Abstract
In this cross-sectional study of US military combat veterans, we assessed the helpfulness of different media for providing health risk communication messages. We have provided preliminary results from a postal survey of 5000 veterans sampled because of their deployment to Vietnam, the Persian Gulf, or Bosnia–Kosovo. Respondents endorsed the primary care provider as the most helpful source of health information. Access to the Internet and use of this medium for seeking health information differed by race, age, and cohort.
Military personnel deployed to war zones face a variety of physical, environmental, and psychological exposures.1,2 Concern about health consequences related to exposures may lead veterans to visit health care providers for treatment and health risk education.3,4 Risk communication regarding potential health outcomes is a fundamental task in the successful treatment of combat veterans.5–7 We have provided preliminary findings from a population-based survey of health concerns and preferred sources for health risk communication among combat veterans.
METHODS
Design
This cross-sectional, 206-item postal survey sampled 5000 veterans from the Vietnam War (1964–1973), the Persian Gulf War (1991), and the Bosnia–Kosovo peace-keeping activity (1995–2002). Approximately equal numbers of veterans from the Vietnam War, the Persian Gulf War, and the Bosnia–Kosovo peacekeeping activity were selected from Department of Defense personnel rosters. Initial findings from the first of 3 survey mailings have been reported here.
Measures
We asked participants to rate the helpfulness of different media for obtaining health information on a 10-point scale and to answer items regarding access to and use of the Internet.
Data Analysis
Mean scores for helpfulness ratings were computed and tested to assess differences by race for each communication mode. Proportions that had access to the Internet and used it to find health information were reported by conflict and race. Differences in Internet access by race were tested with the Pearson χ2 statistic. Trends for Internet use by age and conflict were tested with regression analysis and the Cochran–Armitage trend test, respectively.8
RESULTS
Subjects
The overall response rate for the first wave of surveys (N = 1432, 29%) showed variation by conflict, with the highest response rate from Vietnam veterans (n = 740, 45% of Vietnam sample), followed by veterans from the Persian Gulf War (n = 462, 28% of the Persian Gulf sample) and the Bosnia–Kosovo peacekeeping activity (n = 230, 14% of the Bosnia–Kosovo sample). A small group of respondents served in more than 1 conflict (n = 109).
The respondents were predominantly White (80% overall), which was comparable to the sample distribution (77% overall). Black veterans represented 17% of the sample but only 10% of respondents. The mean age of Vietnam veterans was 60.4 years, of Persian Gulf War veterans was 45.6 years, and of Bosnia–Kosovo peacekeeping activity veterans was 41.7 years.
Helpfulness of Health Information Sources
When participants rated the helpfulness of health information sources, “own doctor” received the highest mean scores overall and across conflict and race subgroups (Table 1 ▶). In contrast, “VA doctor” received the lowest score for helpfulness overall, with significant differences observed by race and cohort. Non-White respondents assigned higher scores than did Whites for the helpfulness of “VA doctor” across all categories, with significant findings for all conflicts combined (P = .008) and Persian Gulf War veterans (P = .05).
TABLE 1—
Helpfulness Ratingsaof Different Modalities for Receiving Health Risk Information, by Race and Conflict: Mean Scores (SD)
| All Conflicts | Vietnam | Persian Gulf | Bosnia–Kosovo | ||||||||||
| Information Source | Total (N = 1288) | White (n = 1034) | Non-White (n = 254) | P | White (n = 662) | Non-White (n = 109) | P | White (n = 405) | Non-White (n = 148) | P | White (n = 158) | Non-White (n = 67) | P |
| Own doctor | 7.2 (2.8) | 7.3 (2.7) | 6.8 (3.0) | .1 | 7.3 (2.8) | 7.2 (3.1) | .73 | 7.0 (2.6) | 6.4 (3.1) | .11 | 7.5 (2.5) | 6.7 (3.0) | .11 |
| Pamphlet or brochure | 6.6 (2.7) | 6.6 (2.7) | 6.7 (2.6) | .58 | 6.6 (2.8) | 6.8 (2.7) | .76 | 6.5 (2.6) | 6.7 (2.6) | .49 | 6.3 (2.6) | 6.8 (2.6) | .24 |
| VA newsletterb | 6.5 (2.9) | 6.5 (2.9) | 6.5 (2.8) | .97 | 6.5 (3.0) | 6.6 (2.9) | .99 | 6.6 (2.7) | 6.4 (2.8) | .58 | 5.7 (2.9) | 6.5 (2.8) | .09 |
| VSO newsletterc | 6.1 (3.0) | 6.0 (3.0) | 6.4 (2.9) | .04 | 6.0 (3.1) | 6.8 (2.9) | .02 | 6.2 (2.8) | 6.4 (2.9) | .47 | 5.5 (2.8) | 6.1 (3.1) | .18 |
| Web site | 6.0 (3.1) | 5.9 (3.0) | 6.3 (3.0) | .06 | 5.6 (3.1) | 5.7 (3.3) | .66 | 6.3 (2.9) | 6.1 (3.0) | .73 | 6.2 (2.9) | 6.9 (2.9) | .08 |
| Television | 5.7 (2.8) | 5.6 (2.7) | 6.1 (2.8) | .002 | 5.6 (2.8) | 5.9 (2.9) | .27 | 5.5 (2.6) | 6.1 (2.9) | .01 | 5.5 (2.8) | 6.5 (2.6) | .03 |
| Newspaper article | 5.6 (2.7) | 5.6 (2.7) | 5.8 (2.8) | .15 | 5.7 (2.7) | 5.8 (2.9) | .71 | 5.4 (2.5) | 5.6 (2.9) | .27 | 5.4 (2.8) | 6.1 (2.7) | .09 |
| VA doctor | 5.5 (3.2) | 5.4 (3.2) | 5.9 (3.2) | .008 | 5.2 (3.2) | 5.8 (3.4) | .12 | 5.4 (3.0) | 6.0 (3.1) | .05 | 5.5 (3.3) | 5.8 (3.1) | .55 |
Note. Kruskal–Wallis test used to compare distributions of scores for Whites and non-Whites. P for χ2 statistic shown. Missing responses for helpfulness ratings ranged from 5% to 32%; Vietnam veterans, 12%–32%; Persian Gulf War veterans, 5%–14%; and Bosnia–Kosovo peacekeeping activity veterans, 5%–12%.
a Range: 1 = not very helpful; 10 = very helpful.
b VA newsletter = official publication of the Department of Veterans Affairs (VA).
c VSO newsletter = publication of a congressionally accredited Veterans Service Organization.
Pamphlets or brochures and Department of Veterans Affairs (VA) newsletters were given the second and third most favorable mean scores for helpfulness (6.6 and 6.5, respectively). Newsletters from Veterans Service Organizations were considered more helpful by non-White Vietnam veterans (P = .02) and by non-Whites for the 3 cohorts combined (P = .04). Television received a low mean score (5.7) relative to other modes for receiving health information but showed a statistically significant difference by race, with a preference expressed by non-White respondents from the Persian Gulf War (P = .01), from Bosnia–Kosovo (P = .03), and overall (P = .002). Regression analyses found that decreasing age strongly predicted higher ratings for the helpfulness of Web sites as a source of health information (β = −0.045/ year; P < .001; R2 = 0.03).
Internet Access
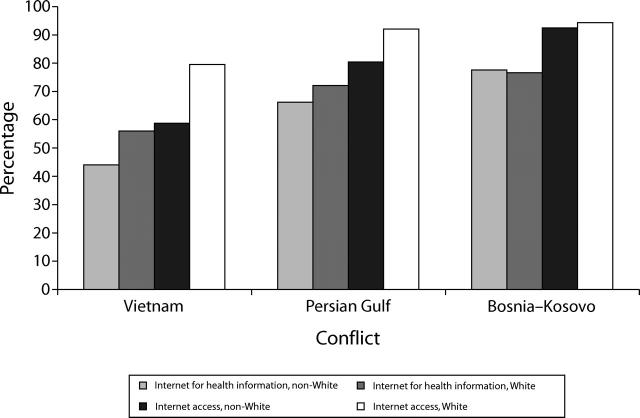
Access to the Internet and use of this medium for obtaining health information have been increasing with successive cohorts (Cochran–Armitage trend test, P < .001; Figure 1 ▶). Differences in access to the Inter-net for Whites and non-Whites were largest for Vietnam veterans (nearly 20%, P< .001) and narrowed over time (12% for the Persian Gulf War veterans, P< .001; and 2% for Bosnia–Kosovo veterans, P= .62).
FIGURE 1—
Percentage of combat veterans from Vietnam War, Persian Gulf War, and Bosnia–Kosovo conflicts who have any access to the Internet and who use the Internet to obtain health information, by race.
DISCUSSION
These preliminary findings indicated high Internet use among veterans, suggesting that the Internet offers an important channel for delivering health risk information to combat veterans. Internet access among Vietnam veterans (77%; 50–87 years old) was higher than that among the general US population (62% of 50- to 58-year-olds, 46% of 59- to 68-year-olds).9 Greater familiarity with the Internet among younger cohorts of veterans makes this medium an especially important tool for risk communication messages. Also, non-Whites rated a variety of media more favorably than did Whites, suggesting greater receptivity to a wider array of information sources.
These findings reinforce the role of the primary health care provider as the most helpful resource for health risk communication. For VA health care providers, having access to knowledge resources and supporting materials related to postdeployment health is critical. Recognizing this need, the VA recently created the War Related Illness and Injury Study Centers, with an expressed purpose of addressing the health risk communication needs of combat veterans. These results will help to form the basis of future postdeployment health risk communication activities in the VA.
Acknowledgments
The Department of Veterans Affairs, War Related Illness and Injury Study Center, Washington, DC, supported this study.
We acknowledge the data management expertise of Marina Dobrovitsky, MA.
Human Participant Protection This study was approved by the institutional review board of the Department of Veterans Affairs Medical Center, Washington, DC.
Note.The opinions expressed by this brief are not necessarily those of the Department of Veterans Affairs.
Contributors A. I. Schneiderman assisted in originating the study, drafted the brief, and conducted the data analysis and interpretation. A. E. Lincoln assisted in the data analysis and interpretation and in the editing of the brief. B. Curbow assisted in originating the study, interpreting the analysis, and editing the brief. H. K. Kang assisted in originating the study and editing the brief.
Peer Reviewed
References
- 1.Hyams KC, Wignall FS, Roswell R. War syndromes and their evaluation: from the US Civil War to the Persian Gulf War. Ann Intern Med. 1996;125: 398–405. [DOI] [PubMed] [Google Scholar]
- 2.A National Obligation: Planning for Health Preparedness and Readjustment of the Military, Veterans, and Their Families After Future Deployments. Washington, DC: National Science and Technology Council, Executive Office of the President; 1998.
- 3.National Research Council. Improving Risk Communication. Washington, DC: National Academy Press; 1989.
- 4.Institute of Medicine. Prevention measures for deployed forces. In: Joellenbeck LM, Russell PK, Guze SB, eds. Strategies to Protect the Health of Deployed U.S. Forces: Medical Surveillance, Record Keeping, and Risk Reduction. Washington, DC: National Academy Press; 2000:92–120. [PubMed]
- 5.Engel CC. Clinical risk communication: explaining causality to Gulf War veterans with chronic multisymptom illnesses. Washington, DC: Dept of Defense; 1999. Available at: http://www.pdhealth.mil/clinicians/downloads/risk_comm.doc. Accessed March 30, 2004.
- 6.Lundgren R, McMakin A. Risk Communication. Columbus, Ohio: Batelle Press; 1998.
- 7.DOD/VHA clinical practice guideline for post-deployment health evaluation and management. Washington, DC: Department of Defense (DoD) and Department of Veterans Health Affairs (VHA); 2000 [Updated December 2001]. Available at: http://www.oqp.med.va.gov/cpg/PDH/PDH_Gol.htm. Accessed March 30, 2004.
- 8.Stokes ME, Davis CS, Koch GG. Categorical Data Analysis Using the SAS System. 2nd ed. New York, NY: John Wiley & Sons Inc; 2001.
- 9.Fox S. Older Americans and the Internet. Washington, DC: Pew Internet and American Life Project; 2004. Available at: http://www.pewinternet.org/reports/pdfs/PIP_Seniors_Online_2004.pdf. Accessed March 30, 2004.