Figure 3. Mechanisms underlying the impact of lymphodepletion on adoptively transferred T cells.
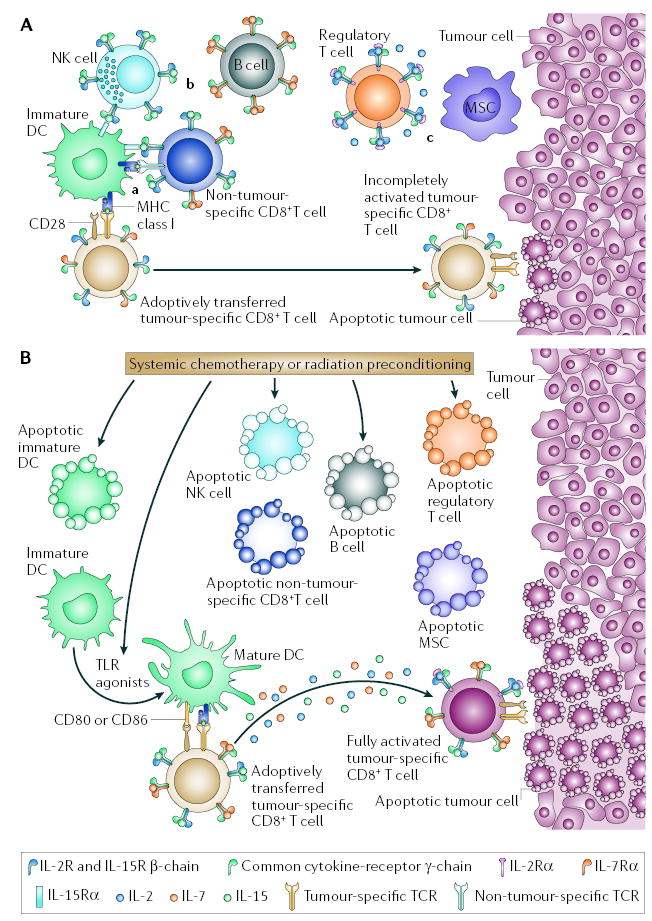
A | Adoptive cell therapy (ACT) in a lymphoreplete host. In a lymphoreplete environment, antitumour responses mediated by adoptively transferred tumour-reactive CD8+ T cells might be reduced because of: a | competition for antigen at the surface of antigen-presenting cells (APCs) and inefficient lymphocyte activation in the absence of co-stimulatory molecules by immature dendritic cells (DCs); b | reduced availability of activating cytokines (including interleukin-2 (IL-2), IL-7 and IL-15) by cellular ‘sinks’ for these cytokines, which include B cells, T cells and natural killer (NK) cells; and c | the suppressive activities of regulatory T (TReg) cells, myeloid suppressor cells (MSCs) and possibly NK cells. TReg-cell suppression is mediated by direct T-cell contact and possibly by the release of inhibitory cytokines such as IL-10 and transforming growth factor-β. MSCs mediate T-cell inhibition through direct T-cell contact and the use of enzymes involved in L-arginine metabolism such as the inducible forms of arginase and nitric-oxide synthase, ARG1 and NOS2. B | Systemic chemotherapy or radiation before ACT might modify the tumour-bearing host. APCs are reduced in number by direct killing but there might be a net increase in lymphocyte activation because of reduced competition for antigen at the APC surfaces. At the same time, as a result of the liberation of Toll-like receptor (TLR) agonists after mucosal damage, DCs might be mature, increasing lymphocyte activation. Activating cytokines, such as IL-2, IL-7 and IL-15 might be increased because of the removal of cellular ‘sinks’; and TReg cells, MSCs, NK cells and their suppressive activities are decreased. These modifications might promote the full activation of adoptively transferred tumour-reactive CD8+ T cells and ultimately tumour destruction.
