Abstract
Objectives. We examined the association between attributes of primary care providers and care for depression, from a patients’ perspective, among a sample of predominantly low-income African American women.
Methods. Computer-assisted telephone interviews were conducted among a population-based sample of 1202 women residing in Washington, DC.
Results. Respondents whose primary care physicians provided more comprehensive medical services were more likely to be asked about and treated for depressive symptoms than women whose providers were less medically comprehensive. Women who rated their providers as having more respect for them also were more likely to be asked about and treated for depression.
Conclusions. More comprehensive primary care delivery and a physician–patient relationship focused on mutual respect are associated with greater rates of physician inquiry about and treatment for depression among vulnerable women.
Depression, a common and often chronic disorder, is expected to become the second greatest cause of disability worldwide over the next decade.1,2 Depressive symptoms, with or without major depressive disorder, can impair functioning to levels comparable to or worse than those seen with chronic medical conditions such as congestive heart failure, diabetes, angina, and arthritis.3,4 Despite the chronic and debilitating course of this disorder and the existence of efficacious interventions,5 most people with depression fail to seek mental health care; those who do seek care are most frequently seen in primary health care settings rather than psychiatric settings.6–8
Unfortunately, depression is underrecognized and undertreated in these general medical care settings,9–11 and there are inconsistencies in the process and quality of care for depression in primary care practices.12 Therefore, an understanding of factors that influence identification and care for depression in this setting is important. Lower-income and non-White women are particularly unlikely to seek care in mental health settings13; they are more likely to seek help from primary health care providers than are wealthier women and White women.14 Yet, primary care providers are less likely to diagnose depression among African American women than among White women.10,15
Although research has examined primary care providers’ knowledge and communication style as factors in identifying depression, little is known about the attributes of primary care delivery systems as they relate to recognition and treatment of this condition. Because lower-income African American women are less likely to use mental health specialty providers than primary care providers for their psychosocial needs,13,14 we hypothesized that, among these women, those whose primary care providers offered more medically comprehensive services would be more likely to have their psychosocial needs met.
In addition, we hypothesized that women whose primary care providers were more accessible, in terms of availability of appointments, hours of operation, and women’s ability to reach them by telephone, would be more likely to be asked about depressive symptoms. Previous studies have shown that better access enhances the likelihood of receipt of needed health care, first-contact care with a primary care provider, and provider continuity.16,17 We examined, among a community sample of predominantly low-income, African American women, associations between primary care attributes and care for depression, both assessed from the patient’s perspective.
METHODS
We identified a population-based sample of women residing in Washington, DC, census tracts where at least 30% of households had incomes below 200% of the 1999 poverty threshold.18 A professional sampling system (Genesys; Georgetown University Medical Center, Washington, DC, and Johns Hopkins School of Public Health, Baltimore, MD) generated a list of telephone numbers designed to provide a sample of 25% random-digitdialing and 75% targeted households. The random-digit-dialing sample was generated from the set of telephone exchanges that serviced lower-income census tracts in Washington, DC. A listed household sample was merged with demographic information, derived from census and marketing data, that targeted our inclusion criteria.
In addition to questions regarding mental health services, the telephone survey used in this study gathered information on respondents’ use of cancer screening services; as a result, only women older than 40 years were eligible for participation. We developed the survey with focus groups, results of previous research,19–24 and pilot testing. It contained items gathering information on women’s primary care experiences, demographic and socioeconomic characteristics, insurance, health status, and depressive symptoms. Interviews were conducted during January through March 2000 by experienced, trained female interviewers. Further details regarding the design of the survey are available elsewhere.25 The response rate was 85%.
Dependent Variables
Three dichotomous items assessed whether respondents had been asked about depressive symptoms (“Has your regular doctor ever asked if you were feeling down, depressed, or nervous?”), had been treated with medication for depression (“Has your regular doctor ever treated you with medication for being depressed or for helping you with your mood?”), or had undergone counseling for depression suggested to them by their primary care provider (“Has your regular doctor ever suggested that you talk with a counselor to help you with your mood?”). The 2 items assessing treatment were not mutually exclusive, and they were combined in the analyses; women with a positive response to either item were categorized as having had “treatment” recommended. Together, the 3 outcomes just described are termed “care for depression.”
Independent Variables
Primary care. The main independent variables of interest were the primary care variables. We defined primary care with the Institute of Medicine’s definition: “provision of integrated, accessible health care services by physicians that are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community.”26 The key attributes of primary care thus include organizational, financial, and geographic accessibility; comprehensive service delivery; a strong patient–provider relationship; continuity with a provider; and coordination of specialty care.26–27
On the basis of our pilot testing, we adapted items from the Primary Care Assessment Survey in developing our primary care variables.19 Because our survey was administered by telephone to a sample that involved a relatively low literacy rate, it was necessary, in the case of certain items, to decrease the number of response options from 6 to 4. Scales were not created; rather, each primary care item was assessed as a separate “predictor” of the dependent variables (inquiry about and treatment for depressive symptoms). We retained the individual variables so that we would be able to ascertain the particular aspects of each primary care domain that were associated with each outcome. Hence, use of individual primary care items allowed us more insight than use of general scales would have provided. Responses to each item were dichotomized, at the median, into “lower” and “higher” amounts of the primary care characteristic in question. Women’s perceptions of their practice’s primary care features were assessed as follows.
Accessibility was operationalized according to the techniques of previous studies.17 Financial accessibility was assessed with a single item asking about the amount of money women paid for office visits. Geographic accessibility was assessed with a single item focusing on women’s ratings of the convenience of their regular doctor’s office location. Organizational accessibility (factors involved in arranging and promoting encounters between patients and providers25) was assessed with 4 items: appointment availability, appointment delays, ease of telephone communication, and amount of physician time with the patient.
The first aspect of comprehensive service delivery, overall comprehensiveness, was assessed with the following questions: “Thinking about how well your doctor knows you, how would you rate your regular doctor’s ability to take care of all of your health care needs? Would you say it is poor, fair, good, or excellent?” The second aspect of comprehensive delivery was comprehensiveness of medical counseling (i.e., regarding smoking, alcohol use, and diet). The third aspect was comprehensiveness of evidence-based medical screening services (cholesterol, blood pressure, height and weight, clinical breast examination and mammogram). The fourth aspect was thoroughness of problem-focused physical examinations.
Using recognized conceptualizations of the patient–provider relationship,26,28–31 we included 5 items that assessed 3 aspects of this relationship: communication, trust, and compassion. Communication was assessed with a question asking the respondent how she would rate her regular doctor’s explanations of her health problems or treatment. Responses were made on a 4-point scale in which response options ranged from poor to excellent. Trust was assessed with a single item: “All things considered, how much do you trust your doctor, on a scale from 0 to 10, where 0 is not at all and 10 is completely.” Compassion was assessed with items asking women to rate their regular provider’s (1) patience with their questions or worries, (2) care and concern for them, and (3) respect for them. Each item involved the same 4 response options, ranging from poor to excellent. Item responses were dichotomized at the median. All of the concepts just described were measured in the context of the global patient–provider relationship; items were not visit specific.
Coordination of specialty care was assessed with women’s ratings of their regular physician’s help in obtaining appointments with specialists, involvement in their care when they were hospitalized or under a specialist’s care, and help in understanding specialists’ recommendations or directions. This variable was assessed only among the 748 women who had been referred to a specialist or hospitalized by their regular physician.
Continuity of care included the degree to which women’s office visits involved the same clinician (visit continuity) and the duration of that relationship with the clinician (longitudinal continuity). Visit continuity was assessed through determination of whether the woman had a usual site of primary care, and if so, whether she had a regular clinician at that site whom she saw for most of her visits. As a means of assessing relationship duration, women were asked, “How long has this person/place been your doctor/source of care?”
Depression status. Survey respondents completed the depression module of the Patient Health Questionnaire from the Primary Care Evaluation of Mental Disorders (PRIME-MD), a reliable and validated screening instrument24 that assesses specific disorders according to criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. The PRIME-MD23,24 has been widely used in clinical research, and items can be read to the patient if necessary.21 The interview format has been used in previous studies involving lower-income women and members of ethnic minority groups.7,32 Results from the PRIME-MD were used to classify individuals into 1 of 3 groups: no depression, minor depression, or major depression.
Control Variables
Control variables included demographic and socioeconomic characteristics such as age, household income, race/ethnicity, education, and health, employment, and insurance status. Insurance categories were uninsured, public insurance only, and private. To be considered “uninsured,” a woman had to have lacked coverage for the entire 12 months before the interview.
Four hundred fifty-five women in the sample (37.8%) had Medicare coverage. Of these women, those with no additional supplementary health insurance plan (i.e., Medi-Gap) (includes those with Medicare part B coverage) were categorized as having public insurance coverage only. Women who had Medicaid and no additional private insurance coverage were classified as “public only.” Women who had a Medi-Gap policy in addition to Medicare coverage were categorized as having private insurance coverage and public coverage as well. These categories allowed us to distinguish between women with and without additional private insurance coverage above and beyond that provided by Medicaid or Medicare.
We also measured the number of visits women had had with their regular provider in the previous year. This “visit frequency” variable was included as a covariate in the models, the reason being that an increased number of visits implies more opportunities for contact and inquiry regarding depressive symptoms.
Data Analysis
We used χ2 tests to assess significance in cross tabulations. We conducted stratified analyses to detect possible interaction effects, focusing special attention on potential interactions between insurance and the 2 independent variables of primary interest, organizational access and comprehensiveness of medical services. All demographic, socioeconomic, health status, primary care, visit frequency, insurance, and plan type characteristics that were conceptually important and contributed to the fit of the model were used as covariates in the logistic regression analyses.33 We conducted bivariate logistic regression analyses to assess the effect of each individual primary care domain on care for depression, adjusting for age, education, income, health status, depression status, insurance coverage, and frequency of primary care visits. We then computed full models (1 with the outcome of inquiry regarding care for depression and 1 with the outcome of treatment for depression) that adjusted for the same covariates but also included all of the primary care domains so that we could obtain adjusted “full model” odds ratios.
RESULTS
Sample Characteristics and Prevalence of Depressive Symptoms
Table 1 ▶ describes the study population, 82.7% of which was African American. The percentage of women in the 41- to 64-year age group (13.2%) who were uninsured was slightly higher than the national rate (7%) for this group.34 The majority of respondents (62%) used a private doctor or a health maintenance organization; 27% visited community health centers or other nonprofit community health clinics. According to the PRIME-MD, 4.7% of the sample screened positive for major depression, and 19.7% screened positive for minor depression. Higher percentages of younger and poorer women were depressed (Table 1 ▶).
TABLE 1—
Characteristics of the Study Population: Washington, DC, 2000.
| Characteristic | Overall (n = 1205), % | Nondepressed (n = 908), % | Minor or Major Depression (n = 294), % |
| Age, y | |||
| 41–64 | 44.7 | 43.1 | 46.0 |
| ≥ 65 | 55.3 | 56.9 | 54.0 |
| Education, y | |||
| < 12 | 26.3 | 23.5 | 32.6a |
| 12 | 33.5 | 33.0 | 35.9 |
| ≥ 12 | 40.2 | 43.5 | 31.2a |
| Income, $ | |||
| Don’t know/refused | 26.9 | 27.1 | 27.4 |
| ≤ 30 000 | 42.5 | 39.3 | 48.9a |
| > 30 000 | 30.6 | 33.6 | 23.6a |
| Race/ethnicity | |||
| Black/African American | 82.7 | 82.0 | 84.8 |
| White | 6.6 | 7.4 | 4.6 |
| Hispanic/other | 3.7 | 3.6 | 4.2 |
| Refused | 7.0 | 6.9 | 6.3 |
| Owns home | 66.2 | 69.8 | 58.8a |
| Work status | |||
| Retired/disabled | 62.6 | 62.3 | 66.1 |
| Working full–time | 24.3 | 25.1 | 19.5 |
| Other | 13.6 | 12.6 | 14.4 |
| Married/living as married | 26.5 | 27.0 | 22.5 |
| Poor/fair health status (self-assessed) | 26.2 | 20.6 | 39.4a |
| Has a regular medical practitioner | 84.8 | 85.1 | 86.4 |
| Health insurance for any period during past 12 mo | |||
| Public only | 22.8 | 19.6 | 28.8a |
| Private (may include Medicare/Medicaid) | 67.9 | 71.6 | 60.2a |
| Uninsured for entire past 12 mo | 9.3 | 8.8 | 11.0 |
Note. Three women were missing information on the Primary Care Evaluation of Mental Disorders, so the sample size was 1202 for this variable.
aχ2P = .001 for comparison of percentages between depressed and nondepressed women.
Consistent with previous studies,9–11 rates of inquiry about and treatment for depression were low (Figure 1 ▶), even though 98% of depressed women reported at least 1 visit to their primary care provider in the previous 12 months and 70.4% reported more than 2 such visits. Presence of depressive symptoms was the factor most consistently associated with recognition and treatment of depression on the part of primary care practitioners (P = .001).
FIGURE 1—
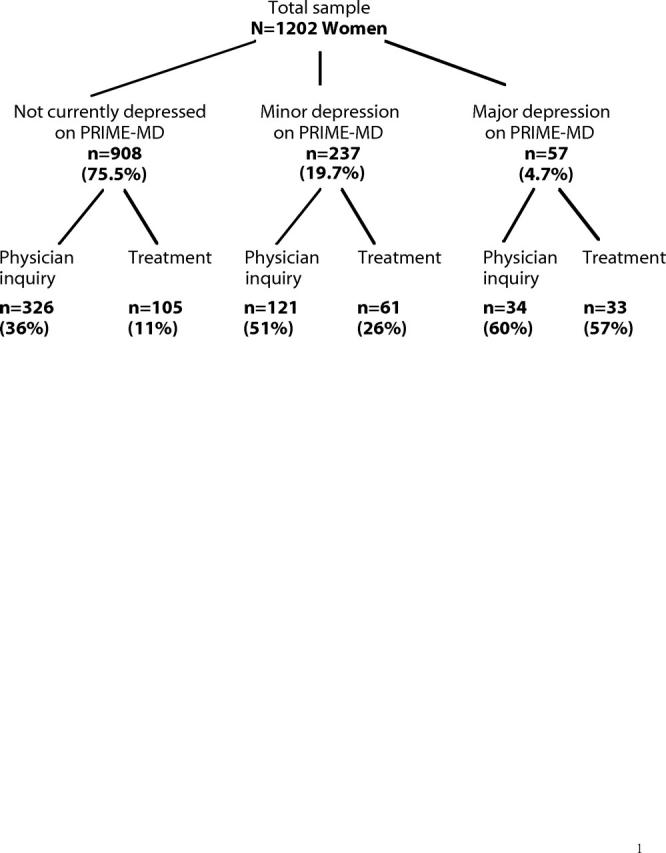
Study women’s prevalence of depression on the PRIME-MD and their primary care physicians’ inquiries about and recommendations of treatment for depression.
Association of Primary Care Attributes With Care for Depression
Table 2 ▶ presents adjusted odds of one’s regular provider inquiring about depressive symptoms according to primary care characteristics. Accessibility, comprehensiveness of medical care, patient–provider communication, coordination of specialty care, and duration of relationship with one’s primary care provider were each individually associated with such inquiries in the bivariate models adjusting for age, socioeconomic status, depression status, health status, frequency of primary care visits, and insurance status. In the models that included all of the primary care characteristics, certain variables stood out as being significantly associated with physician inquiries: comprehensiveness of care, having a more respectful provider, and having a sustained relationship with one’s provider.
TABLE 2—
Women’s Odds of Being Asked About Depression by Their Primary Care Physicians, by Primary Care Characteristics (n = 1202)
| Primary Care Characteristic | Bivariate Odds Ratio | Full Model Odds Ratio |
| Organizational accessibility | ||
| Office hours/appointment availability | 1.04 | 0.73 |
| Waiting time for appointments | 1.52** | 1.20 |
| Ability to reach the office by telephone | 1.48** | 0.94 |
| Amount of time spent with physician | 1.64** | 1.10 |
| Comprehensiveness of medical services | ||
| Ability of physician to address health care needs | 1.66** | 1.00 |
| Thoroughness of physical examination | 1.79** | 1.44* |
| Screening in past year | 1.50* | 1.33* |
| Counseling comprehensiveness in past year | 3.12** | 3.05** |
| Patient–physician relationship: communication | ||
| Explanations of health problems or treatments | 1.56** | 0.91 |
| How often questions were left unanswered | 1.12 | 0.93 |
| Patient–physician relationship: trust | ||
| Extent to which physician trusted | 1.48** | 1.12 |
| Belief that physician’s primary concern is holding down costs (reference group: women responding affirmatively) | 0.89 | 1.18 |
| Patient–physician relationship: compassion | ||
| Physician is patient with questions or worries | 1.79** | 1.25 |
| Physician is caring | 1.96** | 1.19 |
| Physician is respectful | 2.00** | 1.78** |
| Coordination of carea | ||
| Help from physician in obtaining appointment with specialist | 1.43** | 0.89 |
| Involvement of physician in treatment by specialist or hospitalization | 1.64** | 1.14 |
| Physician helped provide an understanding of specialist’s or other doctor’s recommendations or directions | 1.59** | 1.12 |
| Continuity of care | ||
| Has usual site of primary care (reference group: no site) | 2.09 | 1.43 |
| Presence of regular practitioner at site of care | 1.41 | 1.50 |
| Visit continuity (more vs fewer visits with same practitioner) | 1.22 | 1.60 |
| Duration of relationship more than 2 years (reference group: fewer than 2 years) | 1.39** | 1.30* |
Note. Unless otherwise noted, reference groups were those possessing fewer of the primary care characteristics. “Bivariate” odds ratios were obtained from bivariate logistic regression analyses that included 1 primary care variable along with all of the following covariates: age, depression status, income, education, health status, insurance status, and frequency of primary care visits. “Full model” odds ratios adjusted for age, depression status, income, education, health status, insurance coverage, frequency of primary care visits, and all of the primary care features included in the first column.
aCoordination of care items were completed only by the 748 women whose regular physicians had recommended that they see a specialist or who were hospitalized.
*P < .05; **P ≤ .01.
Table 3 ▶ presents the adjusted odds of receiving treatment for depression. Comprehensiveness of medical services, provider compassion, and coordination of specialty care were positively associated with treatment recommendation in the bivariate models. In the full model, which also included all primary care characteristics, comprehensiveness of care and having a more respectful provider were significantly associated with treatment for depression.
TABLE 3—
Women’s Odds of Being Treated for Depression by Their Primary Care Physicians, by Primary Care Characteristics (n = 1202)
| Primary Care Characteristic | Bivariate Odds Ratio | Full Model Odds Ratio |
| Organizational accessibility | ||
| Office hours/appointment availability | 1.15 | 1.21 |
| Waiting time for appointments | 1.06 | 0.95 |
| Ability to reach the office by telephone | 0.82 | 0.64 |
| Amount of time spent with physician | 1.15 | 1.08 |
| Comprehensiveness of medical services | ||
| Ability of physician to address health care needs | 1.47** | 1.34 |
| Thoroughness of physical examination | 1.42* | 1.42 |
| Screening in past year | 0.79 | 1.47* |
| Counseling comprehensiveness in past year | 2.03** | 1.64** |
| Patient–physician relationship: communication | ||
| Explanations of health problems or treatments | 0.87 | 0.41 |
| Frequency at which questions left unanswered | 0.69 | 0.58 |
| Patient–physician relationship: trust | ||
| Extent to which physician trusted | 1.23 | 1.44 |
| Belief that physician’s primary concern is holding down costs (reference group: those responding affirmatively) | 1.00 | 1.18 |
| Physician is patient with questions or worries | 1.33 | 1.32 |
| Physician is caring | 1.42* | 0.99 |
| Physician is respectful | 1.47* | 2.04** |
| Coordination of carea | ||
| Help from physician in obtaining appointment with specialist | 1.42* | 1.30 |
| Involvement of physician in treatment by specialist or hospitalization | 1.59** | 1.16 |
| Physician helped provide an understanding of specialist’s or other doctor’s recommendations or directions | 1.51** | 1.07 |
| Continuity of care | ||
| Has usual site of primary care (reference group: no site) | 1.97 | 0.75 |
| Presence of regular practitioner at site of care | 1.05 | 0.82 |
| Visit continuity (more vs fewer visits with the same practitioner) | 0.91 | 0.83 |
| Duration of relationship more than 2 years (reference group: fewer than 2 years) | 1.05 | 1.14 |
Note. Unless otherwise noted, the reference group (odds ratio of 1) for all primary care variables was the lower category. For example, women’s ratings of comprehensiveness of screening services were dichotomized into lower vs higher, with lower as the reference group. “Bivariate” odds ratios were obtained from bivariate logistic regression analyses that included 1 primary care variable along with all of the following covariates: age, depression status, income, education, health status, insurance status, and frequency of primary care visits. “Full model” odds ratios adjusted for age, depression status, income, education, health status, insurance coverage, frequency of primary care visits, and all of the primary care features included in the first column.
aCoordination of care items were answered only by the 748 women whose regular physicians had recommended that they see a specialist or who were hospitalized.
*P < .05; **P ≤ .01.
In all of the analyses, depression status was the variable most strongly associated with likelihood of receiving care for depression from a primary care provider. Women with better self-assessed physical health status had lower odds of being asked about and treated for depression. Consistent with earlier research,35 having public insurance coverage was positively associated with one’s regular provider inquiring about and recommending treatment for depression. Privately insured women were about half as likely as publicly insured women to have treatment for depression recommended by their primary care provider (P < .01) after adjustment for depression status (data not shown).
Neither financial nor geographic accessibility of primary care was associated with provider inquiry about or treatment for depression. Whereas insured women exhibited no significant differences in rates of provider inquiry according to accessibility, there were differences among women who were uninsured. Uninsured women were more likely to be asked about depressive symptoms if their providers were more accessible (specifically, if the women encountered shorter waits for appointments, were better able to contact their provider by telephone, and reported more satisfaction with the length of their clinical encounters). When this “interaction” between organizational access and insurance was included in the logistic regression analyses, it did not alter the results.
DISCUSSION
In this study, we examined whether specific attributes of primary care settings were associated with care for depression. Among the urban, low-income, predominantly African American women who took part in our study, those whose primary care providers provided more comprehensive medical services were significantly more likely to be asked about and treated for depression. In addition, women who perceived their primary care providers as being more respectful and women who had a sustained relationship with a provider had higher odds of being asked about and treated for depression.
Women whose primary care providers met more of their medical (physical) needs were more likely to obtain care for their psychosocial needs in regard to depression. To our knowledge, there is little literature exploring this relationship. One study assessed the mental health needs of young women and the extent to which their public-sector gynecological clinics provided comprehensive medical care.7 However, that study did not examine the extent to which comprehensiveness of medical services was associated with being asked about or treated for those mental health needs.
In our study, not only the counseling aspects of comprehensiveness (e.g., counseling regarding tobacco and alcohol use and diet) but also the noncounseling aspects (e.g., height, weight, cholesterol, blood pressure screening) were associated with care for depressive symptoms. These findings suggest that care for depression is 1 element of the overall comprehensiveness of primary care practices. There is a need for further research investigating why some primary care practices offer a broader range of services than others.
Provider accessibility, although important in encouraging first-contact care,17 was not associated with care for depression except in the case of uninsured women. Among these women, having more accessible providers was associated with higher rates of provider inquiries about depression. Many women may not seek primary care services because of depressive symptoms but may raise mental health concerns during the course of visits made for other reasons.
Continuity has been well documented as a feature important to patients36 and has been associated with better health outcomes, including enhanced recognition of a patient’s health needs.26,27 Patients who have a continuous relationship with a regular provider have better access to care.37 Accordingly, in our study, women who had sustained relationships with their primary care providers were more likely to be asked about depression.
Respect appears to be an important attribute of patient-centered care among lowincome, minority women. As was the case with earlier investigations,38,39 our study revealed associations between interpersonal aspects of the patient–provider relationship and care for depression. Women who perceived their providers as being more respectful were more likely to receive care for depression. The fact that women who were more often asked about depression also rated their providers as more respectful implies that providers should not be concerned that asking women about depressive symptoms will insult them.
Limitations of this study include the reliance on self-reported data without medical record validation, the possibility of recall bias, the cross-sectional study design, and the absence of information on primary care providers’ knowledge about and attitudes toward depression. Because we did not collect data from primary care providers, we lacked specific information on whether women’s health plans offered mental health “carve-out” benefits—that is, contracts with other organizations to provide mental health services in settings other than primary care. Women with previously recognized depression whose plans include carve-out benefits would not be expected to receive depression treatment from their primary care providers.40 Nonetheless, women who fail to recognize their own depressive symptoms often present to the primary care setting with physical complaints, and the primary care provider is often their only contact with the health care system.
In addition, we did not assess race concordance between patients and providers. Previous research has shown that African Americans rate quality of interpersonal care higher in race-concordant patient–provider relationships.41 If such race concordance, or its absence, had any effects on care for depression, we were unable to control for them. Finally, given the multiple individual comparisons made in our analyses, some of the associations noted may have been due to chance. However, the consistency of the findings across items within domains and across outcomes decreases the likelihood that these findings are spurious.
Because our study was community based, the respondents exhibited varying levels of access to and use of primary care; this strategy ensured that the voices of women with less access to primary care were heard. It also allowed us to include nondepressed women. Inclusion of our nondepressed comparison group allowed us, in turn, to adjust for potential negative bias among depressed patients, whose ratings of care might reflect their own affect rather than the actual quality of care received. Inclusion of items assessing specific features of primary care is important in a study of depressive symptoms among women with varying levels of access. Whereas there is a sizable literature on specific features of primary care as they relate to physical health status, preventable medical hospitalizations, and use of clinical preventive services,42–45 fewer investigations have focused on specific features of primary care as they relate to treatment for depression.
The results of this study have additional implications for care for depression among lower-income women. The association between duration of patient–physician relationship and physician inquiries about depressive symptoms highlights the importance of this basic tenet of primary care. When patients are forced to change their regular primary care providers—a frequent occurrence, especially among members of lower-income groups with transient insurance coverage or changes in employment—their relationships with their providers, and the coordination of their care, suffer.46 Such disruptions in care may have negative implications for recognition and treatment of depression among these groups.
In summary, rates of primary care provider inquiries about and treatment for depression were low in this sample of urban, low-income, predominantly African American women. Women with primary care providers who offered more comprehensive services, in terms of meeting all of these women’s medical needs, were significantly more likely to be asked about and treated for depression. Aspects of the patient–provider relationship, such as whether women were treated with respect, were also associated with inquiry about and treatment for depression. In addition, women with sustained relationships with their primary care providers were more likely to be asked about depression.
Research on improving care for depression needs to further explore the mechanisms and temporal aspects of the relationships between primary care attributes and treatment for depression. Should such relationships be confirmed, health care plans might consider structuring themselves to promote comprehensive service delivery and to foster continuity of care and strong patient–provider relationships. In terms of quality improvement efforts, current interventions directed at primary care providers focus on improving providers’ knowledge of depression treatment guidelines. Our findings suggest the possibility that future interventions targeting providers should incorporate patient-centered communication skills training, especially in the area of relationship building.
Acknowledgments
This work was funded in part by the National Institute of Mental Health (grant 24 MH 57909), by the US Department of the Army (grant 17-97-1-7131), and by the National Cancer Institute (grant RO3 CA83338-02).
We thank Patrick G. O’Malley, MD, MPH, and the anonymous reviewers for their valuable comments on earlier versions of this article.
Human Participant Protection
Ethical clearance for this survey was obtained from the institutional review board of Georgetown University Medical Center.
Contributors
A. S. O’Malley developed the research hypothesis and the survey instrument, obtained funding for the study, carried out the statistical analyses, and wrote the article. C. B. Forrest assisted in the development of the instrument and in revisions of the article. J. Miranda assisted in revisions of the article.
Peer Reviewed
References
- 1.Murray CJ, Lopez AD. Evidence-based health policy—lessons from the Global Burden of Disease Study. Science. 1996;274:740–743. [DOI] [PubMed] [Google Scholar]
- 2.Sartorius N, Ustun TB, Costa e Silva JA, et al. An international study of psychological problems in primary care. Arch Gen Psychiatry. 1993;50:819–824. [DOI] [PubMed] [Google Scholar]
- 3.Wells KB, Steward A, Hays RD, et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA. 1989;262:914–919. [PubMed] [Google Scholar]
- 4.Hays RD, Wells KB, Sherbourne CD, Roger W, Spritzer K. Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry. 1995;52:11–19. [DOI] [PubMed] [Google Scholar]
- 5.Depression in Primary Care, Volume 2: Treatment of Major Depression. Rockville, Md: Agency for Health Care Policy and Research; 1993.
- 6.Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and service use. Arch Gen Psychiatry. 1993;50:85–94. [DOI] [PubMed] [Google Scholar]
- 7.Miranda J, Azocar F, Komaromy M, Golding M. Unmet health needs of women in public-sector gynecologic clinics. Am J Obstet Gynecol. 1998;178:212–217. [DOI] [PubMed] [Google Scholar]
- 8.Miranda J, Green B. The need for mental health services research focusing on poor young women. J Ment Health Policy Economics. 1999;2:73–80. [DOI] [PubMed] [Google Scholar]
- 9.Von Korff M, Shapiro S, Burke JD, et al. Anxiety and depression in a primary care clinic: comparison of Diagnostic Interview Schedule, General Health Questionnaire, and practitioner assessments. Arch Gen Psychiatry. 1987;44:152–156. [DOI] [PubMed] [Google Scholar]
- 10.Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States. J Gen Intern Med. 2000;15:284–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perez-Stable E, Miranda J, Munoz RF, Ying YW. Depression in medical outpatients: underrecognition and misdiagnosis. Arch Intern Med. 1990;150:1083–1088. [DOI] [PubMed] [Google Scholar]
- 12.Wells KB, Schoenbaum M, Unutzer J, Lagomasino IT, Rubenstein LV. Quality of care for primary care patients with depression in managed care. Arch Fam Med. 1999;8:529–536. [DOI] [PubMed] [Google Scholar]
- 13.Leaf P, Livingston M, Tischler G, et al. Contact with health professionals for the treatment of psychiatric and emotional problems. Med Care. 1985;23:1322–1337. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, Zhao S, Blazer DG, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord. 1997;45:19–30. [DOI] [PubMed] [Google Scholar]
- 15.Borowsky SJ, Rubenstein LV, Meredith LS, Camp P, Jackson-Triche M, Wells KB. Who is at risk of nondetection of mental health problems in primary care? J Gen Intern Med. 2000;15:381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berk ML, Schur CL, Cantor JC. Ability to obtain health care: recent estimates from the Robert Wood Johnson Foundation National Access to Care Study. Health Aff (Millwood). 1995;14:139–146. [DOI] [PubMed] [Google Scholar]
- 17.Forrest CB, Starfield B. Entry into primary care and continuity: the effects of access. Am J Public Health. 1998;88:1330–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The 1999 HHS poverty guidelines. Federal Register. 1999;64:13428–13430. [Google Scholar]
- 19.Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–739. [DOI] [PubMed] [Google Scholar]
- 20.Stewart AL, Ware JE, eds. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992.
- 21.National Center for Health Statistics. National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis.htm. Accessed January 14, 2003.
- 22.O’Malley AS, Forrest CB, O’Malley PG. Lowincome women’s priorities for primary care. J Fam Pract. 2000;49:141–146. [PubMed] [Google Scholar]
- 23.Spitzer RL, Williams JBW, Kroenke W, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 24.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. [DOI] [PubMed] [Google Scholar]
- 25.O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations: the roles of primary care, health insurance, and HMOs. J Gen Intern Med. 2002;17:144–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Institute of Medicine. Primary Care: America’s Health in a New Era. Washington, DC: National Academy of Sciences; 1996.
- 27.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York, NY: Oxford University Press Inc; 1998.
- 28.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA. 1992;267:2221–2226. [PubMed] [Google Scholar]
- 29.Quill TE. Partnerships in patient care: a contractual approach. Ann Intern Med. 1983;98:228–234. [DOI] [PubMed] [Google Scholar]
- 30.Thom DH, Campbell B. Patient-physician trust: an exploratory study. J Fam Pract. 1997;44:169–176. [PubMed] [Google Scholar]
- 31.Emanuel EJ, Dubler NN. Preserving the physician-patient relationship in the era of managed care. JAMA. 1995;273:323–329. [PubMed] [Google Scholar]
- 32.Bosworth HB, Parsey KS, Butterfield MI, et al. Racial variation in wanting and obtaining mental health services among women veterans in a primary care clinic. J Natl Med Assoc. 2000;92:231–236. [PMC free article] [PubMed] [Google Scholar]
- 33.Zheng B, Agresti A. Summarizing the predictive power of a generalized linear model. Stat Med. 2000;19:1771–1781. [DOI] [PubMed] [Google Scholar]
- 34.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069. [DOI] [PubMed] [Google Scholar]
- 35.Glied S. Too little time? The recognition and treatment of mental health problems in primary care. Health Serv Res. 1998;33:891–910. [PMC free article] [PubMed] [Google Scholar]
- 36.Kibbe DC, Bentz E, McLaughin CP. Continuous quality improvement for continuity of care. J Fam Pract. 1992;36:304–308. [PubMed] [Google Scholar]
- 37.Lambrew JM, DeFriese GH, Carey TS, et al. The effects of having a regular doctor on access to primary care. Med Care. 1996;34:138–151. [DOI] [PubMed] [Google Scholar]
- 38.Meredith LS, Orlando M, Humphrey N, Camp P, Sherbourne CD. Are better ratings of the patient-provider relationship associated with higher quality of care for depression? Med Care. 2001;39:349–360. [DOI] [PubMed] [Google Scholar]
- 39.Cooper LA, Brown C, Vu HT, et al. Primary care patients’ opinions regarding the importance of various aspects of care for depression. Gen Hosp Psychiatry. 2000;22:163–173. [DOI] [PubMed] [Google Scholar]
- 40.Goldman LS, Nielsen NH, Champion HC, for the Council on Scientific Affairs, American Medical Association. Awareness, diagnosis and treatment of depression. J Gen Intern Med. 1999;14:569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–589. [DOI] [PubMed] [Google Scholar]
- 42.Bindman AB, Grumbach K, Osman D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–311. [PubMed] [Google Scholar]
- 43.Lurie N, Ward NB, Shapiro MR, Brook RH. Termination from Medi-Cal—does it affect health? N Engl J Med. 1984;311:480–484. [DOI] [PubMed] [Google Scholar]
- 44.Bindman AB, Grunbach K, Osmond D, Vranizan K, Stewart A. Primary care and receipt of preventive services. J Gen Intern Med. 1996;11:260–276. [DOI] [PubMed] [Google Scholar]
- 45.Flocke SA, Stange KC, Zyanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(suppl 8):AS21–AS30. [DOI] [PubMed] [Google Scholar]
- 46.Flocke S, Stange KC, Zyzanski SJ. The impact of insurance type and forced discontinuity on the delivery of primary care. J Fam Pract. 1997;45:129–135. [PubMed] [Google Scholar]


