Abstract
The in vitro susceptibilities of 478 Campylobacter jejuni and Campylobacter coli strains isolated from Finnish subjects during 2002 to 2004 were determined. Susceptibility to erythromycin remained high, and telithromycin did not offer any advantage over erythromycin. Reduced susceptibilities to fluoroquinolones and doxycycline were detected almost exclusively among isolates of foreign origin.
Campylobacter jejuni and C. coli are the most frequent bacterial enteropathogens in many countries, such as Finland (14). Few data on the in vitro activity of telithromycin against campylobacters are available (6, 7). We wanted to compare the activity of telithromycin to that of erythromycin against a substantial number of domestically acquired C. jejuni and C. coli isolates. In addition, susceptibilities to doxycycline, ciprofloxacin, and moxifloxacin were tested. Isolates of foreign origin selected on the basis of presumed resistance to erythromycin and/or ciprofloxacin were also included.
A total of 393 human stool culture isolates (379 C. jejuni and 14 C. coli isolates) of domestic origin (patients had not been abroad within 2 weeks prior to becoming ill) were collected in 2002. Furthermore, 85 human Campylobacter isolates (62 C. jejuni and 23 C. coli isolates) collected from 2002 to 2004 were included because of presumed reduced susceptibility, based on disk diffusion, against erythromycin and/or ciprofloxacin. Eighty-one of these 85 patients had been abroad; travel history was not known for 3 patients, and 1 patient had not been abroad.
The antimicrobial agents evaluated were telithromycin (Aventis Pharma S.A., Antony, France), erythromycin (Sigma, St. Louis, Mo.), doxycycline (Orion, Espoo, Finland), ciprofloxacin (Bayer, Leverkusen, Germany), and moxifloxacin (Bayer). The MICs for the isolates were determined by an agar dilution method according to the recent tentative CLSI (formerly NCCLS) guidelines (10, 12). Mueller-Hinton agar (Oxoid, Basingstoke, United Kingdom) supplemented with 5% defibrinated sheep blood was used. C. jejuni strain ATCC 33560 (12) was included as a control organism. For the quality control of moxifloxacin and telithromycin, Staphylococcus aureus strain ATCC 29213 and Escherichia coli strain ATCC 25922 were included. The plates were incubated in a microaerobic atmosphere at 36°C for 48 h.
Susceptibilities to erythromycin and ciprofloxacin were also determined by disk diffusion. Inocula from overnight growth were suspended in sterile saline to match a MacFarland standard of 0.5. Horse blood agar plates were inoculated, and disks (Oxoid) including erythromycin (15 μg) and ciprofloxacin (5 μg) were added. Plates were incubated as described above.
MICs of the tested antimicrobial agents for the domestic strains are shown in Table 1. The majority (70%) of the strains inhibited by erythromycin at 0.5 to 4 μg/ml showed MICs of 2 μg/ml or less of telithromycin. The growth of one domestic isolate was inhibited by erythromycin at a concentration of 8 μg/ml, while 118 isolates (30.0%) had telithromycin MICs of >2 μg/ml. Three (0.8%) domestic isolates had doxycycline MICs of ≥16 μg/ml.
TABLE 1.
MICs of five antimicrobial agents for C. jejuni and C. coli strains of domestic origin isolated during a seasonal peak from 1 July to 30 September 2002 from Finnish subjects (n = 393)
| Antimicrobial agent | MIC (μg/ml)
|
||
|---|---|---|---|
| Range | MIC50 | MIC90 | |
| Erythromycin | 0.5-8 | 2 | 4 |
| Telithromycin | 0.5-32 | 2 | 4 |
| Ciprofloxacin | 0.06-64 | 0.125 | 0.5 |
| Moxifloxacin | 0.0125-16 | 0.06 | 0.125 |
| Doxycycline | 0.06-64 | 0.125 | 0.25 |
Of the 85 Campylobacter isolates selected on the basis of presumed reduced susceptibility to ciprofloxacin and/or erythromycin, 82 isolates had MICs of ≥4 μg/ml for ciprofloxacin. In addition, 17 isolates of domestic origin showed ciprofloxacin MICs of ≥4 μg/ml. Of these 99 isolates, 91 (92%) had moxifloxacin MICs of ≥2 μg/ml. Furthermore, 53 of these 99 isolates had doxycyline MICs of ≥16 μg/ml (Table 2).
TABLE 2.
Distribution of doxycycline and erythromycin MICs for domestic and foreign Campylobacter strains (n = 99) with ciprofloxacin MICs of ≥4 μg/ml
| MIC (μg/ml) | No. of isolatesa:
|
|||
|---|---|---|---|---|
| Doxycycline
|
Erythromycin
|
|||
| Domestic | Foreign | Domestic | Foreign | |
| 0.06 | 0 | 1 | NTb | NT |
| 0.125 | 9 | 19c | 0 | 0 |
| 0.25 | 2 | 7 | 0 | 0 |
| 0.5 | 0 | 1 | 0 | 2 |
| 1 | 0 | 2c | 6 | 13c |
| 2 | 1 | 0 | 6 | 25 |
| 4 | 1 | 1 | 5 | 18c |
| 8 | 1 | 1 | 0 | 7 |
| 16 | 2 | 18c | 0 | 0 |
| 32 | 0 | 12 | 0 | 0 |
| 64 | 1 | 17c | 0 | 0 |
| 128 | 0 | 3 | 0 | 0 |
| 256 | NT | NT | 0 | 1 |
| 512 | NT | NT | 0 | 1 |
| 1,024 | NT | NT | 0 | 7 |
| >1,024 | NT | NT | 0 | 8d |
There were 17 strains of domestic origin and 78 of foreign origin. Four strains were from patients with unknown traveling histories.
NT, not tested.
One strain with unknown traveling history.
Two strains with unknown traveling history.
Of the 25 isolates with erythromycin MICs of ≥8 μg/ml, 9 were C. jejuni and 16 were C. coli, and telithromycin MICs for these are shown in Table 3. In addition, 23 of these 25 isolates showed doxycycline MICs of ≥16 μg/ml. Very high erythromycin MICs (≥1,024 μg/ml) were shown for 15 isolates (11 C. coli and 4 C. jejuni) (Table 3), 13 (87%) being of foreign origin. In total, 23 isolates, 21 of foreign origin and 2 from patients with an unknown travel history, showed simultaneously reduced susceptibilities to ciprofloxacin (MICs, ≥4 μg/ml), erythromycin (MICs, ≥8 μg/ml), and doxycycline (MICs, ≥16 μg/ml) (Table 2), and the MIC range of telithromycin was 4 to >64 μg/ml.
TABLE 3.
Distribution of telithromycin MICs for the 25 isolates with erythromycin MICs of ≥8 μg/ml
| Erythromycin MIC (μg/ml) | No. of isolates with a telithromycin MIC (μg/ml) of:
|
|||||
|---|---|---|---|---|---|---|
| 4 | 8 | 16 | 32 | 64 | >64 | |
| 8 | 2 | 2 | 1 | 2 | 1 | 0 |
| 256 | 1 | 0 | 0 | 0 | 0 | 0 |
| 512 | 1 | 0 | 0 | 0 | 0 | 0 |
| 1,024 | 0 | 0 | 1 | 0 | 5 | 1 |
| >1,024 | 0 | 0 | 0 | 1 | 7 | 0 |
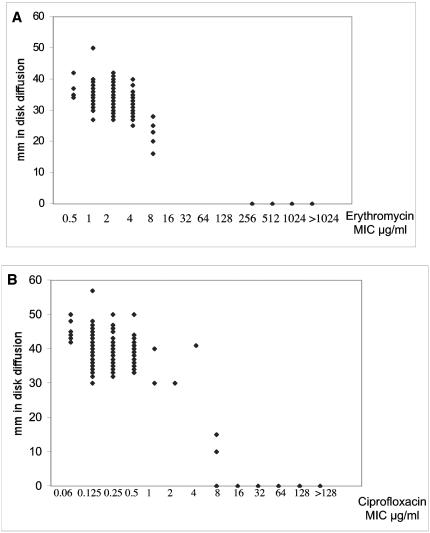
The correlation between the MICs of erythromycin and ciprofloxacin in the agar dilution method compared to the zone diameters in the disk diffusion tests is shown in Fig. 1. In clinical laboratories, the disk diffusion method could be used to detect C. jejuni and C. coli isolates with reduced susceptibilities to ciprofloxacin and erythromycin.
FIG. 1.
(A) Relation between the MICs of ciprofloxacin in the agar dilution method and the zone diameters in the disk diffusion test. (B) Relation between the MICs of erythromycin in the agar dilution method and the zone diameters in the disk diffusion test.
This study shows that among Campylobacter isolates of domestic origin in Finland, reduced susceptibility to antimicrobial agents was rare. Furthermore, the activity of erythromycin against strains of both domestic and foreign origin is still good. Earlier studies have also shown stable macrolide activity against campylobacters (4, 5, 13, 15, 17, 19). As also shown in the present study, reduced susceptibility to erythromycin is more prevalent among C. coli than C. jejuni isolates (1, 4, 5, 17, 21) and most isolates with very high erythromycin MICs are C. coli (9). Our finding that telithromycin did not have any advantage over erythromycin is in line with some previous observations (7).
Reduced susceptibility to fluoroquinolones was almost exclusively detected among isolates of foreign origin, and in half of these isolates, high doxycycline MICs were also demonstrated. Among campylobacters, resistance to fluoroquinolones has increased over the past 15 years in many parts of the world, including Finland (3, 4, 8, 15, 16, 19). In Finland, susceptibility to fluoroquinolones among domestic Campylobacter isolates has remained consistently good (13), as confirmed in the present study. Similarly, in some other countries (Australia and Sweden), fluoroquinolone resistance among domestically acquired campylobacter infections is rare (18, 20). This may be explained in some cases by the lack of fluoroquinolone use in food production animals (2, 11, 20).
Compared to several other studies (16, 18, 19), our study showed a tetracycline agent to have a high activity against Campylobacter isolates of domestic origin. However, of the isolates with reduced susceptibility to ciprofloxacin, 54% were inhibited only by high concentrations of doxycycline. Simultaneously reduced susceptibility to other antimicrobial agents is also possible. In a recent Finnish study, 22% of Campylobacter strains isolated from travelers returning to Finland were multidrug resistant (7). In our study, of the 23 isolates with reduced susceptibilities to ciprofloxacin, doxycycline, and erythromycin, all showed telithromycin MICs of >2 μg/ml. Although campylobacter infection usually is a self-limiting disease and antimicrobial therapy is not needed, the scenario of treating infections caused by multidrug-resistant isolates could be challenging.
In conclusion, erythromycin shows good activity against campylobacters in Finland; isolates with elevated MICs also have a reduced susceptibility to telithromycin. Foreign isolates, frequently with a reduced susceptibility to fluoroquinolones, often show high MICs to other antimicrobial agents as well.
Acknowledgments
This study was partially supported by a Helsinki University Central Hospital Research Fund (grant number TYH 3257) and grants to Daniela Schönberg-Norio from Finska Läkaresällskapet (Finnish Medical Association), Finsk-Norska Medicinska Stiftelsen (Finnish-Norwegian Medical Foundation), and Medicinska Understödsföreningen Liv och Hälsa (Medical Society for Life and Health).
We do not have a commercial or other association that might pose a conflict of interest.
Seppo Sarna is gratefully acknowledged for his comments. The technical assistance of Pirjo Kosonen is gratefully acknowledged.
REFERENCES
- 1.Aarestrup, F., E. Nielsen, M. Madsen, and J. Engberg. 1997. Antimicrobial susceptibility patterns of thermophilic Campylobacter spp. from humans, pigs, cattle, and broilers in Denmark. Antimicrob. Agents Chemother. 41:2244-2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Commonwealth of Australia. 1999. The use of antibiotics in food-producing animals: antibiotic-resistant bacteria in animals and humans. Report of the Joint Expert Technical Advisory Committee on Antibiotic Resistance (JETACAR). [Online.] http://www.health.gov.au/pubs/jetacar.htm.
- 3.Endtz, H., G. Ruijs, B. van Klingeren, W. Jansen, T. van der Reyden, and P. Mouton. 1991. Quinolone resistance in campylobacter isolated from man and poultry following the introduction of fluoroquinolones in veterinary medicine. J. Antimicrob. Chemother. 27:199-208. [DOI] [PubMed] [Google Scholar]
- 4.Engberg, J., F. Aarestrup, D. Taylor, P. Gerner-Smidt, and I. Nachamkin. 2001. Quinolone and macrolide resistance in Campylobacter jejuni and C. coli: resistance mechanisms and trends in human isolates. Emerg. Infect. Dis. 7:24-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Engberg, J., J. Neimann, E. Nielsen, F. Aarestrup, and V. Fussing. 2004. Quinolone-resistant Campylobacter infections: risk factors and clinical consequences. Emerg. Infect. Dis. 10:1056-1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Felmingham, D., and D. Farrell. 2005. In vitro activity of telithromycin against Gram-negative bacterial pathogens. J. Infect. [Online.] doi: 10.1016/j.jinf.2005.05.014. [DOI] [PubMed]
- 7.Hakanen, A., M. Lehtopolku, A. Siitonen, P. Huovinen, and P. Kotilainen. 2003. Multidrug resistance in Campylobacter jejuni strains collected from Finnish patients during 1995-2000. J. Antimicrob. Chemother. 52:1035-1039. [DOI] [PubMed] [Google Scholar]
- 8.Hoge, C., J. Gambel, A. Srijan, C. Pitarangsi, and P. Echeverria. 1998. Trends in antibiotic resistance among diarrheal pathogens isolated in Thailand over 15 years. Clin. Infect. Dis. 26:341-345. [DOI] [PubMed] [Google Scholar]
- 9.Li, C.-C., C.-H. Chiu, J.-L. Wu, Y.-C. Huang, and T.-Y. Lin. 1998. Antimicrobial susceptibilities of Campylobacter jejuni and coli by using E-test in Taiwan. Scand. J. Infect. Dis. 30:39-42. [DOI] [PubMed] [Google Scholar]
- 10.McDermott, P., S. Bodeis, F. Aarestrup, S. Brown, M. Traczewski, P. Fedorka-Cray, M. Wallace, I. Critchley, C. Thornsberry, S. Graff, R. Flamm, J. Beyer, D. Shortridge, L. Piddock, V. Ricci, M. Johnson, R. Jones, B. Reller, S. Mirrett, J. Aldrobi, R. Rennie, C. Brosnikoff, L. Turnbull, G. Stein, S. Schooley, R. Hanson, and R. Walker. 2004. Development of a standardized susceptibility test for Campylobacter with quality-control ranges for ciprofloxacin, doxycycline, erythromycin, gentamicin, and meropenem. Microb. Drug Resist. 10:124-131. [DOI] [PubMed] [Google Scholar]
- 11.Myllyniemi, A.-L., J. Koppinen, V. Gindonis, and S. Nykäsenoja. 2005. FINRES-Vet 2002-2003, Finnish Veterinary Antimicrobial Resistance Monitoring and Consumption of Antimicrobial Agents. National Veterinary and Food Research Institute (EELA), Helsinki, Finland. [Online.] http://www.eela.fi/linked/fi/julkaisut/finres_vet.pdf.
- 12.National Committee for Clinical Laboratory Standards. 2003. Informational supplement M100-S13. NCCLS, Wayne, Pa.
- 13.Rautelin, H., A. Vierikko, M.-L. Hänninen, and M. Vaara. 2003. Antimicrobial susceptibilities of Campylobacter strains isolated from Finnish subjects infected domestically or from those infected abroad. Antimicrob. Agents Chemother. 47:102-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rautelin, H. and M.-L. Hänninen. 2000. Campylobacters: the most common bacterial enteropathogens in the Nordic countries. Ann. Med. 32:440-445. [DOI] [PubMed] [Google Scholar]
- 15.Rautelin, H., O.-V. Renkonen, and T. Kosunen. 1991. Emergence of fluoroquinolone resistance in Campylobacter jejuni and Campylobacter coli in subjects from Finland. Antimicrob. Agents Chemother. 35:2065-2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reina, J., M. Ros, and A. Serra. 1994. Susceptibilities to 10 antimicrobial agents of 1220 Campylobacter strains isolated from 1987 to 1993 from feces of pediatric patients. Antimicrob. Agents Chemother. 38:2917-2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sánchez, R., V. Fernández-Baca, M. Díaz, P. Munoz, M. Rodríguez-Créixems, and E. Bouza. 1994. Evolution of susceptibilities of Campylobacter spp. to quinolones and macrolides. Antimicrob. Agents Chemother. 38:1879-1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sjögren, E., G.-B. Lindblom, and B. Kaijser. 1997. Norfloxacin resistance in Campylobacter jejuni and Campylobacter coli isolates from Swedish patients. J. Antimicrob. Chemother. 40:257-261. [DOI] [PubMed] [Google Scholar]
- 19.Smith, K., J. Besser, C. Hedberg, F. Leano, J. Bender, J. Wicklund, B. Johnson, K. Moore, and M. Österholm. 1999. Quinolone-resistant Campylobacter jejuni infections in Minnesota, 1992-1999. N. Engl. J. Med. 340:1525-1532. [DOI] [PubMed] [Google Scholar]
- 20.Unicomb, L., J. Ferguson, T. Riley, and P. Collignon. 2003. Fluoroquinolone resistance in campylobacter absent from isolates, Australia. Emerg. Infect. Dis. 9:1482-1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Looveren, M., G. Daube, L. de Zutter, J.-M. Dumont, C. Lammens, M. Wijdooghe, P. Vandamme, M. Jouret, M. Cornelius, and H. Goossens. 2001. Antimicrobial susceptibilities of Campylobacter strains isolated from food animals from Belgium. J. Antimicrob. Chemother. 48:235-240. [DOI] [PubMed] [Google Scholar]