Abstract
To assess the accuracy and precision of indirect measurements of systemic arterial blood pressure (BP), results obtained with an oscillometric device (BPo) and a Doppler ultrasonic device (BPud) were compared with those obtained by direct radiotelemetry (BPrt) in 12 conscious beagles. The correlation between indirectly obtained and directly measured values for BP parameters ranged widely for the different indirect methods and sites of cuff placement, with R2 between 0.001 and 0.901. Both indirect methods underestimated all BP parameters, the degree of underestimation increasing at higher values for the BP. The highest correlation occurred when estimates were the average of 5 values consecutively obtained with the oscillometric device and cuff placement at the coccygeal artery (R2 = 0.854 for mean BPo, 0.886 for systolic BPo, and 0.901 for diastolic BPo; P < 0.0001 for all parameters) or with the ultrasonic Doppler device at the metatarsal arteries (R2 = 0.810 for systolic BPud; P < 0.0001). Multiple consecutively obtained values are advised, as this approach improves the reliability of indirect BP measurements. The strong correlation between directly measured values and estimates derived as the average of 5 consecutive indirectly obtained values indicates that the latter approach provides a useful estimate of BP in conscious dogs and is likely to be useful in monitoring disease progress and treatment in dogs with abnormal BP.
Résumé
Afin d’évaluer la justesse et la précision des mesures indirectes de la pression sanguine artérielle systémique (BP), les résultats obtenus avec un appareil oscillométrique (BPo) et un appareil à ultrasons Doppler (BPud) ont été comparés à ceux obtenus par radio-télémétrie directe (BPrt) chez 12 chiens éveillés de race Beagle. La corrélation entre les valeurs des paramètres de BP obtenues de manières indirectes et celles mesurées directement variaient grandement pour les différentes méthodes indirectes et les sites de placement du manchon, avec des valeurs de R2 entre 0,001 et 0,901. Les deux méthodes indirectes ont sous-estimé tous les paramètres de BP, le degré de sous-estimation augmentant avec des valeurs plus élevées de BP. La plus grande corrélation a été notée lorsque les estimés étaient la moyenne de 5 valeurs consécutives obtenues avec l’appareil oscillométrique et le placement du manchon au niveau de l’artère coccygienne (BPo moyenne : R2 = 0,854; BPo systolique: R2 = 0,886; BPo diastolique : R2 = 0,901; P < 0,0001 pour tous les paramètres) ou avec l’appareil à ultrasons Doppler au niveau des artères métatarsiennes (BPud systolique: R2 = 0,810; P < 0,0001). L’obtention de valeurs multiples consécutives est recommandée étant donné que cette approche améliore la fiabilité des mesures indirectes de BP. La forte corrélation entre les valeurs de mesures directes et un estimé correspondant à la moyenne de 5 valeurs obtenues indirectement démontre que cette dernière approche fournit un estimé utile de la BP chez des chiens éveillés et serait certainement utile pour suivre le progrès de maladie et le traitement de chiens avec une BP anormale.
(Traduit par Docteur Serge Messier)
Introduction
Abnormalities of systemic arterial blood pressure (BP) have been associated with a variety of diseases in dogs. Systemic hypotension can lead to tissue ischemia and injury during anesthesia or depletion of extracellular fluid volume (1). Systemic hypertension has been observed in association with kidney disease (2–4), hyperadrenocorticism (5), hypothyroidism (6), pheochromocytoma (7), and diabetes mellitus (8), and in an idiopathic form (9). Systemic hypertension has been causally associated with blindness (10,11), cardiovascular and neurologic complications (2), and progressive renal injury (2–4) in these animals.
Thus, reliable measurement of BP in conscious dogs would be a valuable clinical tool. Measurement of BP by direct techniques, with the use of intra-arterial catheterization or needle puncture, provides reliable and accurate values. Unfortunately, these direct methods are generally not applicable in clinical practice, as they may require anesthesia or sedation and a high degree of technical skill. Also, their invasiveness creates opportunities for infection and hemorrhage, as well as anxiety-induced artifactual elevation of BP.
Several methods indirectly estimate BP by use of an external, inflatable cuff and commercially available detection devices. One such method involves the oscillometric principle, introduced by Marey in 1876 (12). Oscillometric devices use variations in amplitude of oscillations during compression of the arterial wall to estimate arterial pressure (BPo). Another method commonly used for estimating BP employs the ultrasonic Doppler flow detector, which estimates arterial pressure (BPud) by detecting changes induced by blood flow during external compression by an inflatable cuff.
Several studies have evaluated indirect BP methods in dogs; however, most have either used anesthetized animals for comparison with direct measurements (13–19) or have not made comparisons with directly obtained values (20–22). Movement, increased skeletal muscle tone, and lability of measured parameters make indirect measurements in conscious animals substantially more problematic. A few studies have addressed this issue by comparing direct and indirect determinations in conscious animals (23–25).
A radiotelemetric system for measurement of BP, heart rate (HR), and movement in experimental studies has been adapted for use in dogs (26,27). This method involves surgical placement of a small implant into the subcutaneous space in the flank. By using this system, it is possible to compare results for BP obtained by direct, radiotelemetric measurement (BPrt) with simultaneously obtained results from indirect measuring devices in conscious, minimally restrained dogs.
The purpose of this study was to evaluate the reliability of indirect BP estimation by oscillometric or ultrasonic Doppler methods by comparing the results with measurements simultaneously obtained by radiotelemetry.
Materials and methods
Animals
Twelve adult, sexually intact beagles (7 males and 5 females) with a mean weight of 11.1 ± 1.6 kg were procured from the Laboratory Animal Facility of the University of Georgia College of Veterinary Medicine. All animals had been vaccinated against common viral diseases and treated for ectoparasites and endoparasites. In 6 of the beagles, a renal mass had been reduced by approximately seven-eighths by partial nephrectomy (28) at least 2 months previously as part of another study. All the dogs were negative for microfilariae of Dirofilaria immitis (canine heartworm). All studies were conducted in accord with the Guidelines for Care and Use of Laboratory Animals of the US National Institutes of Health and were approved by the Institutional Animal Care Committee of the University of Georgia.
Radiotelemetry system
The use of the radiotelemetry system has previously been described (29,30). Surgical placement of the implant (model TA11PAD-70; Data Sciences International, St. Paul, Minnesota, USA) was performed aseptically in a dedicated suite after anesthesia had been induced. Briefly, the implant catheter was inserted into a muscular branch of the femoral artery and advanced to the level of the descending aorta, and the implant body was placed in the subcutaneous space of the flank. An interval of at least 2 wk was allowed before studies were performed.
For these studies, a radio signal transmitted pressure-waveform data via a receiver (model RLA-2000; Data Sciences International), placed adjacent to the BP measurement table, to a computer (ProLinea 4/66; Compaq Computer Corporation, Houston, Texas, USA). The temporal pattern of BP was reconstructed from the modulations in the radio signal. The radiotelemetric values for systolic, diastolic, and mean BP (SBPrt, DBPrt, and MBPrt, along with HRrt, were determined by computer-assisted analysis (Dataquest LabPro; Data Sciences International), as previously described (31–35).
Direct values were obtained either as the average of 5-s recordings every 30 s or from continuous waveform recordings during the indirect-device cycle, the mean of systolic pressures from the first 15 s being taken as SBPrt, the mean of all values from the middle 15 s as MBPrt, and the mean of the diastolic pressures from the last 15 s as DBPrt. When the 2 direct methods were compared in 90 BP determinations, they provided nearly identical estimates of BP (mean difference, 0.68 ± 0.31 mm Hg; not significantly different).
Indirect BP estimates
All indirect estimates were recorded from conscious beagles with the use of either an oscillometric device (Dinamap, model 8300; Critikon, Tampa, Florida, USA) or an ultrasonic Doppler device (model 811; Parks Medical Electronics, Beaverton, Oregon, USA). For each indirect device, BP estimates were obtained at the same time as direct measurements: 1 observer used the indirect device, and another simultaneously operated the direct telemetry device. Measurements with the 2 indirect devices were obtained at different times, generally on a different day.
The oscillometric device provided estimates of mean, diastolic, and systolic BP (MBPo, DBPo, and SBPo), as well as HRo. The ultrasonic Doppler device provided estimates of systolic BP (SBPud) only. The accuracy of the oscillometric indirect pressure transducer was verified according to the manufacturer’s instructions, with the aid of a mercury manometer. The accuracy of the aneroid manometer used in conjunction with the ultrasonic Doppler device was similarly verified.
The dogs were acclimated to the measurement procedure in the week before the studies and were either restrained gently on the measurement table or placed in Pavlovian slings for at least 5 min before indirect BP estimates, according to the dog’s individual preference. Because preliminary studies demonstrated that movement interfered with the reliability of both indirect methods, estimates obtained while a subject was moving were discarded. Limb and tail circumferences were between 6 and 10 cm, and a #3 neonatal cuff (Disposa-Cuf; Critikon) was used to meet established criteria for cuff size (14,17).
The cuff for the oscillometric device was attached to 5 sites. The coccygeal artery was occluded by placing the cuff 1 cm distal to the base of the tail, with the artery arrow positioned along the ventral midline. The metacarpal arteries were occluded by placing the cuff on the distal portion of the thoracic limb between the carpal and metacarpal pads, with the artery arrow facing the palmar aspect of the paw. The median artery was occluded by placing the cuff on the proximal portion of the thoracic limb between the elbow and the carpal pad, with the artery arrow over the medial surface of the limb. The metatarsal arteries were occluded by placing the cuff on the pelvic limb proximal to the metatarsal pad and below the hock, with the artery arrow facing the plantar aspect of the paw. The cranial tibial artery was occluded by placing the cuff on the pelvic limb proximal to the hock, with the artery arrow facing cranially. If the oscillometric device failed to display a complete set of estimated values for 3 consecutive measurements, the cuff was repositioned, and the measurements were repeated.
The Doppler flow probe was palmar in the thoracic limb (median artery) and plantar in the pelvic limb (tibial and metatarsal arteries). For probe placement, the surface of a limb was shaven and an aqueous ultrasonic transmission gel (Aquasonic 100; Parker Laboratories, Orange, New Jersey, USA) was applied between the probe and the skin. The position of the probe was adjusted until a clear signal was obtained from the amplified loudspeaker, and then the probe was fixed into position with tape. The occluding cuff, with an aneroid manometer (Tomac, Tokyo, Japan) attached, was secured proximally to the Doppler flow detector. To estimate SBP, the pressure in the cuff was increased until the flow signal disappeared and then was gradually decreased, at a rate of approximately 2 mm Hg/s. The sphygmomanometer pressure coinciding with the 1st audible flow signal was taken as SBPud.
For both indirect devices, we attempted to ensure that the cuff was at or within 3 cm of the heart level. For the Doppler device, the cuff and transducer were maintained at or near the same level relative to the heart.
Site-selection studies
Site-selection studies were performed in the 6 normal beagles (3 male and 3 female) at spontaneous BP. Initially, 5 measurement sites (coccygeal, metacarpal, metatarsal, tibial, and median arteries) were evaluated with the oscillometric method, at least 10 measurements being obtained per site per animal. On the basis of these studies, the 2 sites with the strongest correlation between SBPo and SBPrt were selected for further evaluation.
Initial studies were also performed with the ultrasonic Doppler device in the 6 normal beagles. Three sites were evaluated (median, tibial, and metatarsal arteries), with a minimum of 15 measurements at each site. The site with the strongest correlation between SBPud and SBPrt was selected for further evaluation.
Pharmacologic alteration of BP
To test the ability of the oscillometric and ultrasonic Doppler devices to estimate BP over a broad range of values, BP was pharmacologically altered. Three individuals obtained at least 60 measurements each with the Doppler device.
To reduce BP, we gave the animals 2 mg of hydralazine (UDL Laboratories, Rockford, Illinois, USA) and 2.5 mg of atenolol (Lederle Laboratories, Pearl River, New York, USA) per kilogram of body weight (BW) orally twice daily for 2 d. On day 3, the beagles received 6 mg of hydralazine/kg BW and 7.5 mg of atenolol/kg BW orally approximately 2 h before the studies. This approach led to a decrement of approximately 20 mm Hg in MBP in each dog on day 3.
After a recovery period of at least 24 h, additional studies were conducted with the BP elevated. The beagles received 0.03 mg of phenylephrine (Schein Pharmaceutical, Port Washington, New York, USA) per milliliter of lactated Ringer’s solution, with the dosage adjusted to maintain a stable elevation of approximately 30 to 50 mm Hg in MBP. Each beagle received a total dose of approximately 2.25 mg of phenylephrine.
Statistical analyses
All values are expressed as mean ± standard deviation (s). Simple linear regression analysis was used to evaluate the relationships between the indirect and direct values. A commercial software package (Statview 4.5; Abacus Concepts, Berkeley, California, USA) was used. A P-value of less than 0.05 was taken to indicate a statistically significant difference. The mean differences between simultaneously obtained indirect estimates and direct measurements were determined. The average of 5 consecutive simultaneously obtained indirect and direct determinations was evaluated to determine if averaging would increase the strength of relations between indirect and direct results. Statistical analysis included Bland–Altman limits-of-agreement plots (36).
Results
Site-selection studies
A total of 424 simultaneous direct measurements and indirect determinations by the oscillometric method were made at 5 sites in 6 normal, conscious, unmedicated beagles. The correlations between BPrt and BPo varied, R2 ranging from 0.001 to 0.271. The SBPo determined at the coccygeal and tibial sites provided the best correlations (R2 = 0.247 and 0.271, respectively; P < 0.0001 for both), and these 2 sites were therefore chosen for further evaluation of the oscillometric device.
A total of 273 measurements were made at 3 sites in 6 normal, conscious, unmedicated beagles by the ultrasonic Doppler method. There were significant correlations between SBPrt and SBPud at all 3 sites, R2 ranging from 0.174 to 0.827. The metatarsal site provided the strongest correlation (R2 = 0.827), and this site was therefore selected for further evaluation of the Doppler device.
Comparative studies
Comparative studies were conducted at 2 sites for the oscillometric device (264 simultaneous measurements) and 1 site for the ultrasonic Doppler device (270 simultaneous measurements) in 12 conscious beagles, 6 normal and 6 with reduced renal mass. As there were no significant differences between correlations obtained in the 2 groups of dogs or between individuals making the readings, all results were pooled.
The strongest correlations (Table I) were for BP estimates at the coccygeal site with the oscillometric device. However, all correlations for the tibial site with this device were also significant. With the ultrasonic Doppler device, correlation was good at the metatarsal site.
Table I.
Correlation of simultaneous indirect and direct blood pressure (BP) measurements in 12 conscious beagles
|
R2;a mean ± s (and range of values), mm Hgb |
|||
|---|---|---|---|
| Method (and n) | SBP | MBP | DBP |
| Oscillometry at coccygeal site (174) | 0.786 | 0.740 | 0.720 |
| 158.3 ± 37.8 | 112.9 ± 29.5 | 88.8 ± 25.8 | |
| (108–268) | (65–190) | (52–163) | |
| Oscillometry at tibial site (90) | 0.251 | 0.347 | 0.422 |
| 151.7 ± 28.7 | 110.9 ± 23.5 | 88.4 ± 22.1 | |
| (106–222) | (76–170) | (56–152) | |
| Doppler ultrasonography at metatarsal site (270) | 0.753 | ND | ND |
| 167.3 ± 39.7 | ND | ND | |
| (87–199) | ND | ND | |
n — number of simultaneous measurements; s — standard deviation; S — systolic;
M — mean; D — diastolic; ND — not determined
All linear regression relationships were significant at P < 0.0001
Measurements were obtained by the direct radiotelemetric method
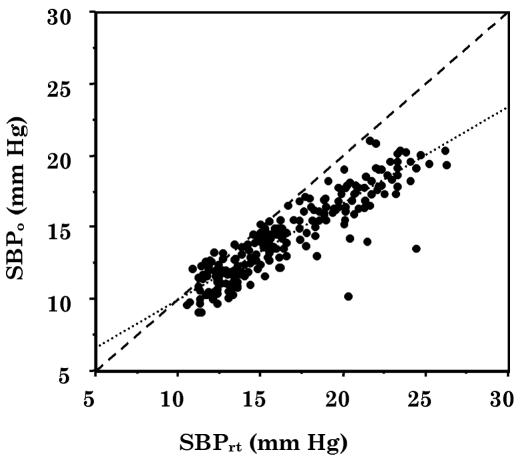
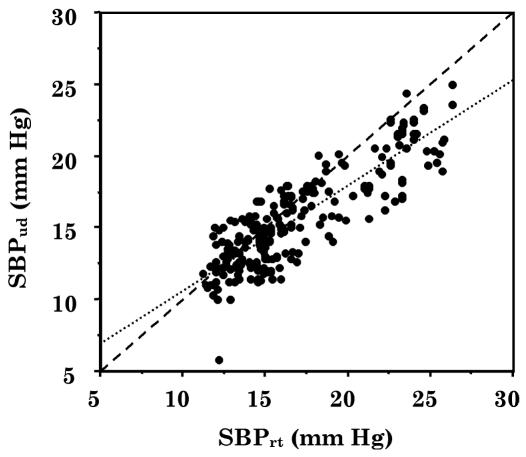
At SBPrt values above 107 mm Hg, the oscillometric device consistently underestimated SBP (Figure 1). A similar pattern of increasing underestimation was observed for MBPo and DBPo at higher values. Although a similar trend of underestimation at higher SBPrt (above 128 mm Hg) was observed with the ultrasonic Doppler device, this device was less consistent and provided both overestimated and underestimated values over the entire range of SBP (Figure 2).
Figure 1.
Simple linear regression relation (dotted line) and line of identity (dashed) for systolic arterial blood pressure (BP) values obtained in 12 conscious beagles by oscillometry (SBPo) at the coccygeal artery site and by radiotelemetry (SBPrt). Each data point corresponds to simultaneously obtained values for SBPo and SBPrt. There were 174 comparisons (R2 = 0.786; P < 0.0001).
Figure 2.
Simple linear regression relation (dotted line) and line of identity (dashed) for systolic arterial BP values obtained in 12 conscious beagles by Doppler ultrasonography (SBPud) at the metatarsal arteries site and by radiotelemetry (SBPr t). Each data point corresponds to simultaneously obtained values for SBPud and SBPrt. There were 270 comparisons (R2 = 0.753; P < 0.0001).
Using average results for 5 consecutive simultaneous direct and indirect determinations improved the reliability of the indirect estimates with both devices (Table II).
Table II.
Correlation of indirect and direct BP measurements in 12 conscious beagles with the use of the averages of 5 consecutive simultaneous determinations
|
R2; mean ± s (and range of values), mm Hg
|
|||
|---|---|---|---|
| Method (and n) | SBP | MBP | DBP |
| Oscillometry at coccygeal site (35) | 0.886a | 0.854a | 0.901a |
| 150.2 ± 32.2 | 109.2 ± 24.7 | 86.3 ± 22.1 | |
| 112–213 | 79–147 | 58–119 | |
| Oscillometry at tibial site (18) | 0.381b | 0.546b | 0.629a |
| 151.7 ± 28.9 | 110.9 ± 23.4 | 88.4 ± 21.8 | |
| 109–199 | 79–153 | 59–129 | |
| Doppler ultrasonography at metatarsal site (54) | 0.810a | ND | ND |
| 149.2 ± 25.8 | ND | ND | |
| 117–192 | ND | ND | |
Significant at P < 0.0001
Significant at P < 0.05
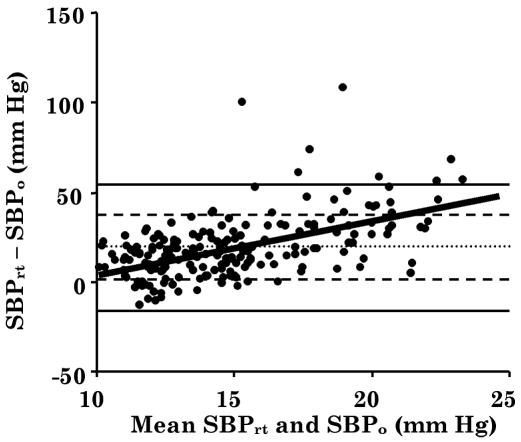
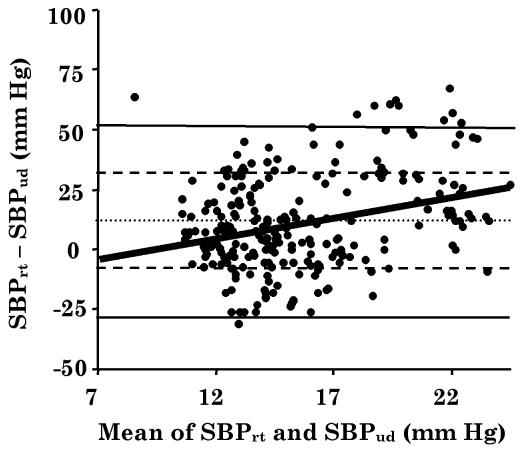
The Bland–Altman limits-of-agreement plots (36) demonstrated the bias (mean difference) of the oscillometric device (Figure 3) and the ultrasonic Doppler device (Figure 4) and the trend for increased overestimation of the indirect devices at higher SBP. The bias of the oscillometric device at the coccygeal site for 174 simultaneous measurements of MBPo, SBPo, and DBPo was 10.8 ± 15.6, 20.0 ± 18.2, and 5.3 ± 15.3, respectively. The bias of the ultrasonic Doppler device at the metatarsal site for 270 simultaneous measurements of SBPud was 11.6 ± 19.7. Thus, there was a heterogeneous underestimation by the indirect devices. For the oscillometric device, 14.4%, 24.7%, and 25.9% of values for SBPo, MBPo, and DBPo, respectively, were within 5 mm Hg of the simultaneously obtained radiotelemetric values, and 29.9%, 48.9%, and 56.9% were within 10 mm Hg. For the Doppler device, 21.5% of values for SBPud were within 5 mm Hg and 43.0% within 10 mm Hg of the simultaneously obtained SBPrt.
Figure 3.
Bland–Altman limits-of-agreement plots (36) for SBPrt and SBPo at the coccygeal site. Each data point corresponds to the difference between 1 pair of simultaneously obtained direct and indirect measurements. Also depicted are the mean overall difference (dotted line), the mean ± 1 standard deviation (s) (dashed line), the mean ± 2 s (solid line), and the simple linear regression relation between the differences and averages of the 2 methods (thick solid diagonal line).
Figure 4.
Bland–Altman limits-of-agreement plots for SBPr t and SBPud. Each data point corresponds to the difference between 1 pair of simultaneously obtained direct and indirect measurements. Also depicted are the mean overall difference (dotted line), the mean ± 1 s (dashed line), the mean ± 2 s (solid line), and the simple linear regression relation between the differences and averages of the 2 methods (thick solid diagonal line).
Discussion
Measurement of BP has become a valuable clinical tool in veterinary medicine for the identification of animals with systemic hypertension. High BP has been associated with kidney disease (2–4), hyperadrenocorticism (5), hypothyroidism (6), pheochromocytoma (7), and diabetes mellitus (8), and also exists in an idiopathic form (9). Since elevations in BP are causally associated with blindness (10,11), cardiovascular and neurologic complications (2), and progressive renal injury (2–4), reliable measurements of BP will allow veterinarians to monitor BP, make informed decisions regarding institution of antihypertensive therapy, and assess the efficacy of such therapy.
Although direct methods for measuring BP are reliable, the procedures are invasive and technically difficult, and they create the potential for complications and artifact. To be relevant to the conscious patient, evaluations of the reliability of indirect methods should be accomplished with simultaneous use of direct methods in conscious animals. Many of the previous studies comparing results of indirect methods and directly obtained values for BP have relied on anesthesia or sedation (13–19).
In this study, as with previous studies (16,24,25), the indirect methods consistently underestimated BP in conscious dogs. In our study, the mean underestimation varied from 2.8 to 20.4 mm Hg for the various pressure–site combinations with the oscillometric device; the mean underestimation was 11.6 mm Hg for SBP at the metatarsal arteries with the ultrasonic Doppler device. The Association for the Advancement of Medical Instrumentation (AAMI) suggested that indirect devices intended for use in humans should differ from a reference method by a mean of less than 5 ± 8 mm Hg (31). The larger values for mean difference and s for the indirect devices in this study reflect an increased degree of inaccuracy and imprecision, respectively. The AAMI criteria for BP devices used in humans also specifies that 95% of indirect estimates should lie within 10 mm Hg of the direct measurements and that 85% of indirect estimates should lie within 5 mm Hg of the direct measurements. Although neither of the indirect methods that we evaluated met these criteria, many indirect devices, including some that are very similar to those tested in the present study (32), meet these criteria in humans. An oscillometric device reportedly met the AAMI criteria in anesthetized cats (33). Until devices that meet AAMI criteria in conscious dogs are identified, the strong correlations demonstrated in the present study for the devices evaluated indicate that these devices can provide only useful approximations of BP in conscious dogs.
Several studies have addressed the relationship between simultaneously obtained direct and indirect values for BP in conscious dogs. Our results are consistent with those from a previous study that addressed this relationship with the use of an ultrasonic Doppler device at the median artery site (24); results from linear regression analysis of the ultrasonic Doppler estimates in conscious dogs indicated an R2 between 0.410 and 0.656. Our study indicated that estimates obtained from the median artery site were inferior to those obtained from the metatarsal arteries site. Results from another study comparing simultaneous indirect estimates obtained with an oscillometric device and direct measurements obtained by radiotelemetric implants in conscious dogs (25) supported the utility of indirect oscillometric estimates at the coccygeal artery, as did our findings. Another group of investigators demonstrated inaccuracies of the oscillometric and Doppler devices in clinical patients (23), similar to those reported herein, and suggested the importance of defining the characteristics of these methods (34).
The radiotelemetric system that we used provided values for MBP, SBP, and DBP for comparison with simultaneously obtained indirect BP measurements. Studies have verified the precision and accuracy of this direct BP measurement method (26,27,35,37–39). In a study performed in our laboratory, direct radiotelemetric measurements correlated strongly with simultaneous directly obtained intra-arterial pressure values in 3 cats (R2 for MBP = 0.999, SBP = 0.997, DBP = 0.998; P < 0.0001), with bias values of less than 2 mm Hg 3 mo after implantation (35). Similar implants were in place for 1 to 3 mo in the present study.
Inaccuracies from oscillometric BP estimation devices might be linked to many sources. Since this method relies on the amplitude of cuff-pressure oscillations for identification of BP, shivering or other movement by a dog interferes with the ability of the device to provide an accurate estimate. We addressed this problem by familiarizing the dogs with the measurement room beforehand, limiting noise and activity in the room, and having the dogs gently restrained by familiar personnel. If an animal moved during a BP determination sequence, the values were discarded. Many of the beagles slept through the procedures. Another potential source of inaccuracy is BP lability. The oscillometric determination sequence lasts approximately 30 to 150 s. If BP changes during the sequence, the BP estimate could be faulty. With the aid of frequent BP determination by the radiotelemetric system, we were able to reduce this source of error.
The ultrasonic Doppler method relies on the ability of the user to hear arterial-wall sounds, which could be masked by patient movement, making it difficult to determine SBP. As with the oscillometric method, anatomic anomalies could influence the ability of the user to obtain an accurate Doppler measurement. The average determination sequence for the ultrasonic Doppler method is approximately 15 to 25 s, and this method would be affected by a sudden change in BP during this interval, as with the oscillometric method. Our discarding of estimations if the dog moved during the determination sequence should have minimized these known sources of error with the ultrasonic Doppler method.
In conclusion, the oscillometric and Doppler techniques provided an approximation of BP in conscious dogs that correlated well with direct measurements of BP. Use of the oscillometric device at the coccygeal artery provided the strongest correlations. However, the Doppler device had a smaller bias and similar, though somewhat lower, correlation of SBPud with SBPrt. Although the results did not meet the AAMI criteria for accuracy and precision, the strong correlation between direct and indirect measurements obtained as an average of 5 consecutive indirect estimates with use of the oscillometric device at the coccygeal artery or the ultrasonic Doppler device at the metatarsal arteries supports the use of these methods for BP determination in conscious dogs.
Acknowledgment
This work was supported in part by the Veterinary Medical Experiment Station of the University of Georgia College of Veterinary Medicine.
References
- 1.Littman MP, Drobatz KJ. Hypertensive and hypotensive disorders. In: Ettinger SJ, ed. Textbook of Veterinary Internal Medicine. Philadelphia: W.B. Saunders, 1995:93–100.
- 2.Jacob F, Polzin DJ, Osborne CA, et al. Association between initial systolic blood pressure and risk of developing a uremic crisis or of dying in dogs with chronic renal failure. J Am Vet Med Assoc. 2003;222:322–329. doi: 10.2460/javma.2003.222.322. [DOI] [PubMed] [Google Scholar]
- 3.Brown SA, Brown CA, Hendi R. Does systemic hypertension damage the canine kidney? [abstract] J Vet Intern Med. 2000;14:351A. [Google Scholar]
- 4.Finco DR. Association of systemic hypertension with renal injury in dogs with induced renal failure. J Vet Intern Med. 2004;18:289–294. doi: 10.1892/0891-6640(2004)18<289:aoshwr>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 5.Ortega TM, Feldman EC, Nelson RW, et al. Systemic arterial blood pressure and urine protein/creatinine ratio in dogs with hyperadrenocorticism. J Am Vet Med Assoc. 1996;209:1724–1729. [PubMed] [Google Scholar]
- 6.Cowgill LD. Systemic hypertension. In: Kirk RW, ed. Current Veterinary Therapy IX. Philadelphia: W.B. Saunders, 1986:360–364.
- 7.Barthez PY, Marks SL, Woo J, et al. Pheochromocytoma in dogs: 61 cases (1984–1995) J Vet Intern Med. 1997;11:272–278. doi: 10.1111/j.1939-1676.1997.tb00464.x. [DOI] [PubMed] [Google Scholar]
- 8.Struble AL, Feldman EC, Nelson RW, et al. Systemic hypertension and proteinuria in dogs with diabetes mellitus. J Am Vet Med Assoc. 1998;213:822–825. [PubMed] [Google Scholar]
- 9.Bovee KC, Littman MP, Crabtree BJ, et al. Essential hypertension in a dog. J Am Vet Med Assoc. 1989;195:81–86. [PubMed] [Google Scholar]
- 10.Sansom J, Bodey A. Ocular signs in four dogs with hypertension. Vet Rec. 1997;140:593–598. doi: 10.1136/vr.140.23.593. [DOI] [PubMed] [Google Scholar]
- 11.Littman MP, Robertson JL, Bovee KC. Spontaneous systemic hypertension in dogs: five cases (1981–1983) J Am Vet Med Assoc. 1988;193:486–494. [PubMed] [Google Scholar]
- 12.Geddes L. The indirect measurement of blood pressure. In: Geddes L, ed. Handbook of Blood Pressure Measurement. Clifton, New Jersey: Humana Press, 1991:51–118.
- 13.Geddes LA, Combs W, Denton W, et al. Indirect mean arterial pressure in the anesthetized dog. Am J Physiol. 1980;238:H664–H666. doi: 10.1152/ajpheart.1980.238.5.H664. [DOI] [PubMed] [Google Scholar]
- 14.Sawyer DC, Brown M, Striler EL, et al. Comparison of direct and indirect blood pressure measurement in anesthetized dogs. Lab Anim Sci. 1991;41:134–138. [PubMed] [Google Scholar]
- 15.Gains MJ, Grodecki KM, Jacobs RM, et al. Comparison of direct and indirect blood pressure measurements in anesthetized dogs. Can J Vet Res. 1995;59:238–240. [PMC free article] [PubMed] [Google Scholar]
- 16.Sawyer DC, Guikema AH, Siegel EM. Evaluation of a new oscillometric blood pressure monitor in isoflurane-anesthetized dogs. Vet Anaesth Analg. 2004;31:27–39. doi: 10.1111/j.1467-2995.2004.00141.x. [DOI] [PubMed] [Google Scholar]
- 17.Valtonen MH, Eriksson LM. The effect of cuff width on accuracy of indirect measurement of blood pressure in dogs. Res Vet Sci. 1970;11:358–362. [PubMed] [Google Scholar]
- 18.Bodey AR, Young LE, Bartram DH, et al. A comparison of direct and indirect (oscillometric) measurements of arterial blood pressure in anaesthetised dogs, using tail and limb cuffs. Res Vet Sci. 1994;57:265–269. doi: 10.1016/0034-5288(94)90116-3. [DOI] [PubMed] [Google Scholar]
- 19.Meurs KM, Miller MW, Slater MR. Comparison of the indirect oscillometric and direct arterial methods for blood pressure measurements in anesthetized dogs. J Am Anim Hosp Assoc. 1996;32:471–475. doi: 10.5326/15473317-32-6-471. [DOI] [PubMed] [Google Scholar]
- 20.Remillard RL, Ross JN, Eddy JB. Variance of indirect blood pressure measurements and prevalence of hypertension in clinically normal dogs. Am J Vet Res. 1991;52:561–565. [PubMed] [Google Scholar]
- 21.Coulter DB, Keith JC., Jr Blood pressures obtained by indirect measurement in conscious dogs. J Am Vet Med Assoc. 1984;184:1375–1378. [PubMed] [Google Scholar]
- 22.Mishina M, Watanabe T, Fujii K, et al. A clinical evaluation of blood pressure through non-invasive measurement using the oscillometric procedure in conscious dogs. J Vet Med Sci. 1997;59:989–993. doi: 10.1292/jvms.59.989. [DOI] [PubMed] [Google Scholar]
- 23.Stepien RL, Rapoport GS. Clinical comparison of three methods to measure blood pressure in nonsedated dogs. J Am Vet Med Assoc. 1999;215:1623–1628. [PubMed] [Google Scholar]
- 24.Chalifoux A, Dallaire A, Blais D, et al. Evaluation of the arterial blood pressure of dogs by two noninvasive methods. Can J Comp Med. 1985;49:419–423. [PMC free article] [PubMed] [Google Scholar]
- 25.Bodey AR, Michell AR, Bovee KC, et al. Comparison of direct and indirect (oscillometric) measurements of arterial blood pressure in conscious dogs. Res Vet Sci. 1996;61:17–21. doi: 10.1016/s0034-5288(96)90104-6. [DOI] [PubMed] [Google Scholar]
- 26.Sherer AD, McCarthy MP, Becker RA, et al. The use of radiotelemetry in conscious dogs to evaluate cardiovascular responsiveness. Contemp Top Lab Anim Sci. 1993;32:48. [Google Scholar]
- 27.Truett AA, West DB. Validation of a radiotelemetry system for continuous blood pressure and heart rate monitoring in dogs. Lab Anim Sci. 1995;45:299–302. [PubMed] [Google Scholar]
- 28.Brown SA, Finco DR, Crowell WA, et al. Single-nephron adaptations to partial renal ablation in the dog. Am J Physiol. 1990;258:F495–F503. doi: 10.1152/ajprenal.1990.258.3.F495. [DOI] [PubMed] [Google Scholar]
- 29.Belew AM, Barlett T, Brown SA. Evaluation of the white-coat effect in cats. J Vet Intern Med. 1999;13:134–142. doi: 10.1892/0891-6640(1999)013<0134:eotwce>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 30.Brown SA, Langford K, Tarver S. Effects of certain vasoactive agents on the long-term pattern of blood pressure, heart rate, and motor activity in cats. Am J Vet Res. 1997;58:647–652. [PubMed] [Google Scholar]
- 31.Prisant LM, Alpert BS, Robbins CB, et al. American National Standard for nonautomated sphygmomanometers. Summary report. Am J Hypertens. 1995;8:210–213. doi: 10.1016/0895-7061(94)00175-B. [DOI] [PubMed] [Google Scholar]
- 32.O’Brien E, Atkins N, Staessen J. State of the market: a review of ambulatory blood pressure monitoring devices. Hypertension. 1995;26:835–842. doi: 10.1161/01.hyp.26.5.835. [DOI] [PubMed] [Google Scholar]
- 33.Pedersen KM, Butler MA, Ersboll AK, et al. Evaluation of an oscillometric blood pressure monitor for use in anesthetized cats. J Am Vet Med Assoc. 2002;221:646–650. doi: 10.2460/javma.2002.221.646. [DOI] [PubMed] [Google Scholar]
- 34.Stepien RL, Rapoport GS, Henik RA, et al. Comparative diagnostic test characteristics of oscillometric and Doppler ultrasonographic methods in the detection of systolic hypertension in dogs. J Vet Intern Med. 2003;17:65–72. doi: 10.1892/0891-6640(2003)017<0065:cdtcoo>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 35.Brown S, Langford K, Tarver S. Effects of pharmacological agents on diurnal pattern of blood pressure, heart rate, and motor activity in cats. Am J Vet Res. 1997;58:647–652. [PubMed] [Google Scholar]
- 36.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 37.Schnell CR, Wood JM. Measurement of blood pressure and heart rate by telemetry in conscious, unrestrained marmosets. Am J Physiol. 1993;264((5 pt 2)):H1509–H1516. doi: 10.1152/ajpheart.1993.264.5.H1509. [DOI] [PubMed] [Google Scholar]
- 38.Sadoff DA, Fischel RJ, Carroll ME, et al. Chronic blood pressure radiotelemetry in rhesus macaque. Lab Anim Sci. 1992;42:78–80. [PubMed] [Google Scholar]
- 39.Chen Q, Okeda R, Matsuo T. Selective distribution of medial thickening in the renal vessels in experimental hypertension. Pathol Int. 1994;44:569–577. doi: 10.1111/j.1440-1827.1994.tb01717.x. [DOI] [PubMed] [Google Scholar]