Abstract
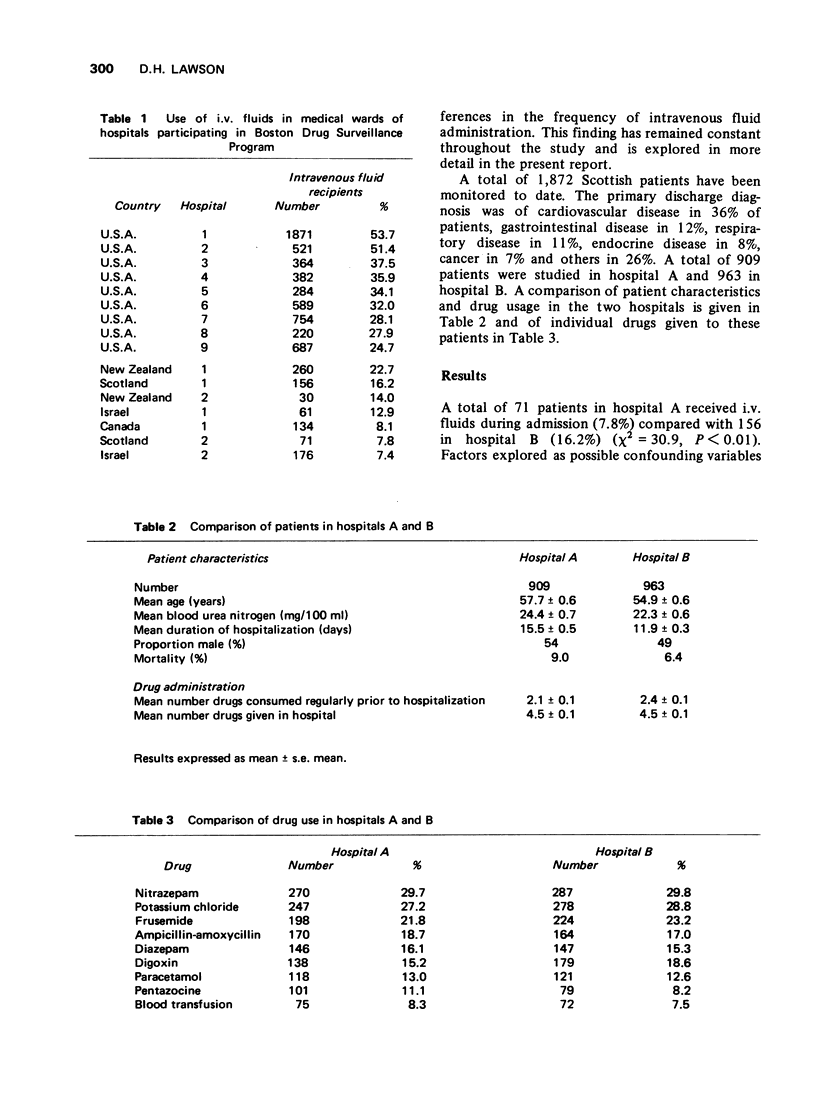
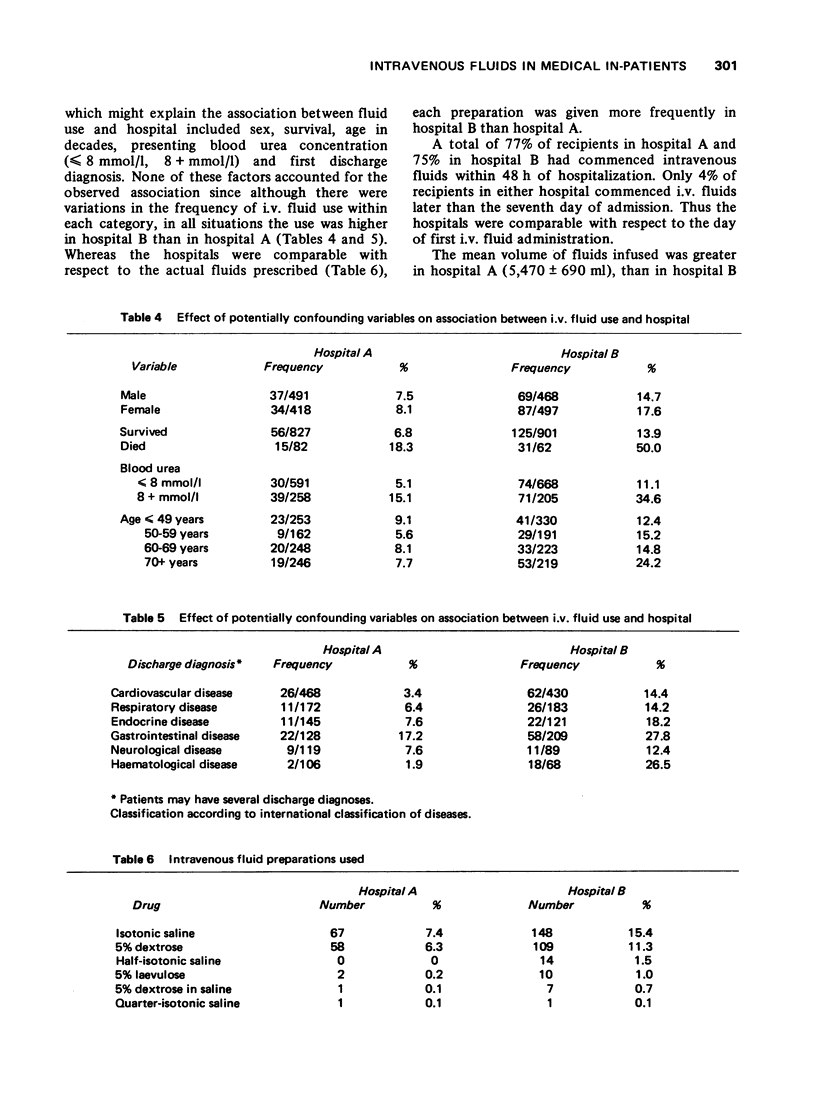
1 Data from the Boston Collaborative Drug Surveillance Program were reviewed to determine the proportion of patients receiving intravenous fluids in the participating hospitals. 2 Wide differences between hospitals in the United States and four other countries were observed: i.v. fluids being given to 54% of patients in one American hospital and only 7% of patients in an Israeli one. A two-fold difference in the frequency of i.v. fluid use in two otherwise comparable Scottish teaching hospitals was observed. This difference was not due to observed patient characteristics, did not arise from selection bias or observational differences between the two hospitals and was unlikely to have arisen by chance. 3 It is concluded that the findings were due to different policies on the part of the attending physicians. Although the study could not be used to evaluate the beneficial effects of the administered fluids, adverse effects were common (15% of recipients) and in some instances potentially serious. Adverse effects were reported more frequently after infusion of 5% dextrose (13% of recipients) than after isotonic saline (7%) perhaps because of the low pH of the former solution.
Full text
PDF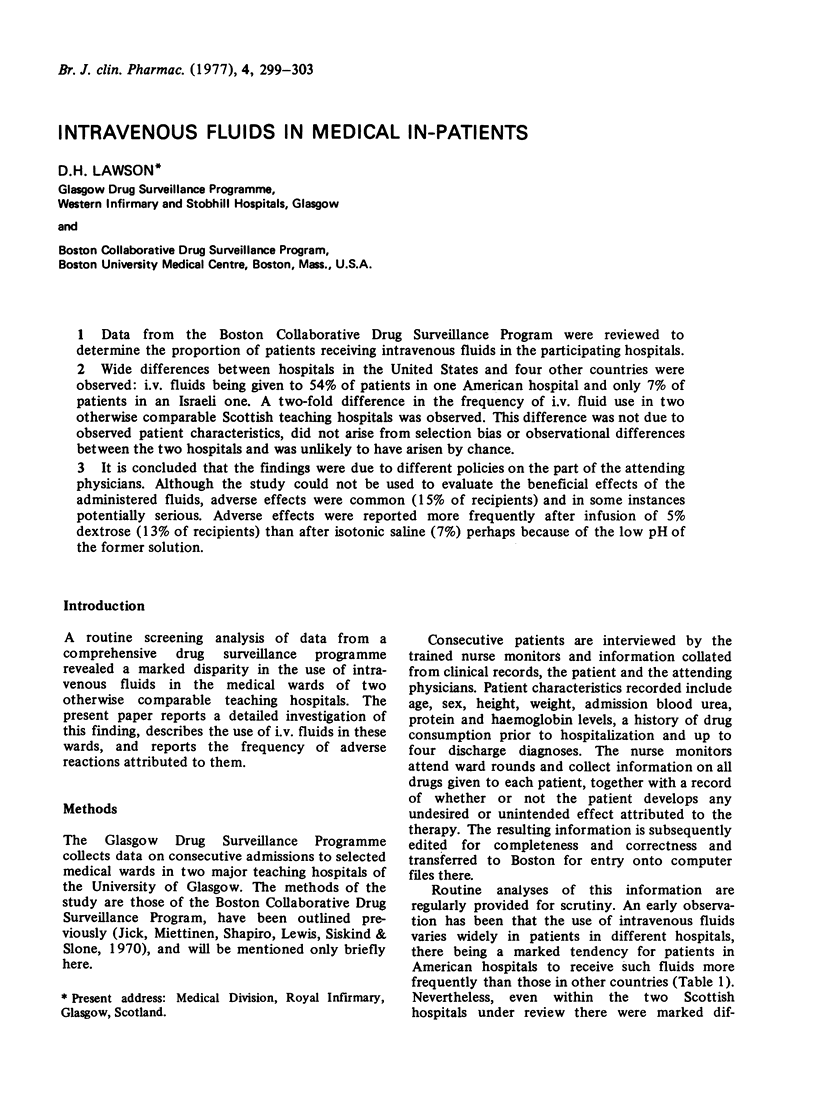
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Clemetson C. A., Moshfeghi M. M. Strange effects of "dextrose 5 percent in water". N Engl J Med. 1969 Feb 6;280(6):332–332. doi: 10.1056/NEJM196902062800618. [DOI] [PubMed] [Google Scholar]
- Collins R. N., Braun P. A., Zinner S. H., Kass E. H. Risk of local and systemic infection with polyethylene intravenous catheters. A prospective study of 213 catheterizations. N Engl J Med. 1968 Aug 15;279(7):340–343. doi: 10.1056/NEJM196808152790702. [DOI] [PubMed] [Google Scholar]
- Conferences and meetings: royal college of surgeons at bristol. Br Med J. 1967 Jan 14;1(5532):107–108. [PMC free article] [PubMed] [Google Scholar]
- Darrell J. H., Garrod L. P. Secondary septicaemia from intravenous cannulae. Br Med J. 1969 May 24;2(5655):481–482. doi: 10.1136/bmj.2.5655.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfving G., Saikku K. Effect of pH on the incidence of infusion thrombophlebitis. Lancet. 1966 Apr 30;1(7444):953–953. doi: 10.1016/s0140-6736(66)90950-0. [DOI] [PubMed] [Google Scholar]
- Jick H., Miettinen O. S., Shapiro S., Lewis G. P., Siskind V., Slone D. Comprehensive drug surveillance. JAMA. 1970 Aug 31;213(9):1455–1460. [PubMed] [Google Scholar]
- Lawson D. H., Jick H. Drug prescribing in hospitals: an international comparison. Am J Public Health. 1976 Jul;66(7):644–648. doi: 10.2105/ajph.66.7.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller R. R. Drug surveillance utilizing epidemiologic methods. A report from the Boston Collaborative Drug Surveillance Program. Am J Hosp Pharm. 1973 Jul;30(7):584–592. [PubMed] [Google Scholar]
- Riyami A. Complications of intravenous infusions. J Ir Med Assoc. 1968 Jan;61(367):23–25. [PubMed] [Google Scholar]
- Turco S. J., Davis N. M. Detrimental effects of particulate matter on the pulmonary circulation. JAMA. 1971 Jul 5;217(1):81–82. doi: 10.1001/jama.1971.03190010063029. [DOI] [PubMed] [Google Scholar]


