Abstract
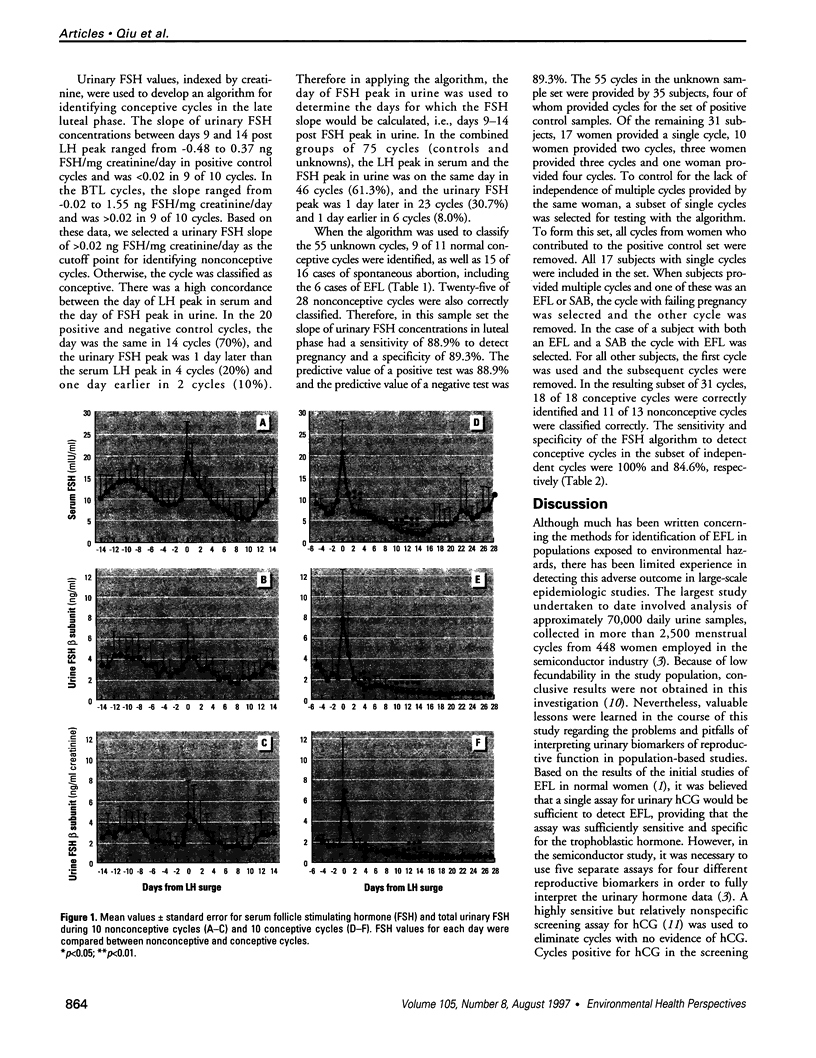
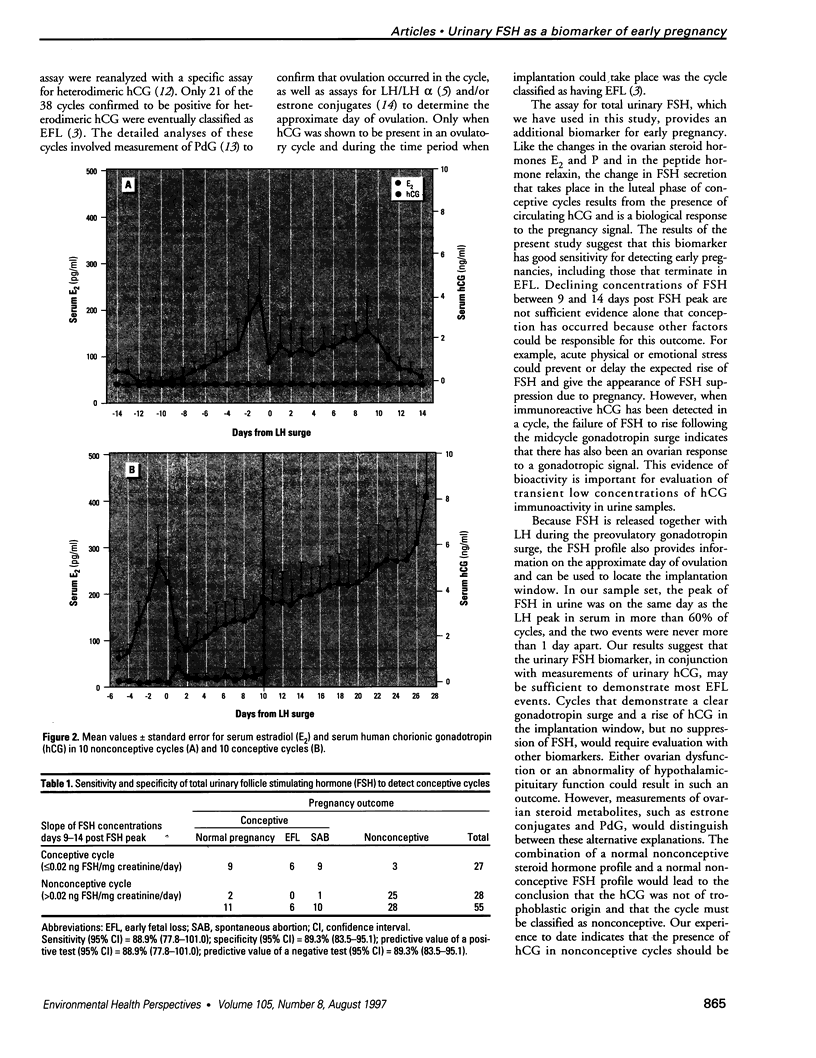
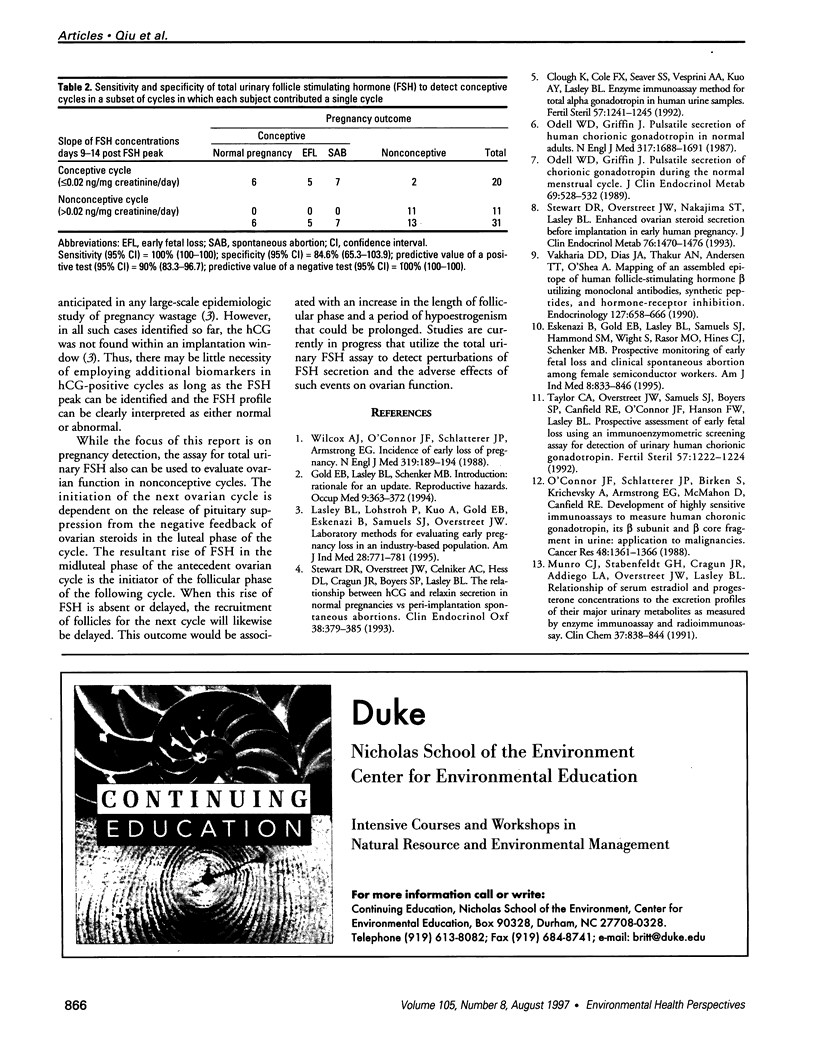
Total concentrations of follicle stimulating hormone (FSH) were evaluated in daily urine samples from conceptive and nonconceptive menstrual cycles by measurement of the FSH beta subunit following treatment of the samples to dissociate the FSH heterodimer. Samples were self-collected by normal subjects during cycles in which daily blood samples also were obtained. Daily blood and urine specimens were collected prospectively from 10 subject in conceptive cycles, which led to normal pregnancies, and from 10 subjects with bilateral tubal ligations to provide control samples form nonconceptive cycles. Mean serum and urinary FSH concentration profiles wer parallel in both groups following ovulation and during he first 9 days of the luteal phase. Mean values for both serum and urinary FSH rose significantly above the postovulatory baseline by 10-12 days following the midcycle luteinizing hormone (LH) peak in nonconceptive cycles, but did not rise at any time following ovulation during conceptive cycles. Following regression analysis of the changing FSH concentration between days 9-14 post-LH surge in conceptive cycles, a slope of </= 0.02 ng FHS/mg creatinine/day was selected as a cutoff point to identify conceptive cycles. There was a high concordance between the day of LH peak in serum and the day of FSH peak in urine. Therefore, in applying the algorithm, the day of FSH peak in urine was used to determine the days for which the FSH slope would be calculated, i.e., days 9-14 post-FSH peak in urine. The sensitivity and specificity of the change in urinary FSH concentrations to detect pregnancy in a different set of 55 cycles were found to 88.9% and 89.3%, respectively. All six cases of early fetal loss in the sample set were correctly identified. These results suggest that urinary FSH can be used as an additional biomarker for the verification of early pregnancy in prospective epidemiological studies in which early fetal loss is a suspected outcome.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Clough K. M., Cole F. X., Seaver S. S., Vesprini A., Kuo A. Y., Lasley B. L. Enzyme immunoassay method for total alpha gonadotropin in human urine samples. Fertil Steril. 1992 Jun;57(6):1241–1246. [PubMed] [Google Scholar]
- Eskenazi B., Gold E. B., Lasley B. L., Samuels S. J., Hammond S. K., Wight S., O'Neill Rasor M., Hines C. J., Schenker M. B. Prospective monitoring of early fetal loss and clinical spontaneous abortion among female semiconductor workers. Am J Ind Med. 1995 Dec;28(6):833–846. doi: 10.1002/ajim.4700280615. [DOI] [PubMed] [Google Scholar]
- Gold E. B., Lasley B. L., Schenker M. B. Introduction: rationale for an update. Reproductive hazards. Occup Med. 1994 Jul-Sep;9(3):363–372. [PubMed] [Google Scholar]
- Lasley B. L., Lohstroh P., Kuo A., Gold E. B., Eskenazi B., Samuels S. J., Stewart D. R., Overstreet J. W. Laboratory methods for evaluating early pregnancy loss in an industry-based population. Am J Ind Med. 1995 Dec;28(6):771–781. doi: 10.1002/ajim.4700280611. [DOI] [PubMed] [Google Scholar]
- Munro C. J., Stabenfeldt G. H., Cragun J. R., Addiego L. A., Overstreet J. W., Lasley B. L. Relationship of serum estradiol and progesterone concentrations to the excretion profiles of their major urinary metabolites as measured by enzyme immunoassay and radioimmunoassay. Clin Chem. 1991 Jun;37(6):838–844. [PubMed] [Google Scholar]
- O'Connor J. F., Schlatterer J. P., Birken S., Krichevsky A., Armstrong E. G., McMahon D., Canfield R. E. Development of highly sensitive immunoassays to measure human chorionic gonadotropin, its beta-subunit, and beta core fragment in the urine: application to malignancies. Cancer Res. 1988 Mar 1;48(5):1361–1366. [PubMed] [Google Scholar]
- Odell W. D., Griffin J. Pulsatile secretion of chorionic gonadotropin during the normal menstrual cycle. J Clin Endocrinol Metab. 1989 Sep;69(3):528–532. doi: 10.1210/jcem-69-3-528. [DOI] [PubMed] [Google Scholar]
- Odell W. D., Griffin J. Pulsatile secretion of human chorionic gonadotropin in normal adults. N Engl J Med. 1987 Dec 31;317(27):1688–1691. doi: 10.1056/NEJM198712313172702. [DOI] [PubMed] [Google Scholar]
- Stewart D. R., Overstreet J. W., Celniker A. C., Hess D. L., Cragun J. R., Boyers S. P., Lasley B. L. The relationship between hCG and relaxin secretion in normal pregnancies vs peri-implantation spontaneous abortions. Clin Endocrinol (Oxf) 1993 Apr;38(4):379–385. doi: 10.1111/j.1365-2265.1993.tb00518.x. [DOI] [PubMed] [Google Scholar]
- Stewart D. R., Overstreet J. W., Nakajima S. T., Lasley B. L. Enhanced ovarian steroid secretion before implantation in early human pregnancy. J Clin Endocrinol Metab. 1993 Jun;76(6):1470–1476. doi: 10.1210/jcem.76.6.8501152. [DOI] [PubMed] [Google Scholar]
- Taylor C. A., Jr, Overstreet J. W., Samuels S. J., Boyers S. P., Canfield R. E., O'Connor J. F., Hanson F. W., Lasley B. L. Prospective assessment of early fetal loss using an immunoenzymometric screening assay for detection of urinary human chorionic gonadotropin. Fertil Steril. 1992 Jun;57(6):1220–1224. [PubMed] [Google Scholar]
- Vakharia D. D., Dias J. A., Thakur A. N., Andersen T. T., O'Shea A. Mapping of an assembled epitope of human follicle-stimulating hormone-beta utilizing monoclonal antibodies, synthetic peptides, and hormone-receptor inhibition. Endocrinology. 1990 Aug;127(2):658–666. doi: 10.1210/endo-127-2-658. [DOI] [PubMed] [Google Scholar]
- Wilcox A. J., Weinberg C. R., O'Connor J. F., Baird D. D., Schlatterer J. P., Canfield R. E., Armstrong E. G., Nisula B. C. Incidence of early loss of pregnancy. N Engl J Med. 1988 Jul 28;319(4):189–194. doi: 10.1056/NEJM198807283190401. [DOI] [PubMed] [Google Scholar]