the subset of distal grafts. The results support a continued aggressive approach to this challenging subset of patients.
The observed shifts in case mix have clear implications for surgical workload and resource utilization in both the inpatient and outpatient setting. The increasing frequency of presentation with tissue necrosis is reflected by the substantial increase in associated minor amputations required in the most recent interval. We did not obtain data on total outpatient visits, wound care, requirement for nursing services, or actual costs (hospital or clinic) associated with LER throughout this series. Unquestionably, all these parameters would be expected to be greatly increased, given the more complex population in group 4. We also did not obtain accurate functional outcomes data on quality of life and health perception for these patients in a retrospective fashion. Such data, obtained prospectively, will be critical as we continue to evaluate the optimal management strategy for older, more debilitated patients.
In conclusion, we observed a profound shift in the population of patients and procedures used to treat lower extremity arterial occlusive disease in our tertiary hospital-based vascular practice during the past two decades. Excellent short-term and long-term outcomes can be achieved in most patients with an aggressive approach relying on autogenous vein conduit for LER. Increasing comorbidities and surgical complexity will require a continuing evaluation of actual resource utilization and costs to attempt to offset a negative balance from declining reimbursement, particularly in the context of capitated systems.
Acknowledgments
The authors thank Ms. Julie Lombarra for maintenance of the vascular registry, retrieval of data, and statistical analyses.
Footnotes
Correspondence: Michael S. Conte, MD, Brigham and Women’s Hospital, 75 Francis St., Boston, MA 02115.
E-mail: mconte@partners.org
Accepted for publication October 9, 2000.
References
- 1.U. S. Bureau of the Census. Statistical Abstract of the United States: 1993. 113th ed. Washington, DC: U.S. Government Printing Office; 1993:91.
- 2.Taylor LM Jr, Edwards JM, Porter JM. Present status of reversed vein bypass grafting: five-year results of a modern series. J Vasc Surg 1990; 11: 193–206. [DOI] [PubMed] [Google Scholar]
- 3.Belkin M, Conte MS, Donaldson MC, et al. The impact of gender on the results of arterial bypass with in-situ greater saphenous vein. Am J Surg 1995; 170: 97–102. [DOI] [PubMed] [Google Scholar]
- 4.Shah DM, Darling CD, Chang BB, et al. Long-term results of in situ saphenous vein bypass: analysis of 2058 cases. Ann Surg 1995; 222: 438–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kent KC, Whittemore AD, Mannick JA. Short-term and midterm results of an all-autogenous tissue policy for infrainguinal reconstruction. J Vasc Surg 1989; 9: 107–14. [DOI] [PubMed] [Google Scholar]
- 6.Donaldson MC, Whittemore AD, Mannick JA. Further experience with an all-autogenous tissue policy for infrainguinal reconstruction. J Vasc Surg 1993; 18: 41–8. [DOI] [PubMed] [Google Scholar]
- 7.Donaldson MC, Mannick JA, Whittemore AD. Femoral-distal bypass with in situ greater saphenous vein. Long-term results with the Mills valvulotome. Ann Surg 1991; 213: 457–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belkin M, Knox J, Donaldson MC, et al. Infrainguinal arterial reconstruction with nonreversed greater saphenous vein. J Vasc Surg 1996; 24: 957–62. [DOI] [PubMed] [Google Scholar]
- 9.Rutherford RB, Flanigan DP, Gupta SK, et al. Suggested standards for reports dealing with lower extremity ischemia. J Vasc Surg 1986; 4: 80–94. [PubMed] [Google Scholar]
- 10.Greenwood M. The natural duration of cancer. In: Reports on public health and medical subjects, no 33. London: His Majesty’s Stationary Office; 1926.
- 11.Whittemore AD, Donaldson MC, Mannick JA. Infrainguinal reconstruction for patients with chronic renal insufficiency. J Vasc Surg 1993; 17: 32–41. [DOI] [PubMed] [Google Scholar]
- 12.Magnant JG, Cronenwett JL, Walsh DB, et al. Surgical treatment of infrainguinal arterial occlusive disease in women. J Vasc Surg 1993; 17: 67–78. [PubMed] [Google Scholar]
- 13.Harris EJ, Taylor LM Jr, Moneta GL, et al. Outcome of infrainguinal arterial reconstruction in women. J Vasc Surg 1993; 18: 627–636. [DOI] [PubMed] [Google Scholar]
- 14.Ritz E, Orth SR. Primary care: nephropathy in patients with type 2 diabetes mellitus. N Engl J Med 1999; 341: 1127–1133. [DOI] [PubMed] [Google Scholar]