Abstract
Objective
To assess the therapeutic value of Gastrografin in the management of adhesive small bowel obstruction after unsuccessful conservative treatment.
Summary Background Data
Gastrografin is a hyperosmolar water-soluble contrast medium. Besides its predictive value for the need for surgery, there is probably a therapeutic role of this contrast medium in adhesive small bowel obstruction.
Methods
Patients with clinical evidence of adhesive small bowel obstruction were given trial conservative treatment unless there was suspicion of strangulation. Those who responded in the initial 48 hours had conservative treatment continued. Patients showing no clinical and radiologic improvement in the initial 48 hours were randomized to undergo either Gastrografin meal and follow-through study or surgery. Contrast that appeared in the large bowel within 24 hours was regarded as a partial obstruction, and conservative treatment was continued. Patients in whom contrast failed to reach the large bowel within 24 hours were considered to have complete obstruction, and laparotomy was performed. For patients who had conservative treatment for more than 48 hours with or without Gastrografin, surgery was performed when there was no continuing improvement.
Results
One hundred twenty-four patients with a total of 139 episodes of adhesive obstruction were included. Three patients underwent surgery soon after admission for suspected bowel strangulation. Strangulating obstruction was confirmed in two patients. One hundred one obstructive episodes showed improvement in the initial 48 hours and conservative treatment was continued. Only one patient required surgical treatment subsequently after conservative treatment for 6 days. Thirty-five patients showed no improvement within 48 hours. Nineteen patients were randomized to undergo Gastrografin meal and follow-through study and 16 patients to surgery. Gastrografin study revealed partial obstruction in 14 patients. Obstruction resolved subsequently in all of them after a mean of 41 hours. The other five patients underwent laparotomy because the contrast study showed complete obstruction. The use of Gastrografin significantly reduced the need for surgery by 74%. There was no complication that could be attributed to the use of Gastrografin. No strangulation of bowel occurred in either group.
Conclusions
The use of Gastrografin in adhesive small bowel obstruction is safe and reduces the need for surgery when conservative treatment fails.
Adhesive small bowel obstruction remains a leading cause of hospital admission. The natural course of this clinical problem is still unclear. Patients with this condition are often difficult to assess and require careful evaluation and management. Immediate surgery is recommended when strangulation is suspected or in complete bowel obstruction. 1 A trial of conservative treatment is acceptable if the obstruction is incomplete. 2,3 However, the optimal duration of this trial of conservative treatment has not been well defined.
The role of water-soluble contrast medium in adhesive small bowel obstruction has been evaluated recently. Studies have documented a diagnostic value of this contrast medium in assessing the need for surgical treatment. 4–7 A possible therapeutic effect of this agent has also been suggested, but the efficacy is still controversial. 8–11 Gastrografin (Schering AG, Berlin, Germany) is the water-soluble contrast medium that has been most commonly studied. This prospective randomized study aimed to examine objectively the therapeutic role of Gastrografin in adhesive small bowel obstruction for patients who failed to respond to conservative treatment.
METHODS
Patients
Patients older than 16 years of age admitted through the emergency room to the Department of Surgery, University of Hong Kong Medical Centre, Queen Mary Hospital, with clinical and radiologic evidence of adhesive small bowel obstruction were included in this study. Patients with documented intraabdominal malignancy, inflammatory bowel disease, or history of abdominal irradiation were excluded. A detailed history, including information on previous abdominal surgery and adhesive obstruction, was taken and a complete physical examination was performed for every patient. A nasogastric tube was inserted for decompression, with strict measurement of output. Intravenous fluid replacement was given and electrolyte imbalances were corrected as required. Supine and erect abdominal radiographs were taken and the maximal diameter of the small bowel was measured on admission.
Management Plan
Emergency laparotomy was performed for patients with suspected bowel strangulation. Those without suspicion of bowel strangulation were treated conservatively, with close monitoring of vital and abdominal signs and daily abdominal radiographs. Patients with obstruction that improved clinically or radiologically in the initial 48 hours continued to receive conservative treatment. Clinical improvement was defined as the presence of decreased abdominal pain, distention, tenderness, or nasogastric tube output, or bowel opening if the patient had constipation on admission. Radiologic improvement was defined as a decrease in the number of dilated bowel loops or in the diameter of dilated small bowel.
Patients who showed neither clinical nor radiologic improvement within 48 hours were considered to have failed conservative treatment and were randomized to undergo either laparotomy or Gastrografin meal and follow-through study. Randomization was accomplished by opening an envelope. The Gastrografin study was performed by a radiologist after informed consent was obtained. One hundred milliliters Gastrografin was administered through a nasogastric tube, and the transit of the contrast was followed by fluoroscopy and serial abdominal radiographs. Patients in whom contrast appeared in the large bowel within 24 hours were regarded as having partial obstruction, in which the obstructing site could still allow the passage of a small amount of gas and fluid. Conservative treatment was continued for these patients. If contrast failed to reach the large bowel within 24 hours, the patient was regarded as having complete obstruction; these patients proceeded to laparotomy. Patients who showed no progressive clinical and radiologic improvement after 48 hours, either in the Gastrografin group or in the group solely managed by conservative treatment, also underwent surgery.
Complete resolution of bowel obstruction was established when the symptoms and signs of obstruction subsided and abdominal radiographs showed no dilated small bowel. A liquid diet was then started. A soft diet was usually given the next day, and solid food the day after. Patients were discharged when solid food was well tolerated. Complications, death rates, and hospital stays were recorded. A flow chart illustrating the management plan in the study is shown in Figure 1.
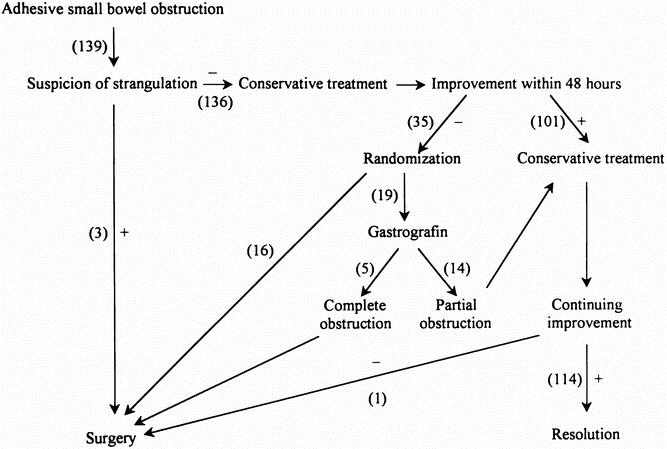
Figure 1. Study protocol.
Statistical Analysis
Data were prospectively collected and entered into a computer database. SPSS software (SPSS Inc., Chicago, IL) was used for data analysis. Univariate analysis was performed by the Student t test or the Mann-Whitney test for continuous variables and by chi-square or Fisher exact tests for categorical variables. P < .05 was considered statistically significant.
A sample size of 154 obstructive episodes was originally planned to give a power of 80%, assuming that the failure rate of conservative treatment in adhesive small bowel obstruction was 30% and the operative rate could be reduced by 26% with the use of Gastrografin for patients with failed conservative treatment. The failure rate of conservative treatment was derived from articles on adhesive obstruction. 2,12,13 The reduction in operative rate was estimated from randomized controlled trials on the therapeutic effect of water-soluble contrast. 8–11 Our results revealed that the use of Gastrografin significantly reduced the operative rate by 74% after 139 obstructive episodes were recruited, giving a power of more than 95%; therefore, the study was stopped.
RESULTS
From July 1999 to December 2000, 124 patients with 139 episodes of adhesive small bowel obstruction were included. Eighty-one patients were male and 43 female. The mean age was 66 years (range 17–95). Ninety patients had undergone a single previous abdominal operation. Colorectal surgery, appendicectomy, cholecystectomy, and gastroduodenal surgery were the most common single antecedent operations. Thirty-four patients had more than one previous abdominal operation (Fig. 2). Thirty-eight patients had a history of adhesive obstruction before the study period. Fifteen patients developed two episodes of obstruction during the study. The time interval between the two episodes ranged from 2 to 17 months, with a median of 5 months. They were all treated conservatively for the first episode without Gastrografin or surgery.
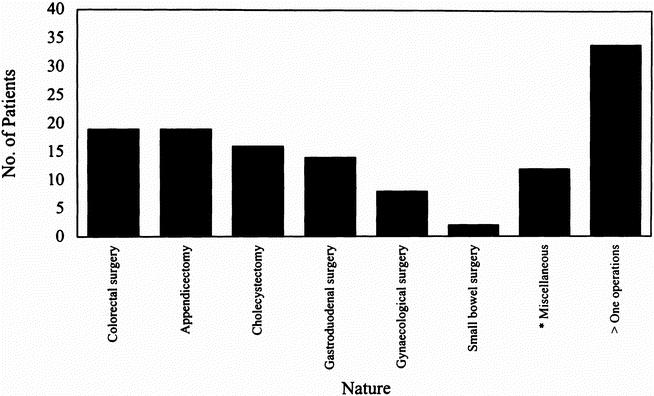
Figure 2. Antecedent operations that cause adhesive small bowel obstruction.
The mean duration of symptoms before admission was 1.84 days (range 1–7). The maximal diameter of the small bowel on admission was a mean of 42 mm (range 20–72). Because the duration of nasogastric tube decompression varied with different patients, the average nasogastric tube output of each patient (total amount of drainage/duration) was used for evaluation. For patients who underwent Gastrografin study or surgery, only the output before the procedure was considered. The mean output was 24 mL/h (range 0–124).
Three patients had emergency surgery performed within 24 hours after admission because of suspected bowel strangulation. Laparotomy confirmed strangulation in two of them, and the diseased bowel segments were resected. One hundred one cases showed improvement or resolution of obstruction during the initial 48 hours, and conservative treatment was continued. Only one of these patients required laparotomy and enterolysis on day 6 after admission. The remaining 100 cases had bowel obstruction resolved with conservative treatment; the mean time of complete resolution was 60 hours (range 7–150) after admission.
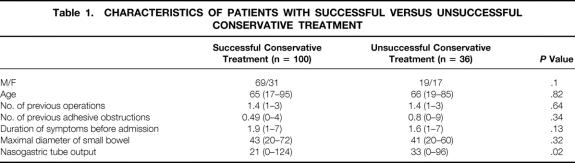
Thirty-five patients showed no improvement within 48 hours. Statistical analysis showed that nasogastric tube output was significantly higher in patients who failed to respond to conservative treatment versus those successfully treated by conventional methods (33 vs. 21 mL/h, P = .02). Other variables including sex, age, duration of symptoms before admission, number of previous abdominal operations and adhesive small bowel obstruction, and maximal diameter of small bowel on admission were not significantly different between the two groups (Table 1).
Table 1. CHARACTERISTICS OF PATIENTS WITH SUCCESSFUL VERSUS UNSUCCESSFUL CONSERVATIVE TREATMENT
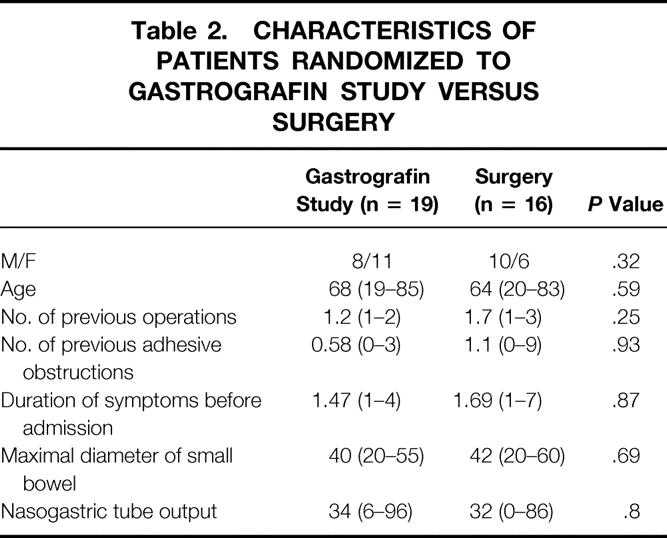
Nineteen patients were randomized to have Gastrografin study and 16 patients surgery. The groups were well matched in terms of age, sex, duration of symptoms before admission, number of previous abdominal operations and adhesive obstruction, maximal diameter of small bowel, and output of nasogastric tube (Table 2). In the Gastrografin group, the mean time that the study started was 60 hours (range 48–68) after admission. Partial obstruction was demonstrated in 14 patients. Obstruction resolved subsequently in all of them at a mean time of 41 hours (range 6–80) after administration of Gastrografin. The remaining five patients had complete obstruction shown by the contrast study and underwent laparotomy. Gastrografin significantly reduced the need for surgery by 74% (14/19, P < .001).
Table 2. CHARACTERISTICS OF PATIENTS RANDOMIZED TO GASTROGRAFIN STUDY VERSUS SURGERY
The administration of Gastrografin was not associated with any complications. There was one postoperative complication in the Gastrografin group as a result of unsuccessful enterolysis and two complications in the group randomized to undergo surgery. One patient in the latter group died of peritonitis after enterolysis (Table 3). No bowel strangulation was noted in either group. The median hospital stay of patients who had received Gastrografin was 10 days (range 5–65); that of the other group was 10 days (range 5–34).
Table 3. COMPLICATIONS AND DEATHS OF PATIENTS UNDERGOING GASTROGRAFIN STUDY VERSUS SURGERY
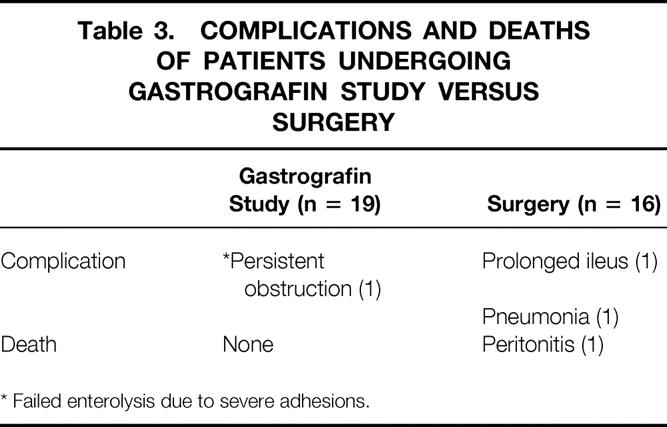
* Failed enterolysis due to severe adhesions.
DISCUSSION
Adhesive small bowel obstruction can be a complication of any abdominal operation. Studies have reported that appendicectomy and colorectal surgery are the procedures that most commonly caused adhesive obstruction. 2,12–15 Our results showed that cholecystectomy and gastroduodenal surgery also commonly caused adhesive bowel obstruction.
The management of adhesive obstruction has remained controversial. Most patients received trial conservative treatment in the initial period unless there was suspicion of bowel strangulation. However, the optimal duration of this trial conservative treatment is not clear. There has been no definite answer as to when conservative treatment should be considered unsuccessful and the patient should undergo surgery. Cox et al reported that of patients who were cured by conservative treatment, 88% had obstruction resolved within 48 hours. 16 Assalia et al recommended that surgery should be considered if the obstruction failed to improve after 48 hours of conservative treatment. 8 Sosa and Gardner found that patients without signs of strangulation could be treated nonoperatively for 24 to 48 hours. 17 The reported operative rate for adhesive small bowel obstruction ranged from 27% to 42%. 2,12,13
This study aimed to evaluate the therapeutic value of Gastrografin for selected patients who had unsuccessful conservative treatment. The ideal design for such a study would require a control arm to continue conservative treatment instead of proceeding to surgery directly. However, to continue conservative treatment for patients who showed no improvement for 48 hours may increase the risk of bowel strangulation. Before we carried out the present study, it was our practice to proceed to surgery if patients showed no clinical and radiologic improvement after receiving conservative treatment for 48 hours. This criterion for proceeding to surgery is generally acceptable according to the literature. 8,16,17 In this study, we randomized these patients to undergo either Gastrografin study or surgical treatment. There was no bowel strangulation in this group of patients with delayed intervention.
The risk factors associated with failure of conservative treatment remain poorly understood. The importance of nasogastric tube output and size of dilated small bowel have seldom been evaluated in the literature. We found that nasogastric tube output was significantly greater in patients who failed to respond to conservative treatment versus those successfully treated with conservative treatment. This could be explained by the difference in the severity of obstruction. An alternative explanation is that the nasogastric tube drainage of patients who responded to conservative treatment decreased with time; therefore, the lower average output. The degree of bowel distention was similar between the two groups, although one might think that patients with grossly distended bowel would be more likely to need surgical treatment. Among the 101 cases treated conservatively for more than 48 hours, only one patient with prolonged obstruction eventually required surgical intervention. Patients who responded to conservative treatment in the first 48 hours had a 99% (100/101) chance of successful nonoperative treatment. Seror et al stated that patients with persistent obstruction for more than 5 days always required surgical intervention. 2 Four patients in our series, however, had bowel obstruction ultimately resolved after conservative treatment for more than 5 days.
Water-soluble contrast medium has been evaluated recently in an attempt to predict the need for surgery in adhesive small bowel obstruction. Studies have also been performed to evaluate its possible therapeutic effect. Gastrografin is the contrast medium most commonly mentioned. It is an ionic, bitter-flavored mixture of sodium diatrizoate, meglumine diatrizoate, and a wetting agent (polysorbate 80). The osmolarity is 1900 mOsm/L, approximately six times that of extracellular fluid. It promotes shifting of fluid into the bowel lumen and increases the pressure gradient across an obstructive site. The bowel content is diluted, and in the presence of the wetting agent, passage of bowel contents through a narrowed lumen is facilitated. Gastrografin also decreases edema of the bowel wall and enhances bowel motility. 6,8,18 Barium has also been used to evaluate adhesive small bowel obstruction; it is not as easily diluted by enteric fluid as Gastrografin and provides a better mucosal image on radiography. However, a barium study can be risky because it may become inspissated and completely obstruct the bowel. Barium may spread into the peritoneal cavity if perforation occurs, a condition that is potentially lethal. Gastrografin is water-soluble and relatively safe even if the obstruction is complicated by perforation. Complications from the use of Gastrografin in small bowel obstruction are rare, although anaphylactoid reactions and lethal aspiration have been described. 19–21 Gastrografin may also shorten postoperative ileus and relieve intestinal obstruction caused by impacted Ascaris lumbricoides and bezoar. 8,22,23
Chen et al studied the predictive role of water-soluble contrast medium in the management of adhesive obstruction. 6 The results of their study showed that patients with contrast observed in the colon within 24 hours were all treated successfully without surgery. Surgery was required in 96% of patients in whom contrast failed to reach the colon within 24 hours. The therapeutic effect of water-soluble contrast in adhesive obstruction is controversial. In a randomized controlled study performed by Assalia et al, Gastrografin significantly prompted the resolution of obstruction, shortened the hospital stay, and reduced the need for surgery to 10% in the treatment group. 9 However, Feigin et al reported no advantage of water-soluble contrast in adhesive small bowel obstruction. 10 The operative rate, time of resolution of obstruction, and hospital stay were similar in the treatment and control groups. Similar results were obtained in Fevang et al’s study. 11 The operative rate in the treatment groups was 12% in Feigin et al’s study and 35% in Fevang et al’s study. There was no complication that could be attributed to the use of the contrast in these studies. Water-soluble contrast medium was given soon after admission in these trials. The method in our study was different: Gastrografin was administered only to patients who failed to respond to conservative treatment. To our knowledge, there has been no similar methodology in other studies. Fourteen of the 19 patients who received Gastrografin had obstruction resolved without surgical intervention. Gastrografin significantly reduced the need of surgery by 74% (14/19). If it was assumed that all 35 patients who showed no response to conservative treatment within 48 hours were given Gastrografin in our series, 9 of them would undergo surgery, and the estimated overall operative rate would be about 9% (13/139). On the other hand, if Gastrografin had not been used, all 35 patients would have undergone surgery, and the overall operative rate would be about 28% (39/139). Concerning the five patients with complete obstruction demonstrated by Gastrografin study, none of these patients had evidence of bowel strangulation at the time of surgery. It was safe to give Gastrografin even after the failure of conservative treatment. Complete resolution of bowel obstruction occurred a mean of 41 hours after administration of Gastrografin. It was usually at least 2 days later that solid food was allowed in our practice. Patients were discharged only when solid food was well tolerated. This could explain why the hospital stay of patients who had received Gastrografin was similar to that of patients who underwent surgery.
We conclude that Gastrografin is safe and reduces the need for surgery when conservative treatment fails.
Footnotes
Correspondence: Dr. Kin-Wah Chu, Department of Surgery, University of Hong Kong Medical Centre, Queen Mary Hospital, Hong Kong, China.
Accepted for publication November 29, 2001.
References
- 1.Playforth RH, Holloway JB, Griffin WO. Mechanical small bowel obstruction: a plea for early surgical intervention. Ann Surg 1970; 171: 783–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seror D, Feigin E, Szold A, et al. How conservative can postoperative small bowel obstruction be treated? Am J Surg 1993; 165: 121–126. [DOI] [PubMed] [Google Scholar]
- 3.Tanphiphat C, Chittmittrapap S, Prasopsunti K. Adhesive small bowel obstruction. A review of 321 cases in a Thai hospital. Am J Surg 1987; 154: 283–287. [DOI] [PubMed] [Google Scholar]
- 4.Blackmon S, Lucius C, Wilson JP, et al. The use of water-soluble contrast in evaluating clinically equivocal small bowel obstruction. Am Surg 2000; 66: 238–244. [PubMed] [Google Scholar]
- 5.Chen SC, Chang KJ, Lee PH, et al. Oral Urografin in postoperative small bowel obstruction. World J Surg 1999; 23: 1051–1054. [DOI] [PubMed] [Google Scholar]
- 6.Chen SC, Lin FY, Lee PH, et al. Water-soluble contrast study predicts the need for early surgery in adhesive small bowel obstruction. Br J Surg 1998; 85: 1692–1694. [DOI] [PubMed] [Google Scholar]
- 7.Wilson MS, Ellis H, Menzies D, et al. A review of the management of small bowel obstruction. Ann R Coll Surg Engl 1999; 81: 320–328. [PMC free article] [PubMed] [Google Scholar]
- 8.Assalia A, Schein M, Kopelman D, et al. Therapeutic effect of oral Gastrografin in adhesive, partial small-bowel obstruction: A prospective randomized trial. Surgery 1994; 115: 433–437. [PubMed] [Google Scholar]
- 9.Assalia A, Kopelman D, Bahous H, et al. Gastrografin for mechanical partial, small bowel obstruction due to adhesions. Harefuah 1997; 132: 629–633. [PubMed] [Google Scholar]
- 10.Feigin E, Seror D, Szold A, et al. Water-soluble contrast material has no therapeutic effect on postoperative small-bowel obstruction: Results of a prospective randomized clinical trail. Am J Surg 1996; 171: 227–229. [DOI] [PubMed] [Google Scholar]
- 11.Fevang BT, Jensen D, Fevang J, et al. Upper gastrointestinal contrast study in the management of small bowel obstruction—a prospective randomized study. Eur J Surg 2000; 166: 39–43. [DOI] [PubMed] [Google Scholar]
- 12.Cox MR, Gunn IF, Eastman MC, et al. The operative aetiology and types of adhesions causing small bowel obstruction. Aust NZ J Surg 1993; 63: 848–852. [DOI] [PubMed] [Google Scholar]
- 13.Matter I, Khalemsky L, Abrahamson J, et al. Does the index operation influence the course and outcome of adhesive intestinal obstruction? Eur J Surg 1997; 163: 767–772. [PubMed] [Google Scholar]
- 14.Füzün M, Kaymak E, Harmancioğlu Ö, et al. Principal causes of mechanical bowel obstruction in surgically treated adults in Western Turkey. Br J Surg 1991; 78: 202–203. [DOI] [PubMed] [Google Scholar]
- 15.Ellis H. The clinical significance of adhesions: Focus on intestinal obstruction. Eur J Surg 1997; 577 Suppl: 5–9. [PubMed] [Google Scholar]
- 16.Cox MR, Gunn IF, Eastman MC, et al. The safety and duration of non-operative treatment for adhesive small bowel obstruction. Aust NZ J Surg 1993; 63: 367–371. [DOI] [PubMed] [Google Scholar]
- 17.Sosa J, Gardner B. Management of patients diagnosed as acute intestinal obstruction secondary to adhesions. Am Surg 1993; 59: 125–128. [PubMed] [Google Scholar]
- 18.Strodahl A, Laerum F, Gjolberg T, et al. Water-soluble contrast media in radiography of small bowel obstruction. Acta Radiol 1988; 29: 53–56. [PubMed] [Google Scholar]
- 19.Skucas J. Anaphylactoid reactions with gastrointestinal contrast media. AJR Am J Roentgenol 1997; 168: 962–964. [DOI] [PubMed] [Google Scholar]
- 20.Ridley LJ. Allergic reactions to oral iodinated contrast agents: reactions to oral contrast. Australas Radiol 1998; 42: 114–117. [DOI] [PubMed] [Google Scholar]
- 21.Trulzsch DV, Penmetsa A, Karim A, et al. Gastrografin-induced aspiration pneumonia: a lethal complication of computed tomography. South Med J 1992; 85: 1255–1256. [DOI] [PubMed] [Google Scholar]
- 22.Watkins DT, Robertson CL. Water-soluble radiocontrast material in the treatment of postoperative ileus. Am J Obstet Gynecol 1985; 152: 450–455. [DOI] [PubMed] [Google Scholar]
- 23.Bar-Maor JA, de Carvalho JLAF, Chappell J. Gastrografin treatment of intestinal obstruction due to Ascaris lumbricoides. J Pediatr Surg 1984; 19: 174–176. [DOI] [PubMed] [Google Scholar]