Abstract
Objective
To evaluate the effect of recurrent nerve dissection on the incidence of recurrent laryngeal nerve injury (RLNI) and to analyze the performance of individual surgeons.
Summary Background Data
Dissection of the recurrent nerve is mandatory in total thyroidectomy, but its relative merit in less extensive resections is not clear. The reported rates of RLNI differ widely; this may reflect a variation in the performance of individual surgeons.
Methods
The authors studied the incidence of RLNI in primary surgery for benign thyroid disease during three periods in a single center. In period 1 (1979–1990; 9,385 consecutive patients, 15,865 nerves at risk), the recurrent nerve was not exposed. In period 2 (1991–1998; 6,128 patients, 10,548 nerves at risk), dissection of the recurrent nerve was the standard procedure. Global outcome and individual performance in these two periods were compared and presented to the surgeons. The effect of this quality control procedure was tested in 1999 (period 3; 930 patients, 1,561 nerves at risk).
Results
Exposure of the recurrent nerve significantly reduced the global rate of postoperative and permanent RLNI. Some but not all surgeons improved their results by recurrent nerve dissection (e.g., permanent RLNI rates ranged from 0% to 1.1%). The documented significant differences in individual performances did not affect the outcome in period 3. The extent of nerve dissection was a source of variability; the rate of permanent RLNI averaged 0.9%, 0.3%, and 0.1% for surgeons who only localized, partially exposed, and completely dissected the recurrent nerve, respectively.
Conclusions
Recurrent nerve dissection significantly reduces the risk of RLNI. Extensive dissection facilitates visual control of nerve integrity during resection and is therefore superior to a more limited exposure of the nerve. Quality control can improve the global outcome and identify the variability in individual performance. This cannot be eliminated by merely confronting surgeons with comparative data; hence, it is important to search for the underlying causes.
Evidence-based medicine provides a rational framework for delivering optimal healthcare. Guidelines that aim at better therapeutic approaches require analysis of outcomes; improving patient care also implicitly requires quality control. Quality control is rigorously enforced for commercially available drugs and is also common for laboratory tests. In contrast, other medical services are not subject to formal control. Hence, the ultimate decision on acceptable standards in medical practice is left to the courts. Every patient aspires to obtain the best possible care by a physician, and healthcare professionals aim at providing this service, although it is sometimes difficult to define. 1 Similarly, educational efforts and training programs aim at evaluating and improving the performance of individual actors in the healthcare system. 2,3 Nevertheless, in many instances, a cause-and-effect relation between the performance of an individual physician and the eventual outcome is difficult to assess. Thus, results may be compared only between treatment groups, and the contribution of individuals is inaccessible to analysis. In many cases, quality improvement is therefore process-oriented and aims at implementing better guidelines. 3–8 It is a matter of debate whether this strategy can identify and remedy individual shortcomings. In contrast, in surgery, many complications can readily be linked to the surgical procedure, and a clear-cut cause-and-effect relation is beyond reasonable doubt. This is exemplified by complications such as postoperative bleeding, leakage at the sites of anastomosis, relapses after surgery for inguinal hernias, and so forth.
Thyroid surgery clearly provides a unique opportunity to evaluate the performance of individual surgeons because it is associated with the risk of a well-defined complication: recurrent laryngeal nerve injury (RLNI). This complication can result only from surgery, is readily diagnosed based on objective criteria by an independent expert (ear-nose-throat specialist), and is a major cause of problems. Clearly, the goal in thyroid surgery is to avoid recurrent nerve palsy by refining the surgical technique, and this goal is the standard against which the outcome at any given time is to be compared. In the present study, we used a large database from a single department and evaluated the effectiveness of quality control in improving the surgical technique and in assessing the performance of individual surgeons. Our analysis showed that the global outcome within a department helps to define a standard with reference to published data. In addition, surgeons whose complication rates are significantly higher can be identified and their surgical procedures can be analyzed to eliminate individual shortcomings. Finally, based on the analysis of more than 27,000 nerves at risk, we conclude that careful dissection of the nerve essentially eliminates the major complication (permanent recurrent nerve palsy) in thyroid surgery for benign disease. Surgical approaches that do not expose the recurrent laryngeal nerves cannot be recommended.
PATIENTS AND METHODS
Patients
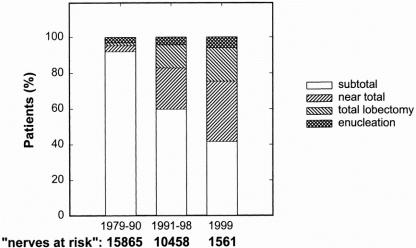
We studied the incidence of RLNI in primary surgery for benign thyroid disease during three periods in a single center. In period 1 (1979–1990), 9,385 consecutive patients (7,870 women, 1,515 men; age at the time of surgery 49.5 ± 14.2 years [range 9–91]) underwent thyroid surgery; in this period, the recurrent laryngeal nerve was not exposed in benign disease. In period 2 (1991–1998), 6,128 patients (5,006 women, 1,122 men; age at the time of surgery 52.8 ± 13.7 years [range 11–91]) underwent thyroid surgery; in this period, dissection of the recurrent nerve was considered the standard procedure in all operations, and patient data were collected prospectively. After an analysis of the outcome in these two periods, the results were presented to the surgeons at the beginning of 1999. In period 3 (1999), the incidence of RLNI was evaluated in 930 patients (724 women, 206 men; mean age 53.2 ± 13.6 years [range 13–86]). Figure 1 gives an overview of the surgical procedures in the three periods.
Figure 1. Distribution of patients in the three study periods according to the extent of resection. Subtotal lobectomy and near-total lobectomy refer to remnant sizes of 2 to 4 g and 1 g or less, respectively. In total lobectomy, no residual tissue is left; enucleation is the localized removal of a circumscribed pathologic lesion. The proportion of extensive resections increased in periods 2 and 3.
Austria is an area of endemic iodine deficiency, with a comparatively high incidence of thyroid disease. The diagnoses and indications for surgery were euthyroid multinodular goiter (mechanical obstruction/suspect nodule; 54.1% in period 1 and 56.6% in period 2), euthyroid solitary nodule (cold nodule; 14.1% in period 1 and 13.6% in period 2), unifocal autonomous adenoma (18.6% in period 1 and 17.3% in period 2), multifocal autonomous disease (11.6% in period 1 and 7.5% in period 2), and Graves disease (1.6% in period 1 and 4.9% in period 2). The diagnosis of Graves disease was based on the detection of antibodies directed against the TSH-receptor and/or endocrine ophthalmopathy. The proportion of Graves disease increased (at the expense of multifocal autonomous disease) because the sensitivity of the laboratory determination increased. In case of suspect nodules, the tissue was removed and a cancer operation was started only after the histologic (frozen-section) diagnosis. Patients undergoing a cancer operation were not included in the current analysis because our standard procedure includes removal of the thyroid and the paratracheal and jugular lymph nodes, a procedure with an inherently greater risk of RLNI. Inflammatory disease was defined based on laboratory findings and histopathologic criteria (presence of lymphocytic infiltration). Regardless of the underlying cause, the presence of thyroid inflammation (Graves disease vs. other inflammatory diseases) did not result in an increased risk of RLNI (not shown).
Perioperative Management and Follow-Up
Apart from routine laboratory determinations, 9 patient evaluation included sonography, scintigraphy, and, when appropriate, needle aspiration. All patients were evaluated before and after surgery (day 3 or 4 after surgery) for vocal cord function by laryngoscopy (indirect laryngoscopy with a mirror or direct laryngoscopy with a flexible endoscope if indirect laryngoscopy was not feasible; both were carried out by an ear-nose-throat specialist). If postoperative nerve injury occurred, follow-up examinations were performed on day 14 and after 2 to 3, 6, and 12 months. Palsy (lack of mobility) on day 3 to 4 was classified as RLNI irrespective of whether it recovered rapidly or slowly; reduced mobility on the first examination was left unclassified and reinvestigated after 10 days. If the reduced mobility persisted, the patient was considered to have RLNI. Patients in whom the second examination showed normal mobility were not classified as having RLNI. RLNI that did not resolve within the first 12 months were classified as permanent RLNI. Recovery of vocal cord function was, in fact, adequately described by a monoexponential rise with a half-life of about 1.7 months (i.e., 50% of the patients had recovered within 1.7 months).
Statistical Analysis
Starting with 1979, the diagnostic findings, surgical procedures, surgical team, complications, and follow-up findings for every patient were entered by physicians into a computerized documentation system (MediCare ChirDok system from Micom, Wiener Neustadt, Austria) that was adapted for the specific requirements of thyroid surgery. The data (including key laboratory parameters and demographic information) were stored in codified form; a built-in subroutine detects incompatible entry errors. Entries were independently double-checked by physicians. The system allows for data retrieval and evaluation by user-defined algorithms and thus supports the efficient analysis of large data sets. Statistical differences between treatment groups were evaluated by the chi-square test. Where appropriate, the homogeneity of binomial distributions was analyzed by contingency tables according to Brandt and Snedecor. To account for the different types of operations (unilateral and bilateral procedures), we present the data based on the number of nerves at risk.
RESULTS
Period 1
Between 1979 and 1990, 9,385 patients (corresponding to 15,865 nerves at risk) were treated by 11 surgeons (numbers 1–11 in Table 1) and by guest surgeons (summarized as number 12 in Table 1) who visited for training purposes. The routine procedure did not include recurrent nerve dissection. The average rate of postoperative and permanent nerve injury was comparable to that reported in the literature, but three arguments led to the conclusion that recurrent nerve exposure ought to be mandatory in surgery for benign diseases. First, the analysis of complication rates showed that the incidence of nerve injury increased with the extent of thyroid resection. 10 This can also be seen from the data in Figure 2, where total lobectomies were found to carry a disproportionate risk of postoperative recurrent nerve palsy. It is obviously not possible to carry out a total lobectomy without encountering the recurrent laryngeal nerve. Second, reports in the literature indicated that recurrent nerve exposure did not increase the risk of primary palsy, 11 although this was questioned by others. 12 Third, it is evident from Table 1 that there were large differences between individual surgeons within the department, resulting in a nonhomogeneous binomial distribution (chi-square = 84.55, P < .001). The number of patients was too large for these discrepancies to result from variable levels of experience. Rather, the data suggested that there were fundamental differences in the surgical technique of individual surgeons. These considerations led to the conjecture that the recurrent nerves were subjected to a variable risk of injury because they were not exposed. This is substantiated by the variable recovery rate, which ranged from 33% to 85%.
Table 1. RECURRENT LARYNGEAL NERVE (RLN) INJURY IN PERIOD 1
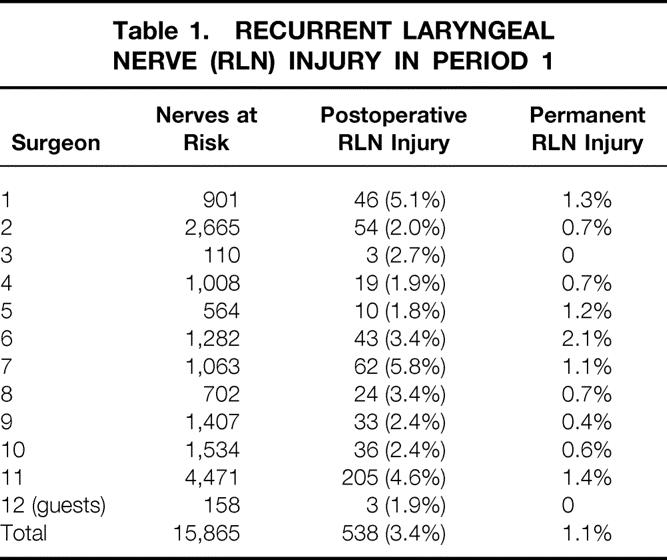
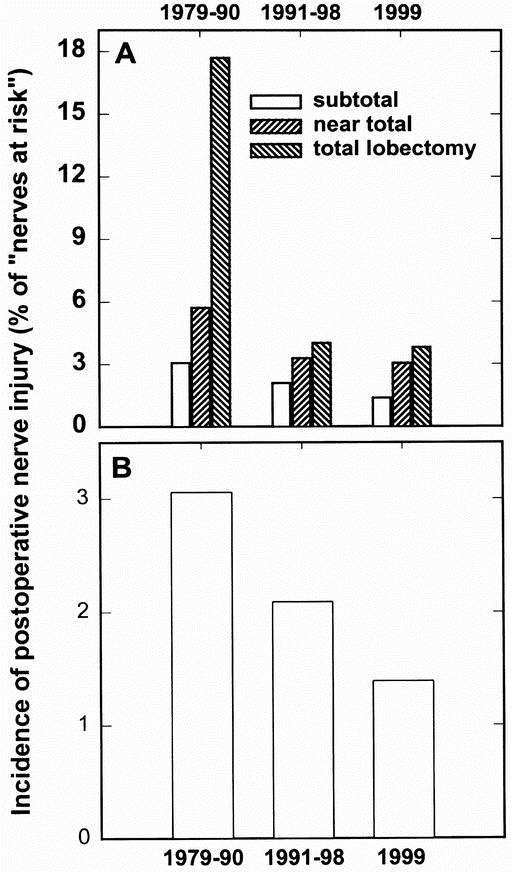
Figure 2. Incidence of postoperative recurrent nerve injury without nerve exposure (period 1, 1979–1990) and with nerve exposure (period 2, 1991–1998, and period 3, 1999). (A) Extensive resections were associated with a higher risk of recurrent nerve injury, in particular in period 1, when the recurrent nerve was not exposed. For subtotal resections there were 14,619, 6,263, and 651 nerves at risk in periods 1, 2, and 3; for near-total lobectomies, the corresponding numbers were 524, 2,412, and 529 nerves at risk. For total lobectomies there were 260, 1,343, and 291 nerves at risk. In all three types of resections, the incidence of recurrent nerve injury declined significantly (P < .01) if period 1 (no nerve exposure) was compared with period 2 (surgery with nerve exposure). (B) The data for subtotal resections have been redrawn with an expanded y-axis to illustrate the significant effect of nerve exposure (P < .001, period 1 vs. 2).
Hence, at the end of 1990, the decision was made in the department that the surgical approach was to include recurrent nerve exposure in all thyroid operations (except those confined to the thyroid isthmus). The stated goal was to allow unambiguous identification of the nerve, but the extent of dissection was not explicitly defined.
Period 2
In period 2, the incidence of recurrent nerve injury (transient and permanent) declined (Table 2), although the proportion of more extended resections increased (see Fig. 1). During period 2, near-total (with thyroid remnants ≤2 g) and total thyroidectomies were found to yield superior results in the management of hyperthyroidism. 13 In addition, exposure of the recurrent laryngeal nerve allowed total removal of dorsal nodules in multinodular goiter. These two factors accounted for the higher proportion of near-total resections and lobectomies. A separate comparison taking into account only the subtotal resections shows that the incidence of recurrent nerve palsy declined significantly from 1991 to 1998 (see Fig. 2; chi-square = 15.58, P < .001); the same holds true if the more radical approaches (near-total and total lobectomies) are separately compared. Finally, the incidence of postoperative bilateral nerve injury, the most dreaded complication, decreased with recurrent nerve exposure (Fig. 3). Because of the low incidence, the difference did not reach the level of statistical significance (chi-square = 3.58, P = .058). If the additional 631 patients who underwent bilateral resection in 1999 were included in the statistical comparison, the difference between the two groups (surgery with and without recurrent nerve exposure) was significant (P = .05). Based on these findings, we conclude that the overall results were improved by recurrent nerve dissection.
Table 2. RECURRENT LARYNGEAL NERVE (RLN) INJURY IN PERIOD 2
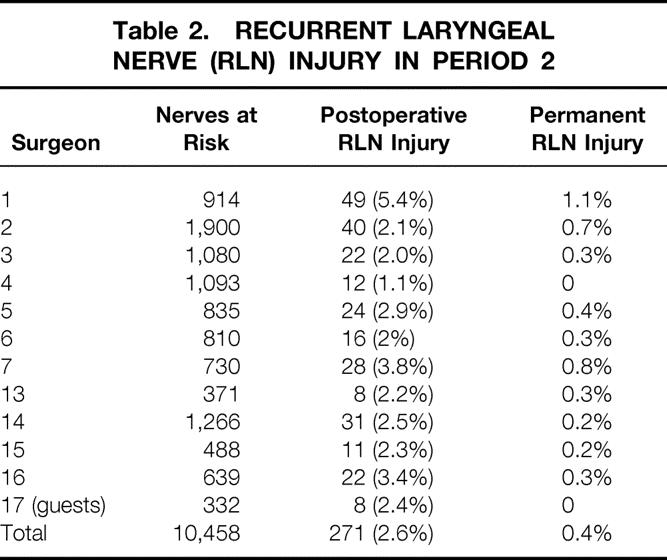
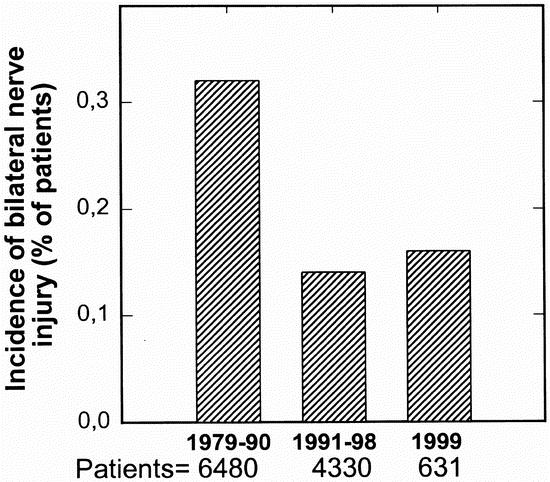
Figure 3. Incidence of postoperative bilateral recurrent nerve injury without nerve exposure (period 1, 1979–1990) and with nerve exposure (period 2, 1991–1998, and period 3, 1999). Nerve exposure resulted in a decline in the incidence of bilateral vocal cord paralysis. Statistical significance was reached only if the data for the two periods with nerve exposure (periods 2 and 3) were combined and compared with period 1. The comparison between period 1 and period 2 gave P = .058.
Effect of Surgeon on Outcome
When the performance of individual surgeons was analyzed based on the incidence of RLNI (see Table 2), the binomial distribution was again not homogeneous (chi-square = 48.97, P < .001). Thus, the outcome still significantly depended on the surgeon. Six surgeons were further evaluated in detail based on the following criteria: they had been present throughout both periods and had performed a large number of operations in each period (>500 nerves at risk), with the number of operations varying by no more than 1.5-fold in the two periods. The outcome improved in four surgeons (Fig. 4). A closer inspection of the data showed that in surgeons 4, 5, and 6, the incidence of permanent palsy declined; this improvement was more pronounced than the decline in the global average. The performance of surgeon 7 was also better in the second period, but this improvement was still less than desirable because the rate of nerve palsy clearly exceeded the global average. For two surgeons, no improvement was noted, and the incidence of primary palsy and the recovery rate did not change. Nevertheless, these two surgeons differed in an important way. Surgeon 1 had a high rate of postoperative nerve injury, but the incidence of recurrent nerve palsy in surgeon 2 was lower than the global average; however, vocal cord function recovered poorly in patients treated by this surgeon. This is readily evident if surgeon 2 is compared with surgeon 3 (who was excluded from the interperiod comparison because the numbers of operations in the two periods differed widely). The rates of postoperative paresis were comparable (about 2%), but the recovery rate was 67% (27/40) for surgeon 2 and 86% (19/22) for surgeon 3.
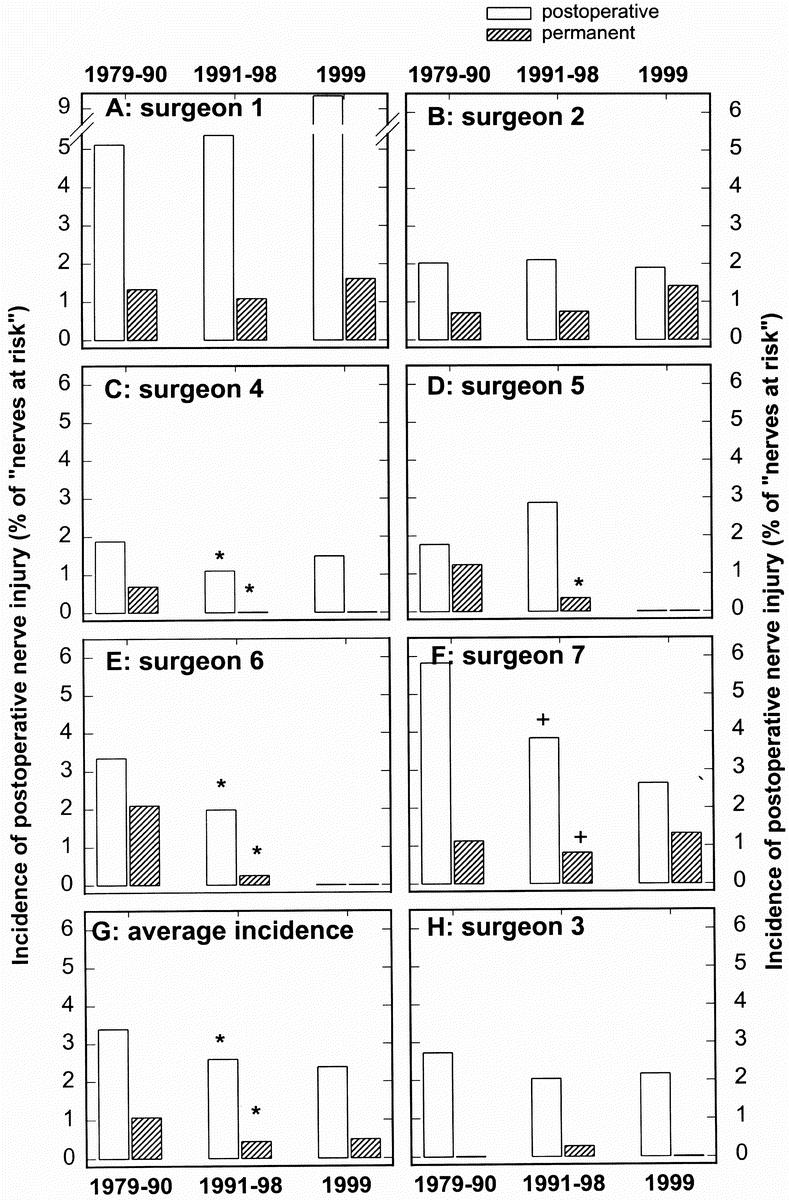
Figure 4. Comparison among seven surgeons of the incidence of postoperative and permanent recurrent nerve palsy without nerve exposure (period 1, 1979–1990) and with nerve exposure (period 2, 1991–1998, and period 3, 1999). There was a significant improvement between periods 1 and 2 (*P < .05) for surgeons 4, 5, and 6; in surgeon 7, the level of significance was reached only if the combination of periods 2 and 3 was compared (+P < .05); for the comparison of periods 1 and 2, P = .056 was calculated. (G) Global average as shown in Tables 1 to 3.
The size of the diseased thyroid obviously has an impact on outcome. We found that the risk of RLNI increased with the size of the resected thyroid tissue. However, the sizes of the resected specimen did not differ appreciably in periods 1 and 2: in 60.8% in period 1 and 58.9% in period 2 the mass of the resected tissue was 50 g or less, in 25.4% and 26.1% it was 50 to 100 g, in 7.9% and 8.4% it was 101 to 150 g, in 3.4% and 3.7% it was 151 to 200 g, in 1.5% and 1.7% it was 201 to 250 g, and in 1.1% and 1.3% it was more than 251 g. A similar analysis was carried out for each surgeon subjected to a detailed comparison (surgeons 1–7). These surgeons did not differ whether they were compared by the size of the resected specimen or by the distribution of diagnoses (data not shown). We conclude that neither size nor diagnosis was a variable that confounded our analysis.
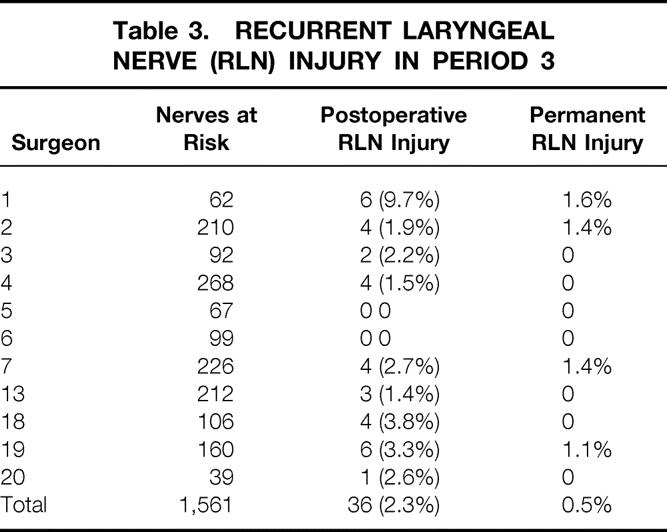
Period 3
At the end of 1998, the number of operations approached that of period 1. Therefore, the statistical analysis summarized above was carried out. The surgeons were informed of the outcome in their personal series, of the results of all other surgeons (anonymously), and of the global average. This comparison was chosen to allow each surgeon to draw conclusions with respect to her or his performance. The outcome in 1999 was analyzed at the end of June 2000. All patients in whom vocal cord mobility was abnormal at this time were considered to have permanent recurrent nerve palsy. The mere presentation of the data to the surgeons did not result in any further appreciable improvement in the global performance (Table 3).The surgeons who had achieved good results in period 2 (numbers 3–6) clearly achieved excellent results (no permanent nerve injury). In contrast, for surgeons whose performance was lower than average, the improvement was essentially confined to the results of surgeon 7; in this case, the rate of postoperative RLNI declined significantly (chi-square = 6.06, P < .05), but the rate of permanent palsy was still high. During 1999, the surgical procedure of surgeon 1 was evaluated by colleagues and he agreed to a different assignment. Finally, the performance of surgeon 2 continued to be good (below the global average) with respect to the incidence of postoperative nerve injury, but the recovery rate remained poor. This observation prompted an investigation into the surgical procedures used by all surgeons. On questioning both the surgeons and their team, it was noted that surgeons 4 and 6 exposed the recurrent nerve over its entire cervical course, surgeons 3 and 5 dissected the nerve in the vicinity of the inferior thyroid artery, and surgeons 1, 2, and 7 only localized the nerve. Based on this evaluation, we compared the patients in these three groups and found that the incidence of permanent nerve injury was 0.86% (35 of 4,042 nerves at risk), 0.29% (6 of 2,074 nerves at risk), and 0.09% (2 of 2,270 nerves at risk) if the nerves were only localized, partially exposed, and completely dissected, respectively.
Table 3. RECURRENT LARYNGEAL NERVE (RLN) INJURY IN PERIOD 3
DISCUSSION
Despite many excellent studies, 11,14 the merit of recurrent nerve dissection has repeatedly been questioned because there was no change 15–18 or an increase in the risk of vocal cord paralysis. 12 Several of these studies concluded that recurrent nerve dissection is not mandatory in subtotal resection but advocate the procedure for the sake of practice that will be useful in complicated cases (e.g., thyroid cancer). The ethical basis for this recommendation is questionable. Our data unequivocally show that nerve dissection does not increase the risk of transient or permanent nerve injury; in contrast, the incidence of recurrent nerve palsy actually declined. We believe that the number of patients in the present study is large enough to support this conclusion in a definitive way. The current analysis also indicates that correct dissection enhances the rate of recovery. The ideal situation is to expose the nerve over its entire cervical course (from the jugular angle to the entry into the larynx); devascularization is best avoided by keeping the nerve surrounded by connective tissue and by avoiding removal of the nerve from its substratum. The improved outcome after complete dissection can be rationalized as follows: total dissection of the recurrent nerve over its entire cervical course precludes an incorrect assignment; it also allows the surgeon to verify the anatomic integrity of the nerve and to identify extralaryngeal ramifications (occurring in 63% to 73% of patients 19,20). This situation is clearly superior to partial exposure of the nerve, a conclusion that is also supported by the poor outcome of surgeons who only aimed at identifying the nerve. Based on the large number of patients, we rule out the validity of the argument that the dissected nerve is per se more vulnerable to permanent injury. In contrast, our observations suggest that vocal cord function generally recovers if the nerves are anatomically intact. This interpretation is based on the personal series of surgeon 4. The extent of dissection is subject to individual variation. However, for surgeon 4, the complete dissection of the nerve over its entire cervical course has been adequately documented by the detailed reports. In this personal series of 1,361 nerves at risk (827 patients), there was not a single case of permanent nerve injury.
It is a truism that every operation is a matter of practice and that learning ought to be associated with a decline in complications. Accordingly, the outcome is improved with the volume of operations performed. 21 This general statement is also true for thyroid surgery. 22 In the current situation, however, we believe that learning curves are not so important to understand our global trends for several reasons. First, the surgeons compared in detail in Figure 3 had performed several hundred operations in each period. They can therefore be considered to have adequate expertise in thyroid surgery. Second, the guest surgeons who came to the department to obtain training had low rates of complications both between 1979 and 1990 (guest surgeons are summarized as number 12 in Table 1) and between 1991 and 1998 (summarized as number 17 in Table 2). This phenomenon is consistent with results from a recent study in which beginners showed low rates of complication because of extensive supervision; the rate of complications increased after 50 operations and learning became manifest by the fact that after 200 operations complication rates were low again. 23 Similar conclusions—that is, that endocrine surgery trainees do not necessarily have higher complication rates than experienced surgeons—were also reached by Mishra et al. 24
Studies that focus on the volume of operations reveal general trends and underline the importance of experience. 21 However, they do not provide insights into variations at the individual level that go beyond surgical volume. Given the variability in manual dexterity, it is highly unlikely that experience per se can remedy poor performance. Our analysis showed a variability in individual performance, although all surgeons had performed a large number of operations. Most importantly, the current study revealed that surgeons differed with respect to their ability (or willingness) to assimilate a refined technique. An improvement is difficult to obtain for several reasons. First, if the number of operations is low, statistical differences cannot readily be shown, and hence it is difficult to obtain convincing arguments in favor of a technical improvement. In the case of thyroid surgery, this issue is exemplified by the fact that the merit of recurrent laryngeal nerve dissection is continuously being questioned 12,15–18 despite numerous earlier studies. 11 Second, trained surgeons consider themselves experts and are reluctant to have their performance compared and controlled at the individual level. This is illustrated by the present study; evidence for the superiority of complete dissection was gathered during the course of our analysis. Each surgeon was allowed to draw his or her conclusions by being exposed to the data that clearly indicated that complete dissection gave superior results. Our (empiric) observations indicate that mandatory policies may not necessarily be assimilated by surgeons because they differ in their definition of what a complete nerve dissection actually is, and that these differences in assessment clearly have repercussions; confronting the surgeons with the results of the evaluation resulted in only marginal changes in surgeons who performed below average. In our study, the three surgeons who performed less well than the others were also the most senior ones. This fact highlights a problem encountered with supervision and retraining, because these surgeons are less likely to accept the advice of younger colleagues (whom they may have trained originally). Nevertheless, for those who achieved good results, the evaluation results in positive reinforcement.
It is obvious that quality management is a process that continuously resets the standard of comparison. Technical innovations aim at minimizing the risks for patients. In the case of thyroid surgery, electrical nerve stimulation (i.e., intraoperative neuromonitoring of vocal cord muscle responsiveness) may represent a significant improvement for technically difficult operations such as those for recurrent disease and thyroid cancer. 25 This approach allows the surgeon to identify ramifications in the recurrent laryngeal nerve and thus provides intraoperative guidance. Preliminary evidence based on electrical stimulation indicates that in the vast majority of patients, the most ventral branch innervates the vocal cord muscles. This branch is obviously most vulnerable to injury by sutures placed on remnant tissue. Nonrecurrent variants (which we estimate to occur with a frequency in the range of 4 in 1,000) can also more readily be identified by neuromonitoring.
The rigorous implementation of standards with respect to acceptable complication rates obviously generates a driving force for further specialization into subdisciplines, but this development is not new. It was already appreciated some 20 years ago 21 and was found to pertain to disciplines other than surgery; complications are inversely related to volume not only in surgery 26 and in invasive procedures 27 but also in medical care. 28 Volume also has a pronounced effect on outcome when analyzed at the level of the individual physician. 29 Finally, evaluations that analyze the performance of individual surgeons may have legal repercussions. Nevertheless, we believe that these difficulties should not detract from the primary goal, which is to improve the quality of care for patients. This can be achieved only if it is based on a sound analysis of unquestionable data. Most surgical procedures have typical complications where a cause-and-effect relation is beyond doubt. We therefore believe that the approach used in the current study has implications that are applicable to many situations and may also be extended to other standardized treatment forms.
Footnotes
Correspondence: Michael Freissmuth, MD, Institute of Pharmacology, University of Vienna, Währinger Strasse 13a, A-1090 Vienna, Austria.
E-mail: michael.freissmuth@univie.ac.at
Accepted for publication June 18, 2001
References
- 1.Blumenthal D. Part 1. Quality of care: what is it? N Engl J Med 1996; 335: 891–894. [DOI] [PubMed] [Google Scholar]
- 2.Holli K, Laippala P, Ojala A, et al. Quality control in health care: an experiment in radiotherapy planning for breast cancer patients after mastectomy. Intl J Radiat Oncol Biol Phys 1999; 44: 827–833. [DOI] [PubMed] [Google Scholar]
- 3.Ayanian JZ, Landrum MB, Normad SL, et al. Rating the appropriateness of coronary angiography: do practicing physicians agree with an expert panel and with each other? N Engl J Med 1998; 338: 1896–1904. [DOI] [PubMed] [Google Scholar]
- 4.Schnelle JF, Cruis PA, Rahman A, et al. Developing rehabilitative behavioral interventions for long-term care: technology transfer, acceptance, and maintenance issues. J Am Geriatr Soc 1998; 46: 771–777. [DOI] [PubMed] [Google Scholar]
- 5.Russel NS, Bartelink H. Radiotherapy: the last 25 years. Cancer Treatment Rev 1999; 25: 365–367. [DOI] [PubMed] [Google Scholar]
- 6.Katz RI, Lagasse RS. Factors influencing the reporting of adverse perioperative outcomes to a quality management program. Anesth Analg 2000; 90: 344–350. [DOI] [PubMed] [Google Scholar]
- 7.Holl RW. Computer programs and data sheets. Initiative of quality control of the German Working Group on Pediatric Diabetology. Hormone Res 1998; 50: 68–73. [DOI] [PubMed] [Google Scholar]
- 8.Hecker W, Grabert Holl RW. Quality of paediatric IDDM care in Germany: a multicentre analysis. German Paediatric Diabetology Group. J Pediatr Endocrinol Metab 1999; 12: 31–38. [DOI] [PubMed] [Google Scholar]
- 9.Hermann M, Richter B, Roka R, et al. Thyroid surgery in untreated severe hyperthyroidism: perioperative kinetics of free thyroid hormones in the glandular venous effluent and peripheral blood. Surgery 1994; 115: 240–245. [PubMed] [Google Scholar]
- 10.Hermann M, Keminger K, Kober F, et al. Risk factors of recurrent nerve palsy: a statistical analysis of 7566 thyroid operations. Chirurgie 1991; 62: 182–188. [PubMed] [Google Scholar]
- 11.Jatzko GR, Lisborg PH, Müller MG, et al. Recurrent nerve palsy after thyroid operations: principal nerve identification and a literature review. Surgery 1994; 115: 139–144. [PubMed] [Google Scholar]
- 12.Friedrich T, Steinert M, Keitel R, et al. The incidence of recurrent laryngeal nerve lesions after thyroid surgery: a retrospective analysis. Zentralbl Chirurgie 1998; 123: 25–29. [PubMed] [Google Scholar]
- 13.Hermann M, Roka R, Richter B, et al. Early relapse after operation for Graves’ disease: postoperative hormone kinetics and outcome after subtotal, near-total and total thyroidectomy. Surgery 1998; 124: 894–900. [PubMed] [Google Scholar]
- 14.Witte J, Simon D, Dotzenrath C, et al. Recurrent nerve palsy and hypocalcemia after surgery of benign thyroid disease. Acta Chir Austria 1996; 28: 361–364. [Google Scholar]
- 15.Bergamaschi R, Becouarn G, Ronceray J, et al. Morbidity of thyroid surgery. Am J Surg 1998; 176: 71–75. [DOI] [PubMed] [Google Scholar]
- 16.Kasemsuwaran L, Nubthuenetr SJ. Recurrent laryngeal nerve paresis: a complication of thyroidectomy. Otorhinolaryngology 1997; 26: 365–367. [PubMed] [Google Scholar]
- 17.Miller W, Buttres M, Leibl, B, et al. Evaluation of thyroid surgery by rate of recurrent nerve palsy. Chirurgie 1995; 66: 1210–1214. [PubMed] [Google Scholar]
- 18.Koch B, Boettcher M, Huschnitt N, et al. Must the recurrent laryngeal nerve be identified routinely during resection of nodular goiter? Chirurgie 1996; 67: 927–932. [Google Scholar]
- 19.Armstrong WG, Hinton JW. Multiple divisions of the recurrent laryngeal nerve: an anatomic study. Arch Surg 1951; 62: 532–539. [DOI] [PubMed] [Google Scholar]
- 20.Katz A, Nemiroff P. Anastomoses and bifurcations of the recurrent laryngeal nerve: report of 1177 nerves visualized. Am Surg 1993; 59: 188–191. [PubMed] [Google Scholar]
- 21.Luft HS, Bunker JP, Enthoven AV. Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med 1979; 301: 1364–1369. [DOI] [PubMed] [Google Scholar]
- 22.Sosa JA, Bowman HM, Tielsch JM, et al. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg 1998; 228: 320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lamadé W, Renz K, Willeke F, et al. Effect of training on the incidence of nerve damage in thyroid surgery. Br J Surg 1999; 86: 388–391. [DOI] [PubMed] [Google Scholar]
- 24.Mishra A, Agarwal G, Agarwal A, Mishra SK. Safety and efficacy of total thyroidectomy in hands of endocrine surgery trainees. Am J Surg 1999; 178: 377–380. [DOI] [PubMed] [Google Scholar]
- 25.Jonas J, Bähr R. Intraoperative electromyographic identification of the recurrent laryngeal nerve. Chirurg 2000; 71: 534–538 [DOI] [PubMed] [Google Scholar]
- 26.Begg CB, Cramer LD, Hoskins WJ, Brenna MF. Impact of hospital volume on operative mortality formajor cancer surgery. JAMA 1998; 280: 1747–1751. [DOI] [PubMed] [Google Scholar]
- 27.Jollis JG, Peterson ED, DeLong ER, et al. The relation between the volume of coronary angioplasty procedure at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med 1994; 331: 1625–1629. [DOI] [PubMed] [Google Scholar]
- 28.Thiemann DR, Coresh J, Oetgen WJ, et al. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med 1999; 340: 1640–1648. [DOI] [PubMed] [Google Scholar]
- 29.Jollis JG, Peterson ED, Nelson CL, et al. The relationship between physician and hospital coronary angioplasty volume and outcome in treating elderly patients. Circulation 1997; 95: 2485–2491. [DOI] [PubMed] [Google Scholar]