Abstract
Objectives. We evaluated self-perceived access to health care in a cohort of Medicare beneficiaries.
Methods. We identified patterns of use and barriers to health care from self-administered questionnaires collected during the 1993–1994 annual examination of the Cardiovascular Health Study.
Results. The questionnaires were completed by 4889 (91.1%) participants, with a mean age of 76.0 years. The most common barriers to seeing a physician were the doctor’s lack of responsiveness to patient concerns, medical bills, transportation, and street safety. Low income, no supplemental insurance, older age, and female gender were independently related to perceptions of barriers. Race was not significant after adjustment for other factors.
Conclusions. Psychological and physical barriers affect access to care among the elderly; these may be influenced by poverty more than by race.
Disparity in access to health care among nonelderly Americans has been well documented. The primary reason for this disparity is lack of health insurance, either employer-sponsored or public.1–5 Approximately 16% of Americans aged younger than 65 years were uninsured in 2000.6 A large percentage of working-age Americans without coverage have histories of chronic conditions, including diabetes, heart disease, and depression.2 The vast majority of these people delayed or did not receive needed care because of cost. Although the most important factor affecting the ability to use health services in the nonelderly is lack of insurance, other factors have also emerged. Factors highly correlated with lack of insurance, including race, income, and other sociodemographic characteristics, have been associated with lower health care use in younger populations.7–9
Although there is a perception of greater equality regarding access to health care in older Americans because of the provision of Medicare, recent studies have concluded otherwise.10–15 Cost appears to be one of the major factors associated with lack of access to care. Between 1995 and 1997, approximately 11% of Medicare beneficiaries reported delaying care because of cost or because they had no specific source of care.13 Because out-of-pocket expenses are the greatest financial burden for Medicare recipients, issues of cost in the elderly are primarily related to insurance coverage supplemental to Medicare. Type of insurance has been reported to be independently related to both use of health services and medical outcomes.11,14 In addition to lack of complementary health insurance, evidence is accumulating that other sociodemographic factors may affect the health care services received by individuals aged 65 years and older, including race, education, age, and gender.10,12–15 It is also becoming evident that satisfaction with provider services may impact perceptions of access to health care16,17 and clinical outcomes.18,19
Data regarding characteristics of Medicare recipients and perceptions of barriers to care are needed to better understand this complex issue. The Cardiovascular Health Study (CHS), with a longitudinal cohort drawn from Medicare enrollment files in 1989–1990 and 1992–1993,20 included a self-administered questionnaire on access and barriers to health care at the annual examination completed in 1993–1994. Using these data, we were able to investigate the following questions: Where do the elderly receive their medical care, and how easily are they able to be seen by a physician? What are the self-perceived barriers affecting the ability of elderly patients to see a physician? Are socioeconomic characteristics associated with self-reported barriers to care?
METHODS
Study Population and Design
The CHS participants included 5888 men and women aged 65 years or older who were randomly selected from Medicare eligibility lists in 4 communities: Forsyth County, NC; Sacramento County, Calif.; Washington County, Md.; and Allegheny County, Pa.20 Eligibility requirements for participants included not being institutionalized or wheelchair-dependent, able to provide informed consent, not under treatment for cancer at the time of enrollment, and planning to remain in their respective geographic regions for at least 3 years.21 Other eligible individuals within the same household as a sampled participant were also recruited into the study. The institutional review board at each participating center approved the study, and each participant gave informed consent. In 1989–1990, 5201 participants were recruited and completed a baseline examination; in 1992–1993, an additional 687 African American participants were enrolled. At baseline, an extensive confirmation of self-reported cardiovascular disease was performed.22
The CHS study design and objectives have been published previously.20 The baseline examination included collection of demographic data, standardized medical history questionnaires, physical examination, anthropometry, blood pressure measurement, cognitive testing, psychosocial questionnaires including instruments for social support and network and depression, resting electrocardiography, spirometry, and laboratory analyses after phlebotomy. Follow-up contact occurred every 6 months, alternating between telephone calls and clinic visits. Nine additional clinical examinations were performed through 1998–1999. Surveillance for all hospitalizations with extensive medical record collection for cardiovascular events was initiated and continues to be conducted.23
Questions on Access to Health Care
Included in every annual clinic examination was a self-administered medical history questionnaire to update the status of specific diseases and to answer other health-related questions. During the follow-up clinic visit from July 1993 until June 1994, a series of questions was added to the medical history questionnaire to ascertain participants’ perceptions of access to health care. Questions included asking participants about the medical setting where care was usually sought, making an appointment versus walking in to the medical office when care was needed, ability to see the same doctor at each visit, how soon after needing care they were able to be seen, and whether they had a doctor or doctor’s assistant that could be reached by telephone for medical problems. In addition, participants were asked to record the level to which a series of 9 statements affected their ability to see a doctor in the past year. The statements included “not having a regular doctor,” “taking care of others (e.g., “caring for a spouse or grandchildren”), “ difficulty finding transportation,” “doctor/clinic/hospital bills,” “work responsibilities,” “fearful for safety on streets,” “fear that doctor will perform tests that I don’t need,” “fear that doctor will discover a serious illness,” and “doctor is not responsive to my concerns.” Individuals responded using a 5-point Likert scale with the following choices: “not at all,” “very little,” “moderate amount,” “very much,” “a whole lot,” and “don’t know.”
Participants either received the questionnaire by mail and returned it to the clinic during the examination or completed the form in the clinic. A clinic technician reviewed the questionnaire for completeness and inconsistencies during the visit so that mistakes could be corrected before the participant’s departure. Quality control procedures after data collection included statistical analyses for inconsistencies and identification of outliers. Data were verified by site staff when problems were found. Responses to the questions on access to health care are reported here.
Statistical Analyses
SPSS, Version 11, was used for analyses.24 Descriptive statistics were calculated for participants completing the questionnaires, and bivariate associations were evaluated using χ2 tests. A dichotomous measure of having problems with access to care was computed by a respondent’s having answered “moderate amount,” “very much,” or “a whole lot” to any of the 9 statements on barriers to seeing a doctor. Using this measure as the outcome variable, unconditional logistic regression was used to assess the associations with the following sociodemographic characteristics of participants: age (categorized into 5 levels), gender, income (4 categories), race (White vs non-White), education (4 levels), and insurance coverage complementary to Medicare (none, Medicaid, private, or other). Medicaid was combined with no insurance because both represented lower socioeconomic status and to increase the number in the category. Unadjusted models for each factor and a model containing all of the variables together to evaluate independent associations were completed. Odds ratios (ORs) and 95% confidence intervals (CIs) for all models were reported.
RESULTS
A total of 5367 CHS participants were living at the time of the 1993–1994 clinic examination. Of these, 4889 (91.1%) completed the medical history questionnaire, including the questions on access to care. Mean age of respondents was 76.0 years (SD = 5.4), 59.7% were female, and 16.8% were of non-White ethnic minority, primarily African American (Table 1 ▶). Less than 40% had an annual household income of over $25 000. Almost 71% had private insurance supplemental to Medicare, 9% had no additional insurance, and 5% used Medicaid. Forty-four percent were found to have hypertension (defined by medication use or blood pressure measurement), and almost 13% reported a history of diabetes.
TABLE 1—
Characteristics of 4889 CHS Participants Who Completed Questions on Access to Care at the 1993–1994 Annual Examination
| No. | % | |
| Total | 4889 | . . . |
| Age, y | ||
| < 72 | 1020 | 20.9 |
| 72–74 | 1296 | 26.5 |
| 75–79 | 1377 | 28.2 |
| 80–84 | 815 | 16.7 |
| ≥85 | 381 | 7.8 |
| Mean age, y (SD) | 76.0 (5.4) | |
| Gender | ||
| Female | 2917 | 59.7 |
| Male | 1972 | 40.3 |
| Race | ||
| White | 4066 | 83.2 |
| African American | 795 | 16.3 |
| Other a | 28 | 0.5 |
| Education | ||
| Less than high school | 1339 | 27.4 |
| High school graduate | 1370 | 28 |
| Some college | 1121 | 22.9 |
| ≥College graduate | 1046 | 21.4 |
| Unknown | 13 | 0.3 |
| Annual household income, $ | ||
| < 12 000 | 1188 | 24.3 |
| 12 000–24 999 | 1577 | 32.3 |
| 25 000–49 999 | 1181 | 24.2 |
| ≥50 000 | 637 | 13 |
| Unknown | 306 | 6.3 |
| Smoking status | ||
| Current | 439 | 9 |
| Former | 2183 | 44.6 |
| Never | 2220 | 45.4 |
| Unknown | 47 | 1 |
| Hypertension | ||
| Hypertensive | 2166 | 44.3 |
| Borderline | 585 | 11.6 |
| Normal | 1875 | 38.4 |
| Unknown | 283 | 5.8 |
| Diabetes (self-reported) | ||
| Has | 634 | 12.9 |
| Does not have | 4229 | 86.5 |
| Unknown | 26 | 0.5 |
| Supplemental insurance | ||
| None | 434 | 8.8 |
| Private | 3467 | 70.9 |
| Medicaid | 254 | 5.2 |
| Other | 669 | 13.7 |
| Unknown | 67 | 1.4 |
Note. CHS = Cardiovascular Health Study.
aIncludes 9 American Indian/Alaska Natives, 4 Asian/Pacific Islanders, and 5 participants of other racial/ethnic origin.
Bivariate associations between questions on care-seeking behavior or ability to receive services and sociodemographic characteristics are shown in Tables 2 ▶ and 3 ▶. Most respondents (87%) reported using a physician’s office for medical care, and less than 1% relied on an emergency department for regular care. Individuals who usually used a physician’s office for care were more likely to be younger, female, and White; to have supplemental insurance; and to have a higher income than those who received care in other settings. Persons of minority ethnicity were more likely to receive care in a health department clinic (4.9%) than were Whites (0.2% ).
TABLE 2—
Bivariate Associations Between Specific Aspects of Access and Sociodemographic Characteristics Among Participants in the Cardiovascular Health Study, 1993–1994
| Gender | Race | Supplemental Insurance | ||||||
| Male, No. (%) | Female, No. (%) | White, No. (%) | Non-White, No. (%) | Private, No. (%) | Other, No. (%) | None/Medicaid, No. (%) | Total, No. (%) | |
| Where do they go for medical care? | ** | ** | ** | |||||
| Doctor’s office | 1674 (84.9) | 2560 (87.8) | 3664 (90.1) | 570 (69.3) | 3059 (88.2) | 607 (90.7) | 526 (76.7) | 4234 (86.6) |
| Hospital clinic | 201 (10.2) | 166 (5.7) | 223 (5.5) | 144 (17.5) | 239 (6.9) | 34 (5.1) | 86 (12.5) | 367 (7.5) |
| Other clinic | 58 (2.9) | 114 (3.9) | 115 (2.8) | 57 (6.9) | 116 (3.3) | 18 (2.7) | 34 (5.0) | 172 (3.5) |
| Health department clinic | 12 (0.6) | 35 (1.2) | 7 (0.2) | 40 (4.9) | 18 (0.5) | 4 (0.6) | 22 (3.2) | 47 (1.0) |
| Emergency room | 12 (0.6) | 15 (0.5) | 20 (0.5) | 7 (0.9) | 14 (0.4) | 2 (0.3) | 9 (1.3) | 27 (0.6) |
| Physician home visit | 15 (0.8) | 27 (0.9) | 37 (0.9) | 5 (0.6) | 21 (0.6) | 4 (0.6) | 9 (1.3) | 42 (0.9) |
| How do they usually see the doctor? | * | ** | ** | |||||
| Make appointment | 1883 (96.1) | 2828 (97.7) | 3959 (98.0) | 752 (92.3) | 3364 (97.5) | 657 (98.5) | 634 (93.2) | 4711 (97.0) |
| Walk-in | 77 (3.9) | 67 (2.3) | 81 (2.0) | 63 (7.7) | 88 (2.5) | 10 (1.5) | 46 (6.8) | 144 (3.0) |
| How soon are they able to be seen? | ** | * | ||||||
| Same day | 830 (46.0) | 1153 (44.1) | 1591 (43.1) | 362 (54.1) | 1366 (42.9) | 279 (47.4) | 316 (52.5) | 1983 (44.9) |
| 1–3 d | 722 (40.0) | 1140 (43.6) | 1606 (43.5) | 256 (35.4) | 1393 (43.8) | 237 (40.3) | 218 (36.2) | 1862 (42.2) |
| 4–7 d | 154 (8.5) | 199 (7.6) | 305 (8.3) | 48 (6.6) | 267 (8.4) | 42 (7.1) | 40 (6.6) | 353 (8.0) |
| 1–2 wk | 71 (3.9) | 87 (3.3) | 138 (3.7) | 20 (2.8) | 110 ( 3.5) | 25 (4.3) | 19 (3.2) | 158 (3.6) |
| > 2 wk | 27 (1.5) | 33 (1.3) | 52 (1.4) | 8 (1.2) | 46 (1.4) | 5 (0.8) | 9 (1.5) | 60 (1.3) |
| Are they able to see the same doctor every time? | * | ** | * | |||||
| Yes | 1803 (92.4) | 2731 (94.2) | 3800 (94.1) | 734 (90.6) | 3245 (94.1) | 622 (93.4) | 611 (90.4) | 4532 (93.5) |
| No | 149 (7.6) | 167 (5.8) | 240 (5.9) | 76 (9.4) | 202 (5.9) | 44 (6.6) | 65 (9.6) | 316 (6.5) |
| Do they have a doctor they can talk to by telephone? | ** | ** | ||||||
| Yes | 1632 (87.3) | 2447 (88.1) | 3434 (88.8) | 645 (82.4) | 2942 (89.0) | 577 (90.0) | 517 (79.3) | 4079 (87.8) |
| No | 332 (11.9) | 431 (11.2) | 138 (17.6) | 365 (11.0) | 58 (9.1) | 135 (20.7) | 569 (12.2) | 237 (12.7) |
*P < .01 for χ2 tests of the 2 categorical variables; **P < .001 for χ2 tests of the 2 categorical variables.
TABLE 3—
Bivariate Associations Between Specific Aspects of Access and Sociodemographic Characteristics Among Participants in the Cardiovascular Health Study, 1993–1994
| Income | Age Category | |||||||
| < $12 000, No. (%) | $12 000– $24 999, No. (%) | $25 000–$49 999, No. (%) | ≥$50 000, No. (%) | < 75 y, No. (%) | 75–79 y, No. (%) | ≥85 y, No. (%) | Total, No. (%) | |
| Where do they go for medical care? | * | * | ||||||
| Doctor’s office | 967 (81.4) | 1385 (87.8) | 1041 (88.2) | 575 (90.3) | 1996 (86.2) | 1208 (87.7) | 1030 (86.1) | 4234 (86.6) |
| Hospital clinic | 84 (7.1) | 122 (7.7) | 92 (7.8) | 39 (6.1) | 190 (8.2) | 102 (7.4) | 75 (6.3) | 367 (7.5) |
| Other clinic | 69 (5.8) | 42 (2.7) | 35 (3.0) | 18 (2.8) | 102 (4.4) | 30 (2.2) | 40 (3.3) | 172 (3.5) |
| Health department clinic | 36 (3.0) | 8 (0.5) | 3 (0.3) | 0 (0.0) | 12 (0.5) | 23 (1.7) | 12 (1.0) | 47 (1.0) |
| Emergency room | 14 (1.2) | 10 (0.6) | 2 (0.2) | 1 (0.2) | 11 (0.5) | 8 (0.6) | 8 (0.7) | 27 (0.6) |
| Physician home visit | 18 (1.5) | 10 (0.6) | 7 (0.6) | 4 (0.6) | 5 (0.2) | 6 (0.4) | 31 (2.6) | 42 (0.9) |
| How do they usually see the doctor? | * | |||||||
| Make appointment | 1113 (95.1) | 1518 (96.9) | 1151 (97.7) | 628 (98.7) | 2239 (96.9) | 1329 (97.1) | 1143 (97.2) | 4711 (97.0) |
| Walk-in | 57 (4.9) | 48 (3.1) | 27 (2.3) | 8 (1.3) | 72 (3.1) | 39 (2.9) | 33 (2.8) | 144 (3.0) |
| How soon are they able to be seen? | * | |||||||
| Same day | 521 (50.7) | 625 (43.5) | 470 (43.1) | 247 (21.1) | 930 (43.7) | 560 (45.2) | 493 (46.9) | 1983 (44.9) |
| 1–3 d | 393 (38.3) | 637 (44.3) | 466 (42.8) | 253 (43.1) | 934 (43.9) | 504 (40.7) | 424 (40.3) | 1862 (42.2) |
| 4–7 d | 70 (6.8) | 127 (8.8) | 89 (8.2) | 49 (8.3) | 172 (8.1) | 97 (7.8) | 84 (8.0) | 353 (8.0) |
| 1–2 wk | 31 (3.0) | 35 (2.4) | 48 (4.4) | 29 (4.9) | 64 (3.0) | 59 (4.8) | 35 (3.3) | 158 (3.6) |
| > 2 wk | 12 (1.2) | 14 (1.0) | 17 (1.6) | 9 (1.5) | 27 (1.2) | 18 (1.4) | 15 (1.4) | 60 (1.3) |
| Are they able to see the same doctor every time? | ||||||||
| Yes | 1082 (92.2) | 1469 (93.7) | 1105 (94.1) | 594 (94.1) | 2128 (92.6) | 1290 (94.4) | 1116 (94.3) | 4532 (93.5) |
| No | 21 (6.9) | 98 (6.3) | 69 (5.9) | 37 (5.9) | 171 (7.4) | 77 (5.6) | 68 (5.7) | 316 (6.5) |
| Do they have a doctor they can talk to by telephone? | * | |||||||
| Yes | 921 (82.5) | 1347 (89.6 | 975 (87.2) | 568 (91.9) | 1915 (87.0) | 1172 (89.1) | 992 (87.6) | 4079 (87.8) |
| No | 196 (17.5) | 157 (10.4) | 143 (12.8) | 50 (8.1) | 285 (13.0) | 143 (10.9) | 141 (12.4) | 569 (12.2) |
*P < .001 for χ2 tests of the 2 categorical variables.
Overall, only 3% sought “walk-in” care rather than scheduling an appointment. Walk-in care was used more frequently by minority participants and persons without supplemental insurance or at lower incomes and most likely reflects use of health department clinics. Almost 45% were able to make a same-day appointment; appointments within 3 days were made by over 87% of respondents. Although gender and age were not associated with how soon a patient could be seen, differences by race (minorities were more likely to obtain a same-day appointment), income (low-income patients were more likely to obtain a same-day appointment), and insurance coverage (those with coverage were less likely to obtain a same-day appointment) were found. Most participants (93%) regularly saw the same physician for care. Female gender, White race, and insurance coverage were associated with the ability to see the same doctor, although absolute differences were small. Over 87% had a doctor they could talk to on the telephone. Minorities and persons with lower income or without supplemental insurance were less likely to have access to a physician by telephone.
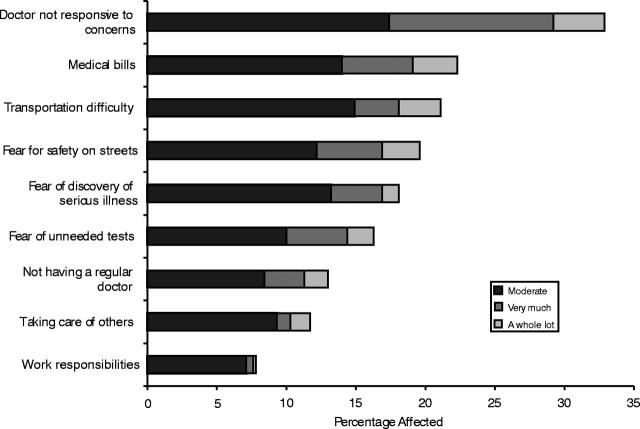
Overall, 4855 persons (99% of participants completing a clinic visit) answered a minimum of 1 of the 9 questions on barriers to health care. Of these, 592 (12.2%) reported having at least 1 barrier that affected their ability to see a doctor either a “moderate amount,” “very much,” or “a whole lot.” The Cronbach coefficient α, reflecting internal consistency among the 9 barriers, was calculated as .7. No more than 4% of respondents were affected by any 1 of the 9 barriers listed in the questionnaire. Of those reporting at least 1 barrier (Figure 1 ▶), the most common barrier reported was the doctors’ lack of responsiveness to concerns, cited by almost one third of respondents (32.9%). Other important barriers included medical bills (22.3%), transportation problems (21.1%), street safety (19.6%), fear of discovering a serious illness (18.1%), and fear of unneeded tests (16.3%). Fewer than 15% responded that they were affected by not having a regular doctor (13.0%), taking care of others (11.7%), and work responsibilities (7.8%). Individuals of minority race were more likely to be affected by medical bills, transportation difficulties, street safety, and fear of a serious illness (χ2 P < .05) than Whites; however, these bivariate associations do not take into consideration socioeconomic factors such as income or supplemental insurance.
FIGURE 1—
Distribution of self-reported responses to the question “How much did each of the following affect your ability to see a doctor in the past year?” from 592 participants in the Cardiovascular Health Study affected by at least 1 barrier.
Results of the unadjusted logistic regression model to assess determinants of access problems showed that older age, female gender, non-White race, lower income, and lack of complementary insurance were all significantly related to a self-perception of problems with access to care (Table 4 ▶). Education was also investigated, and the unadjusted risk for less than a high school degree resulted in an OR of 1.6 (95% CI = 1.2–2.0) compared with college graduates. Education, however, was not included in the adjusted model, as extremely high correlations with the other sociodemographic variables resulted in overadjustment. In the adjusted model evaluating independent associations of the other 4 sociodemographic characteristics, all income categories below $50 000 per year were associated with perceived barriers to care.
TABLE 4—
Independent Determinants of Access Problems Using Multiple Logistic Regression Unadjusted and Adjusted for Age, Race, Gender, Income, and Supplemental Insurance Among Participants in the Cardiovascular Health Study, 1993–1994
| Risk Factor | No. | Subjects | Unadjusted OR (95% CI) | P | Adjusted OR (95% CI)a | P |
| Age, y | ||||||
| < 72 | 1018 | 132 | 1.0b | 0.003 | 1.0b | 0.03 |
| 72–74 | 1290 | 146 | 0.9 (0.7, 1.1) | 0.9 (0.7, 1.2) | ||
| 75–79 | 1367 | 143 | 0.8 (0.6, 1.0) | 0.8 (0.6, 1.1) | ||
| 80–84 | 805 | 105 | 1.0 (0.8, 1.3) | 1.0 (0.7, 1.3) | ||
| ≥85 | 375 | 66 | 1.4 (1.0, 2.0) | 1.4 (1.0, 2.0) | ||
| Gender | ||||||
| Male | 1956 | 202 | 1.0b | 0.001 | 1.0b | 0.05 |
| Female | 2899 | 390 | 1.4 (1.1, 1.6) | 1.2 (1.0, 1.5) | ||
| Race | ||||||
| White | 4040 | 454 | 1.0b | < .001 | 1.0b | 0.14 |
| Non-White | 815 | 138 | 1.6 (1.3, 2.0) | 1.2 (0.9, 1.5) | ||
| Income | ||||||
| ≥$50 000 | 635 | 42 | 1.0b | < .001 | 1.0b | < .001 |
| $25 000–49 999 | 1178 | 107 | 1.4 (1.0, 2.0) | 1.4 (1.0, 2.0) | ||
| $12 000–24 999 | 1564 | 195 | 2.0 (1.4, 2.8) | 1.9 (1.4, 2.7) | ||
| < $12 000 | 1173 | 214 | 3.2 (2.2, 4.5) | 2.6 (1.8, 3.7) | ||
| Supplemental insurance | ||||||
| Private | 3455 | 397 | 1.0b | < .001 | 1.0b | 0.006 |
| Other | 664 | 62 | 0.8 (0.6, 1.1) | 0.8 (0.6, 1.0) | ||
| None/Medicaid | 682 | 126 | 1.7 (1.4, 2.2) | 1.3 (1.0, 1.7) | ||
Note. OR = odds ratio; CI = confidence interval. aAdjusted for all variables shown in the table. breference value.
Participants earning less than $12 000 annually were 2.6 times (95% CI = 1.8–3.7) more likely to report a barrier to seeing a doctor than those earning $50 000 or more. Individuals with no supplemental insurance or Medicaid (OR = 1.3, 95% CI = 1.0–1.7), individuals older than 85 years (OR = 1.4, 95% CI = 1.0–2.0), and women (OR = 1.2, 95% CI = 1.0–1.5) were also more likely to report barriers to care after adjustment for the other characteristics. Although an association between minority race and barriers to care was found in the unadjusted model (OR = 1.6, 95% CI = 1.3–2.0), adjustment attenuated the association (OR = 1.2, 95% CI = 0.9–1.5). A model in which age was included as a continuous variable produced similar results. No interactions between race and age, gender, income, or supplemental insurance were found.
DISCUSSION
The data collected in the CHS evaluating access and barriers to health care in Medicare recipients provide new insights into behaviors and perceptions of the elderly regarding their ability to obtain care. Although most participants routinely sought medical care at a physician’s office or clinic, minorities used health department/government-sponsored clinics and the emergency room more. Most respondents were able to make an appointment to see a doctor within a few days, and most had a doctor they could reach by telephone to discuss medical conditions. Over 90% were able to see the same doctor on multiple visits. The problem cited most often that affected one’s ability to see a doctor was the doctor’s lack of responsiveness to concerns rather than physical barriers such as cost or transportation. Age, gender, income, and insurance coverage were related individually and independently to perceptions of access problems when controlled for race and each other. Race was no longer associated with perceived barriers to access after adjustment for age, gender, income, and insurance. Although it is well known that sociodemographic variables such as these are highly correlated within most populations, these data suggest that poverty rather than race may be the underlying factor influencing access to health care for the elderly.
A number of studies have reported racial disparities in the use of medical services among Medicare beneficiaries.12,13,25–28 Most of these studies have found independent associations between access and other socioeconomic factors such as health insurance and income. Large databases, such as those compiled by insurance providers and the government, are often used to assess these issues. Differences according to race were found in the quality of clinical care received by enrollees in managed care organizations as assessed by standardized measures of use.10 In this study by Schneider et al.,10 race was independently associated with reduced quality of care in 4 clinical outcomes after adjusting for age, sex, Medicaid insurance, income, education, and rural residence. Income, education, and rural residence were estimated using information available by zip code. Likewise, it has been reported that racial differences persisted in the use of medical procedures and tests among Medicare beneficiaries not fully accounted for by financial barriers.15 This study used Medicare claims data, which did not include information regarding income or education.
Psychological Barriers to Care
The most difficult aspect of assessing race in studies such as these, which use Medicare claims data or other large provider databases, is the inability to control for other socioeconomic factors. In these types of studies, income, education, and rural residence are typically not available on each individual, and subsequently these factors are estimated by using zip code or other methods. In the CHS, self-reported income was known for each participant and provided greater control in the analyses. We found that income was the most important factor related to problems of self-perceived access, although insurance coverage, age, and gender remained independently related. In the Women’s Health Initiative, racial differences disappeared, whereas insurance and perceived health were independently related to fewer provider visits in the previous year.14 These and our results suggest that with adequate information on other socioeconomic factors, the association between race and access may be attenuated.
The results of this study may shed light on consequences of different proposals currently being considered for Medicare reform. These data show that income is a strong predictor of access to health care in the elderly, independent of race. Should reform result in more out-of-pocket expenses, it will surely decrease an older person’s ability to be treated by a physician. It follows that rather than saving money, such a system would incur far greater expenses, as untreated conditions and lack of prevention would lead to greater severity of disease, which would promote more emergency visits and longer hospital stays.
It is intriguing that in this study an elderly person’s perception of the physician’s lack of responsiveness was a greater disincentive to seeking care than more tangible barriers. Other studies have found that barriers to care such as cost, transportation, lack of information, and caring for others prevent individuals from obtaining health care.13,29 However, data on patients’ perceptions as an underlying cause of racial disparity are limited. One study found that racial and ethnic minority groups had less positive perceptions of their physicians in terms of both style (e.g., listening skills, ability to explain) and trust (e.g., placed patient’s needs above others, referred the patient when needed)30; issues of trust within racial minorities have been documented in other studies.31 A qualitative study of angina found that patients felt physicians were busy and that patients did not like to bother them with their own conditions.32 Lack of satisfaction has also been found to be associated with more symptoms and lower medication compliance in patients,18 whereas greater satisfaction has been associated with better outcomes.19 As physicians are forced to spend less time with their patients because of financial and other managerial constraints, it is not surprising that patients will be affected. Interpretation of our data suggests that the psychological impact of perceptions of care may later translate into barriers for seeking future health care.
The CHS provides a great resource for examining issues related to health care in the elderly. Strengths of this study include the large sample size, even at visits years after baseline. Retention of participants has been excellent and was calculated at over 94% of those alive at the 1993–1994 annual examination. All data were meticulously collected using standardized methods across sites; quality control procedures increased the accuracy of data. As enrollees were primarily selected randomly from Medicare files, generalizability of results may also be high.
Study Limitations
There are limitations to this study. In these analyses, the outcome variable was constructed from 9 separate responses concerning barriers to access to create a global measure and to increase power for analyses. It should be noted that the results found for this global access measure may be different than associations found for the individual barriers or combinations of them. The cross-sectional nature of these analyses prevents consideration of previous or future behaviors of participants. As these data were collected in 1993–1994, they may not accurately reflect current health care access issues. However, the deterioration of the US economy since then may lead us to surmise that economic barriers would have a more important impact on access to care now than what is reflected in this study. In addition, similar to many volunteer cohorts, participants in the CHS tended to be healthier and better educated than those who declined to be a part of the cohort.21 Although the data collected here were gathered at the fifth follow-up visit for most of the participants, some of the “healthy cohort” effect may still have remained at that time. In addition, our cohort would contain fewer of the persons most at risk for access problems compared with the general population (i.e., the poor and uninsured). However, a special effort to recruit additional African Americans into the study during the third year of the CHS ensured that associations pertaining to race could be adequately assessed.
Analyses of issues related to health care in the CHS have led to several conclusions. First, these data confirm that certain groups of the elderly American population, although not a large proportion, may have problems with access to medical care and treatment even though they possess Medicare insurance. Persons at greatest risk of confronting barriers are those with the lowest income, those in the oldest age group, females, the less educated, and those lacking insurance beyond Medicare. Racial disparities may play less of a role in health care access when these other factors are carefully controlled. Finally, our data suggest that access to care may be affected by more than socioeconomic factors such as income and age. Perceptions of physicians’ attitudes toward a patient’s health and personal needs, as perhaps measured by time spent with a patient and level of response to concerns, may also act as a barrier to obtaining necessary treatment and preventive care. Although Medicare data are extremely valuable in health utilization studies, care must be taken when making conclusions regarding independent associations of data not collected at the individual level. Future studies should consider careful ascertainment of socioeconomic variables along with perceptions of care and other psychological factors when evaluating access to health care in the elderly. Determination of associations between perceptions of barriers and actual access to care based on use is also needed to more clearly understand this issue.
Acknowledgments
The research reported in this article was supported by contracts N01-HC-85079 through N01-HC-85086, N01-HC-35129, and N01 HC-15103 from the National Heart, Lung, and Blood Institute.
A full list of participating CHS investigators and institutions can be found at http://www.chs-nhlbi.org. Participating CHS investigators and institutions include Steering Committee Chairman Curt D. Furberg, MD, PhD, Wake Forest University School of Medicine; Jean Olson, MD, MPH, National Heart, Lung, and Blood Institute Project Office; Gregory L. Burke, MD, Wake Forest University School of Medicine; Pentti M. Rautaharju, MD, PhD, Wake Forest University, Echocardiography Reading Center; John Robbins, MD, MHS, University of California–Davis; Linda P. Fried, MD, MPH, Johns Hopkins University; Nick Bryan, MD, PhD; Norman J. Beauchamp, MD, Johns Hopkins University, Magnetic Resonance Imaging Reading Center; Lewis H. Kuller, MD, DrPH, University of Pittsburgh; Julius M. Gardin, MD, University of California–Irvine, Echocardiography Reading Center (baseline); John S. Gottdiener, MD, Georgetown Medical Center, Echocardiography Reading Center (follow-up); Daniel H. O’Leary, MD, New England Medical Center, Boston, Ultrasound Reading Center; Russell P. Tracy, PhD, University of Vermont, Central Blood Analysis Laboratory; Paul Enright, MD, University of Arizona, Tucson, Pulmonary Reading Center; Ronald Klein, MD, University of Wisconsin, Retinal Reading Center; Richard A. Kronmal, PhD, University of Washington, Coordinating Center.
Contributors A. L. Fitzpatrick led the analysis and drafted the article. N. R. Powe conceived the idea and developed the questions administered in the study. N. R. Powe, L. S. Cooper, D. G. Ives, and J.A. Robbins participated in the analyses and modification of the article. N. R. Powe, D. G. Ives, and J. A. Robbins were also involved in data collection in managerial roles at the CHS field centers.
Human Participation Protection Human subjects approval was received from the institutional review boards at all participating institutions of the Cardiovascular Health Study including the University of Washington, Johns Hopkins University, University of Pittsburgh, University of California–Davis, and Wake Forest University.
Peer Reviewed
References
- 1.McCormick MC, Weinick RM, Elixhauser A, Stagnitti MN, Thompson J, Simpson I. Annual report on access to and utilization of health care for children and youth in the United States–2000. Ambul Pediatr. 2001;1:3–15. [DOI] [PubMed] [Google Scholar]
- 2.Reed MC, Tu HT. Triple jeopardy: low income, chronically ill and uninsured in America. Issue Brief Cent Stud Health Syst Change. 2002;49:1–4. [PubMed] [Google Scholar]
- 3.Broyles RW, Narine L, Brandt EN Jr. The temporarily and chronically uninsured: does their use of primary care differ? J Health Care Poor Underserved. 2002;13:95–111. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham PJ. Declining employer-sponsored coverage: the role of public programs and implications for access to care. Med Care Res Rev. 2002;59:79–98. [DOI] [PubMed] [Google Scholar]
- 5.Guyer J, Broaddus M, Dude A. Millions of mothers lack health insurance coverage in the United States: most uninsured mothers lack access both to employer-based coverage and to publicly subsidized health insurance. Int J Health Serv. 2002;32:89–106. [DOI] [PubMed] [Google Scholar]
- 6.Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 2001 Current Population Survey. EBRI Issue Brief. 2001;240:1–31. [PubMed] [Google Scholar]
- 7.Keruly JC, Conviser R, Moore RD. Association of medical insurance and other factors with receipt of anti-retroviral therapy. Am J Public Health. 2002;92:852–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruiz P. Hispanic access to health/mental health services. Psychiatr Q. 2002;73:85–91. [DOI] [PubMed] [Google Scholar]
- 9.Strzelczyk JJ, Dignan MB. Disparities in adherence to recommended followup on screening mammography: interaction of sociodemographic factors. Ethn Dis. 2002;12:77–86. [PubMed] [Google Scholar]
- 10.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA. 2002;287:1288–1294. [DOI] [PubMed] [Google Scholar]
- 11.Porell FW, Miltiades HB. Access to care and functional status change among aged Medicare beneficiaries. J Gerontol B Psychol Sci Soc Sci. 2001;56:S69–S83. [DOI] [PubMed] [Google Scholar]
- 12.Gornick ME. The association of race/socioeconomic status and use of Medicare services: a little-known failure in access to care. Ann N Y Acad Sci. 1999;896: 497–500. [DOI] [PubMed] [Google Scholar]
- 13.Janes GR, Blackman DK, Bolen JC, et al. Surveillance for use of preventive health-care services by older adults, 1995–1997. MMWR CDC Surveill Summ. 1999;48:51–88. [PubMed] [Google Scholar]
- 14.Hsia J, Kemper E, Sofaer S, et al. Is insurance a more important determinant of healthcare access than perceived health? Evidence from the Women’s Health Initiative. J Womens Health Gend Based Med. 2000;9: 881–889. [DOI] [PubMed] [Google Scholar]
- 15.Escarce JJ, Epstein KR, Colby DC, Schwartz JS. Racial differences in the elderly’s use of medical procedures and diagnostic tests. Am J Public Health. 1993; 83:948–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akinci F, Sinay T. Perceived access in a managed care environment: determinants of satisfaction. Health Serv Manage Res. 2003;16:85–95. [DOI] [PubMed] [Google Scholar]
- 17.Meng YY, Jatulis DE, McDonald JP, Legorreta AP. Satisfaction with access to and quality of health care among Medicare enrollees in a health maintenance organization. West J Med. 1997;166:242–247. [PMC free article] [PubMed] [Google Scholar]
- 18.Harris LE, Luft FC, Rudy DW, Tierney WM. Correlates of health care satisfaction in inner-city patients with hypertension and chronic renal insufficiency. Soc Sci Med. 1995;41:1639–1645. [DOI] [PubMed] [Google Scholar]
- 19.Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in Type 2 diabetes mellitus. Diabet Med. 2003;20:486–490. [DOI] [PubMed] [Google Scholar]
- 20.Fried LP, Borhani NO, Enright PE, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. [DOI] [PubMed] [Google Scholar]
- 21.Tell GS, Fried LP, Hermanson B, et al. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993; 3:358–366. [DOI] [PubMed] [Google Scholar]
- 22.Psaty BM, Kuller LH, Bild D, et al. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–277. [DOI] [PubMed] [Google Scholar]
- 23.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events: the Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285. [DOI] [PubMed] [Google Scholar]
- 24.Norusis MJ, SPSS Inc. SPSS for Windows, Advanced Statistics, Release 11.0. Chicago, IL: SPSS Inc; 2002.
- 25.Lurie N, Zhan C, Sangl J, Bierman AS, Sekscenski ES. Variation in racial and ethnic differences in consumer assessments of health care. Am J Manag Care. 2003;9: 502–509. [PubMed] [Google Scholar]
- 26.Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996; 335:791–799. [DOI] [PubMed] [Google Scholar]
- 27.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269:2642–2646. [PubMed] [Google Scholar]
- 28.Roetzheim RG, Pal N, Tennant C, et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999;91:1409–1415. [DOI] [PubMed] [Google Scholar]
- 29.Ahmed SM, Lemkau JP, Nealeigh N, Mann B. Barriers to healthcare access in a non-elderly urban poor American population. Health Soc Care Community. 2001;9:445–453. [DOI] [PubMed] [Google Scholar]
- 30.Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perception of physician style and trust. Arch Fam Med. 2000;9:1156–1163. [DOI] [PubMed] [Google Scholar]
- 31.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118:358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gardner K, Chapple A. Barriers to referral in patients with angina: qualitative study. BMJ 1999;319: 418–421. [DOI] [PMC free article] [PubMed] [Google Scholar]