Abstract
Objectives. This study assessed the tobacco cessation knowledge, attitudes, and behaviors of dentists participating in a large managed care dental plan.
Methods. Participating dentists in 4 states were surveyed via mail.
Results. Dentists' perceived success in helping patients quit using tobacco was highly correlated with discussion of specific strategies for quitting, advice about the use of nicotine gum, and time spent counseling patients. Dentists who were confident about their smoking cessation knowledge frequently advised patients to quit and spent more time counseling patients about tobacco cessation.
Conclusions. Tobacco cessation is not a routine part of dental practice. Knowledge, time spent counseling patients, and specific strategies for quitting were associated with dentists' perceptions of success. (Am J Public Health. 2002;92:997–1001)
The use of tobacco products, especially cigarettes, represents the leading cause of preventable illness and death in the developed world. In addition to being associated with a number of cancers and coronary conditions, tobacco plays a role in the etiology of a number of oral conditions; it is a primary risk factor for oral cancer,1,2 as well as leukoplakia,3 periodontitis,4 and delayed wound healing.5
Health care providers can play a vital role in helping their patients attempt and realize tobacco cessation. The 2000 Public Health Service clinical practice guideline6 indicates that “brief physician advice significantly increases long-term smoking abstinence rates.” However, according to the guideline, intensive interventions are more effective than less intensive interventions and should be used whenever possible.
Office-based interventions involve the use of some or all of a combination of cessation advice by a clinician, setting of a quit date, use of nicotine replacement therapy, and one or more recall visits for reinforcement and support. Currently, most tobacco cessation interventions are provided by physicians, although it has been demonstrated that all health care providers can be effective.7 In addition, pilot studies have indicated that the most effective interventions may be office based1,8; in this instance, key office staff are trained in cessation techniques, and an effort to provide tobacco cessation services is made by all trained members.9
The American Dental Association (ADA) has endorsed dentists' role in tobacco cessation efforts.10 Tobacco cessation has been assigned an ADA procedure code; however, dentists use this code infrequently. Dental teams (dentists, dental hygienists, dental assistants, and support staff) have been encouraged by organizations including the ADA, the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, and the Public Health Service11 to provide tobacco cessation instruction and intervention in the dental office. The guidelines6 promulgated for health professionals are consistent with the broad preventive message already provided in dental offices.
In the mid-1990s, nearly 25% of dental schools and 36% of dental hygiene schools in Canada and the United States did not include questions about tobacco on their health history forms12; continuing education courses that specifically addressed tobacco cessation were few,13 and only 19% of dentists or hygienists had completed formal training in tobacco cessation.14 More recent assessments of dental programs indicate an upward trend in the number of schools advising their students to discuss strategies to help their patients stop using tobacco.15
National surveys suggest that between 30% and 50%14,16 of US dentists, along with 25% of hygienists, ask their patients about smoking. However, the cessation advice provided in dental offices has been described as “rather ad hoc and somewhat superficial,”17 with fewer than 20% of dentists using an office-based smoker identification system14 and fewer than 5% offering follow-up services to help patients quit.16
In a study that attempted to compare the quality and quantity of tobacco cessation services provided by different health care providers, including physicians, dentists, mental health counselors, and social workers, the authors concluded that cessation interventions by dental providers ranked lowest in terms of both quantity and quality.18 However, it is apparent that evidence of smoking cessation activities by dentists has been collected in a sporadic fashion. Results reported depend on the populations tested and the methods used to collect and analyze data.
Lack of training and lack of financial incentives are most often cited to explain the reluctance of dentists and hygienists to provide tobacco cessation interventions.14 Dentists' concern about their ability to effectively help patients quit is another of the most frequently cited reasons for not incorporating tobacco cessation activities into their practices.19,20 Additional barriers practitioners perceive to providing tobacco cessation services include amount of time required to counsel patients, patient resistance, and lack of knowledge about referrals.20 This is not restricted to dentists; integration of clinical guidelines into practice is a problem for all clinicians. For example, Cabana et al. provided a thorough assessment of physicians' difficulties in following clinical practice guidelines.21
Despite the relative absence of tobacco cessation activities in dental offices, dentists are favorably situated to provide cessation services, in that more than 50% of smokers make an annual visit to the dentist.22,23 Dental patients, especially those with insurance, receive care on a regular basis. Dental treatment often necessitates frequent contact with patients over an extended period of time, providing a mechanism for long-term contact and reinforcement. In addition, dental providers are in the unique position of being able to associate cessation advice with readily visible changes in oral status.
Physicians' offices are not the locus of regular well visits in the critical 20- to 44-year age group, in which tobacco cessation strategies may have their greatest impact in preventing morbidity and mortality. Visits to physicians are often made only if they are mandated by employers or are “problem oriented.”
Dental visits, in contrast, are usually preventive. Furthermore, patients who attend dental offices for “problem-oriented” visits are mainstreamed into prevention programs and regular examination and hygiene visits after completion of treatment. In addition, dentists have strong financial incentives from managed care organizations to maintain patients' health. Failure to maintain patients' dental health will result in more treatment visits, which are costly and often produce no additional compensation for the dentist.
An increasingly common feature of dental practice is an emphasis on cosmetic dentistry. Patients today are more acutely aware of their appearance; they request whitening agents, porcelain laminate overlays on anterior teeth, crowns, and plastic composites. All of these treatments counter the effects of staining and poor oral appearance caused by smoking. The opportunity to introduce cessation strategies is a “natural” in this context.
Assuming that dentists' knowledge and experiences may affect subsequent practices, an effective way to influence a change in dentists' tobacco cessation activities may be through office-based educational interventions targeting the dental provider. In addition, incentives and regulatory mechanisms provided through the managed care organization24 should help promote clinical tobacco cessation as a standard of dental practice.
In this study, we surveyed dentists in a large managed care dental plan in regard to their knowledge of and attitudes toward tobacco cessation practices. Also, we assessed whether they support, encourage, or promote the use of tobacco cessation measures in their patient–provider relationships and whether patient expectations create demand for these services.
METHODS
After a list of dentists participating in the Aetna managed care plan was obtained, the list was cleaned according to the following criteria: (1) 300 or more Aetna patients of record and (2) dental practice located in the New York to Philadelphia metropolitan corridor, which includes parts of Connecticut, New Jersey, New York, and Pennsylvania. This corridor, which was accessible by car for planned future visits, contains a large number of dental offices enrolled in the Aetna dental insurance plan.
Dental offices were eligible to participate only if all of the providers employed in the office were not employed in any other office. The number of offices that employed dentists who worked at more than one location or had the same owner approached 25% of the overall sample. In addition, if more than one office was owned by an individual, only one of these offices could participate.
Twenty-one percent of the 355 eligible offices agreed to participate. Seventy-five dental offices were recruited into the study during 2000–2001. Data were generated through a questionnaire (Survey of Dentists' Knowledge, Attitudes, Beliefs, and Practices) completed by the principal dentist within the office; SPSS was used in entering and analyzing data.
Dental offices were first contacted by mail. A letter that described the study, appealed for completion of the questionnaire, and alerted the dentist that a member of the research team would be calling the office in a few days was sent with a $100 check, the questionnaire, and a self-addressed stamped envelope. Dentists were fully informed of study details, via the telephone calls, and were provided an opportunity to ask questions concerning the study.
Data were collected from 75 dental offices via the mailed survey instrument, which consisted of 29 closed-ended questions. The survey included sections on (1) office-based barriers to smoking cessation counseling, (2) processes involved in the adoption of cessation counseling, (3) perceptions of staff and patient acceptance of related changes, and (4) allocation of resources (time, labor, money).
Frequencies were calculated for all variables. Proportions of dentists reporting behaviors related to advice or prescriptions of nicotine replacement therapy and discussion of setting specific quit dates were calculated, along with Pearson correlations between the following key variables: (1) percentage of patients asked about tobacco use, (2) frequency of advice to smokers to quit, (3) counseling of patients regarding tobacco cessation, (4) average time counseling patients regarding tobacco cessation, (5) decade of graduation from dental school, (6) perceived success in helping patients quit, and (7) whether more than 40% of patients were queried in regard to tobacco use.
RESULTS
Best practices for clinical interventions in primary care settings encompass 5 steps.6 These steps, referred to as the “5 A's,” are ask, advise, assess, assist, and arrange. As recommended in the 2000 Public Health Service clinical practice guideline, it is important for the clinician to ask the patient whether he or she uses tobacco, advise him or her to quit, assess willingness to make a quit attempt, assist in making a quit attempt, and arrange for follow-up contacts to prevent relapse. At the time of administration of this survey, one of the A's—assess—had not been incorporated into the clinical practice guideline. Results reported subsequently reflect an emphasis on the other “A's,” each of which is indicated in sequential fashion to mirror dentists' knowledge, attitudes, and behavior.
In terms of assessment of clinician knowledge, results of our survey indicated that 82% of the patients who participated in the tobacco cessation program were told about associations between tobacco use and general health status. Our analyses of clinicians' attitudes provided the following results: 95.2% of the providers indicated that they were willing or very willing to receive training, and 12.5% of dentists indicated that time was not a barrier to incorporating tobacco cessation activities into dental offices; twice as many reported that reimbursement was not a barrier.
Dentists' perceived success in helping patients quit using tobacco was highly correlated with the percentage of tobacco-using patients who were asked about their tobacco use, the frequency with which they were given advice (proportion of visits), assistance in terms of discussions of the association of tobacco use with general health, discussions of specific strategies for quitting, advice about the use of nicotine gum, and average time spent counseling patients regarding tobacco cessation. This last variable had the highest correlation (0.635) with dentists' perceived success in assisting patients to quit using tobacco (Table 1 ▶).
TABLE 1.
—Bivariate Relationships Between Critical Variables in This Study
| Percentage of Patients Asked About Tobacco Use | Frequency of Advice to Smokers to Quit | Average Time Counseling Patients Regarding Tobacco Cessation | Counseled Patients Regarding Tobacco Cessation | Decade of Graduation from Dental School | Perceived Success n Helping atients Quit | More Than More Than40% of Patients Asked About Tobacco Use | |||||||||||||||
| Correlation | P | No. | Correlation | P | No. | Correlation | P | No. | Correlation | P | No. | Correlation | P | No. | Correlation | P | No. | Correlation | P | No. | |
| Percentage of patients asked about tobacco use | … | 0.591 | .000 | 68 | 0.457 | .000 | 67 | … | …a | 0.395 | .003 | 54 | … | ||||||||
| Frequency of advice to smokers to quit | 0.591 | .000 | 68 | … | 0.400 | .001 | 67 | 0.412 | .001 | 67 | …a | 0.550 | .000 | 54 | 0.616 | .000 | 68 | ||||
| Average time counseling patients regarding tobacco cessation | 0.457 | .000 | 67 | 0.400 | .001 | 67 | … | … | …a | 0.635 | .000 | 54 | 0.435 | .000 | 67 | ||||||
| Decade of graduation from dental school | …a | …a | …a | …a | … | …a | …a | ||||||||||||||
| Perceived success in helping patients quit | 0.395 | .003 | 54 | 0.550 | .000 | 54 | 0.635 | .000 | 54 | 0.390 | .004 | 54 | …a | … | 0.399 | .003 | 54 | ||||
| Discussion of the association of tobacco use with general health | 0.304 | .023 | 56 | 0.503 | .000 | 56 | …a | …a | …a | 0.365 | .013 | 46 | 0.316 | .018 | 56 | ||||||
| Discussion of setting specific quit dates with patients interested in quitting | …a | …a | …a | …a | …a | …a | …a | ||||||||||||||
| Discussion of specific strategies for quitting | …a | …a | 0.508 | .000 | 56 | …a | …a | 0.413 | .004 | 47 | …a | ||||||||||
| Advice on nicotine gum | …a | 0.372 | .005 | 55 | 0.402 | .002 | 55 | …a | …a | 0.356 | .014 | 47 | …a | ||||||||
| Advice on the nicotine transdermal patch | …a | 0.318 | .018 | 55 | 0.329 | .014 | 55 | …a | …a | …a | …a | ||||||||||
| Prescription of bupropion | …a | …a | 0.316 | .019 | 55 | …a | …a | …a | …a | ||||||||||||
| Referral of patients to cessation clinics or programs | 0.329 | .014 | 55 | …a | …a | … | …a | …a | 0.313 | .020 | 55 | ||||||||||
Note. P values are 2-tailed.
aNonsignificant.
Our analyses of clinician behavior provided the following results. The dentist was responsible for tobacco cessation in 96% of offices, with few offices (3%) using a dental hygienist. Only 9.4% of the providers surveyed had received previous training in tobacco cessation. Fewer than one fifth of dentists had asked about tobacco use during the past month with more than 80% of their patients.
Of the dentists surveyed, 25.5% reported that they advised patients to quit smoking at every or almost every visit, but only half of these dentists indicated that they had a specific strategy for discussing tobacco cessation with patients who smoke. Relatively few dentists (12.3%) recorded counseling behaviors on the charts of more than 80% of their patients. In all, 9.7% of responding dentists reported assisting patients with information about the use of a transdermal patch or nicotine gum on a consistent basis.
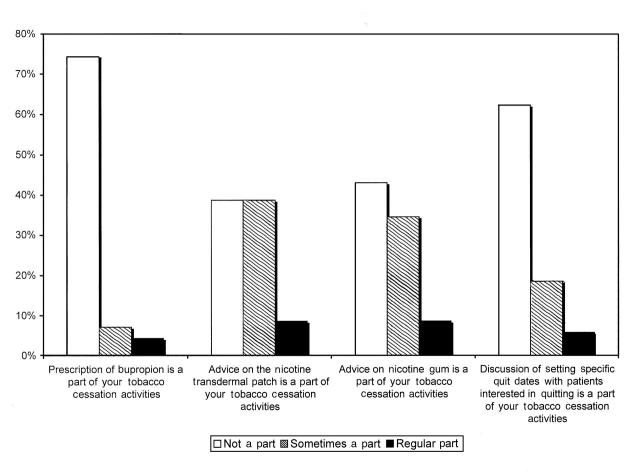
Assisting patients with tobacco cessation advice about or prescription of nicotine replacement therapy was not a part of usual and customary practice for the responding dentists, with between 40% and 50% reporting that giving advice about the nicotine transdermal patch was not a part of their tobacco cessation activities and fewer than 10% reporting that it was a regular part of their activities. Approximately 75% of dentists did not assist patients by prescribing bupropion (Zyban), with approximately 5% reporting that it was a regular part of their activities.
More than 60% of responding dentists reported that assisting tobacco-using patients in setting a specific quit date was not a part of their activities; about 5% reported that it was, in fact, a regular part of their activities (Figure 1 ▶). There were statistically significant correlations between average time spent counseling patients regarding tobacco cessation and discussing specific strategies for quitting with patients, providing advice on nicotine gum and on the nicotine transdermal patch, and prescribing bupropion.
FIGURE 1.
—Tobacco cessation activities of dentists: 4 US states, 2000–2001.
Some “negative findings” were unexpected and perhaps counterintuitive. For example, decade of graduation from dental school, a proxy for age, was not highly correlated with any of the other variables included in the correlation matrix, and referral of patients to cessation clinics or programs was moderately correlated only with percentage of patients asked about tobacco use. Also, with the exception of a statistically significant but only moderate correlation with time spent counseling patients (0.316), prescription of bupropion was not correlated with any of the variables in the correlation matrix (Table 1 ▶).
DISCUSSION
The results of this study indicate that many dental offices participating in the survey did not have prior training in tobacco control, did not ask their patients about tobacco use, and did not provide advice about nicotine replacement therapy. In addition, patient expectations do not create a demand for these services.
Moreover, pharmaceutical companies offering nicotine replacement therapy products often direct their efforts at physicians. However, as mentioned earlier, physicians' offices are not the locus of regular well visits in the 20- to 44-year age group, in which tobacco cessation strategies may have their greatest impact in preventing morbidity and mortality. In contrast, dental visits among people in this age group are usually preventive.
Also as mentioned, patients who attend dental offices for problem-oriented visits are later enlisted into prevention programs and continue with visits on a regular schedule. Moreover, managed care organizations provide dentists with a strong financial incentive to maintain their patients' health so as to avoid costly additional treatment visits.
Recruitment of dentists into this study was difficult, even though free continuing education and a $100 honorarium were provided. Barriers to acceptance of dentists' role in tobacco cessation training are substantial. Incorporating the “5 A's” into dental practices requires systematic changes in these practices. There is a substantial “disconnect” between a dentist's advice to quit and assisting and arranging for the patient to quit.
CONCLUSIONS
Findings associated with this study should be interpreted with a degree of caution. Generalization to other populations would not be appropriate. The dental health maintenance organization involved in this study is not necessarily representative of other such organizations. The relatively low response rate of dentists invited to participate is probably an indication that there is even more resistance to incorporating tobacco cessation into dental practices than these findings suggest.
This study is the first step in developing an intervention. Nevertheless, several of the present findings should help others who are considering addressing this critical public health problem. For example, average time spent counseling patients regarding tobacco cessation was shown to be associated with provision of advice on nicotine replacement therapy (nicotine gum, nicotine transdermal patch, bupropion) and discussion of specific strategies for quitting. Also, age was not associated with whether or not dentists engaged in tobacco prevention activities. Finally, dentists who were confident about their smoking cessation knowledge were shown to advise patients to quit more frequently.
Acknowledgments
This work was supported in part by grants from the Robert Wood Johnson Foundation and Aetna Inc. Informed consent procedures were approved by the institutional review board of Columbia University.
Special thanks to Ed Schooley, DDS, Marvin Zatz, DDS, MPH, and Thomas Gotowka, DDS, MS, MPA, for their support and assistance in implementing this project within the managed care organization examined. We would also like to acknowledge the assistance of Faith Miller-Sethi, a graduate student in the Mailman School of Public Health, Columbia University.
D. Albert, K. Ahluwalia, and D. Sadowsky helped to plan the study and write the article. D. Albert and D. Sadowsky worked on the analysis. A. Ward was responsible for field operations during the study.
Peer Reviewed
References
- 1.Day GI, Blot WJ, Austin DF, et al. Racial differences in risk of oral and pharyngeal cancer: alcohol, tobacco and other determinants. J Natl Cancer Inst. 1993;85:465–473. [DOI] [PubMed] [Google Scholar]
- 2.Mashburg A, Samit A. Early diagnosis of asymptomatic oral and oropharyngeal squamous cancers. CA Cancer J Clin. 1995;45:328–351. [DOI] [PubMed] [Google Scholar]
- 3.Palmer RM. Tobacco smoking and oral health. Br Dent J. 1988;164:258–260. [DOI] [PubMed] [Google Scholar]
- 4.Tomar SL, Asma S. Smoking attributable periodontitis in the United States: findings from NHANES III. J Periodontol. 2000;71:743–751. [DOI] [PubMed] [Google Scholar]
- 5.Preber H, Bergstrom J. Effect of smoking on periodontal healing following surgical therapy. J Clin Periodontol. 1990;17:324–328. [DOI] [PubMed] [Google Scholar]
- 6.Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence: Clinical Practice Guideline. Rockville, Md: Public Health Service; 2000.
- 7.Fiore MC, Bailey WC, Cohen SJ, et al. Smoking Cessation: Clinical Practice Guideline No. 18. Rockville, Md: Agency for Health Care Policy and Research; 1996. AHCPR publication 96-0692.
- 8.Solberg LI, Kottke TE, Brekke ML, Calomeni CA, Conn SA, Davidson G. Using continuous quality improvement to increase preventive services in clinical practice—going beyond guidelines. Prev Med. 1996;25:259–267. [DOI] [PubMed] [Google Scholar]
- 9.Kottke TE, Solberg LI, Conn SA, et al. A comparison of two methods to recruit physicians to deliver smoking cessation interventions. Arch Intern Med. 1990;150:1477–1481. [PubMed] [Google Scholar]
- 10.Jones R. Tobacco or oral health: past progress, impending challenge. J Am Dent Assoc. 2000;131:1130–1136. [DOI] [PubMed] [Google Scholar]
- 11.Tobacco Use and Dependence Clinical Practice Guideline Panel. A clinical practice guideline for treating tobacco use and dependence: a US Public Health Service report. JAMA. 2000;283:3244–3254. [PubMed] [Google Scholar]
- 12.Yellowitz JA, Goodman HS, Horowitz AM, Al-Tannir MA. Assessment of alcohol and tobacco use in dental school health history forms. J Dent Educ. 1995;59:1091–1096. [PubMed] [Google Scholar]
- 13.Continuing Education Course Listing: July–December 1994. Chicago, Ill: American Dental Association; 1993:30.
- 14.Dolan TA, McGorray SP, Grinstead-Skigen CL, Mecklenburg R. Tobacco control activities in U.S. dental practices. J Am Dent Assoc. 1997;128:1669–1679. [DOI] [PubMed] [Google Scholar]
- 15.Barker GJ, Williams KB. Tobacco use cessation activities in U.S. dental and dental hygiene student clinics. J Dent Educ. 1999;63:828–833. [PubMed] [Google Scholar]
- 16.Jones RB, Pomrehn PR, Mecklenburg RE, Lindsay EA, Manley M, Ockene JK. The COMMIT dental model: tobacco control practices and attitudes. J Am Dent Assoc. 1993;124:92–104. [DOI] [PubMed] [Google Scholar]
- 17.Hastreiter RJ, Bakdash B, Roesch MH, Walseth J. Use of tobacco prevention and cessation strategies and techniques in the dental office. J Am Dent Assoc. 1994;125:1475–1484. [DOI] [PubMed] [Google Scholar]
- 18.Secker-Walker RH, Chir B, Solomon LJ, Flynn BS, Dana GS. Comparisons of the smoking cessation counseling activities of six types of health professionals. Prev Med. 1994;23:800–808. [DOI] [PubMed] [Google Scholar]
- 19.Hayes C, Kressin N, Garcia R, Mecklenburg R, Dolan T. Tobacco control practices: how do Massachusetts dentists compare with dentists nationwide? J Massachusetts Dent Soc. 1997;46:9–14. [PubMed] [Google Scholar]
- 20.Gould KA, Eickhoff-Shemek JM, Stacy RD, Mecklenburg RE. The impact of National Cancer Institute training on clinical tobacco use cessation services by oral health teams. J Am Dent Assoc. 1998;129:1442–1449. [DOI] [PubMed] [Google Scholar]
- 21.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. [DOI] [PubMed] [Google Scholar]
- 22.Martin LM, Bouquot JE, Wingo PA, Heath CW. Cancer prevention in the dental practice: oral cancer screening and tobacco cessation advice. J Public Health Dent. 1996;56:336–340. [DOI] [PubMed] [Google Scholar]
- 23.How to Help Your Patients Be Tobacco Free: Trainers Guide. Rockville, Md: Public Health Service; 1997.
- 24.Severson HH, Eakin EG, Stevens VJ, Lichtenstein E. Dental office practices for tobacco users: independent practice and HMO clinics. Am J Public Health. 1990;80:1503–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]