Abstract
Factitious disease is defined as the intentional production (or feigning) of disease in oneself to relieve emotional distress by assuming the role of a sick person. Although the self-induction of disease is a conscious act, the underlying motivation is usually unconscious. It has been estimated that 3% to 5% of physician-patient encounters involve factitious disease. This article presents 6 case studies from Baylor University Medical Center that highlight various clinical aspects of factitious disease. Patients with factitious diseases are extremely difficult to recognize because they do not appear different from patients with authentic causes of similar symptoms, because their psychiatric abnormalities are not appreciated, and because doctors and nurses have alowindex of suspicion. Since patients with factitious disease present a false medicalhistory, their physicians prescribe unnecessary procedures and therapies that may result in iatrogenic disease. In many cases, damage to these patients from doctors' actions exceeds the harm resulting from the patients' self-induced illness. The clues that should suggest factitious disease, the diagnostic roles of the clinician and a consulting psychiatrist, and the ethical conflicts that confront doctors taking care of such patients are discussed. To help keep factitious disease in clinical perspective, one of the case studies involves the antithesis of factitious disease, where a patient was mistakenly diagnosed as having psychogenic pain when in fact the symptoms were caused by an overlooked physical disease. Better knowledge of the clinical features of factitious disease might have prevented the disastrous outcome.
It is said that Claudius Galen,∗ a second-century Roman physician (1), was the first to call attention to factitious diseases. In a treatise entitled On Feigned Diseases and the Detection of Them, Galen apparently provided a long list of symptoms that patients had feigned or induced in themselves to simulate illness (2). In a book published in 1843, Hector Gavin† first used the term “factitious disease” (4). He mainly described soldiers and seamen who mimicked illness to incite compassion or attention. He also emphasized the importance of factitious diseases in the private practice of medicine as he described a subgroup of women “who assume the semblance of disease for some inexplicable cause” (5). Gavin had a good sense of humor: “The Irish are the most numerous and expert at counterfeiting disease. The Lowland Scotsman comes next to the Irishman, and what he wants in address he makes up in obstinacy” (3).
In 1934, Karl A. Menninger (1893–1990) discussed the compulsion of “certain neurotic characters” to secure repeated surgical operations (6). Such patients force themselves on a surgeon, preferably one who is strong and dynamic, demanding an operation either verbally or in some physiological way. “There is frequently no doubt about the necessity of the operation, the only question being whether the necessity is psychological or physical.” Ironically, such an operation may relieve an emotional problem (at least temporarily) which a psychiatrist had treated without success. Menninger concluded that polysurgical addiction is a form of focal self-destruction, a “partial suicide” in which responsibility for the act is partially shifted to the surgeon. Regardless of the motivation, polysurgery is common in many forms of factitious disease, as will be illustrated in our case studies.
In 1951, Asher‡ created the name Munchausen's syndrome to describe one form of factitious disease (10). According to Feldman (2), Baron von Münchhausen (1720–1797)
was an honorable man and a famous and colorful war hero. After his retirement from the German cavalry, he spent his time traveling around his homeland, delighting listeners with tales of his military adventures. Although he embellished some of his stories for dramatic effect, they were essentially true. Historical records bear no evidence of his having feigned illness or duped people into caring for him. However, Rudolph Erich Raspe, a thief on the run from German authorities, appropriated and anglicized the Baron's name for the title of a 1785 pamphlet of outrageous and patently false tales, Baron Munchausen's Narrative of His Marvelous Travels and Campaigns in Russia.
Subsequently, lying and Munchausen were connected in German culture when fibbing children were called “little Munchausens” (11). In his 1951 paper, Asher described a series of patients whose medical histories consisted mainly of falsehoods and who visited and deceived an astounding number of hospitals and doctors. A large number of abdominal surgical scars characterized this condition. “Like the famous Baron von Munchausen, the persons affected have always traveled widely; and their stories, like those attributed to him, are both dramatic and untruthful. Accordingly, the syndrome is respectfully dedicated to the baron and named after him” (10).
According to current usage, Munchausen's syndrome is considered to be the most extreme form of factitious disease. Clinically, such patients have a seemingly insatiable compulsion to mimic serious and life-threatening disease. They become “hospital hobos” with no job and no roots (12). As they wander from one hospital to the next, they assume different character roles, like an actor. They may pretend to be anything from war heroes to priests from a monastery. In one case a prostitute from Piccadilly identified herself as a Texan (13). Their attitude towards doctors and nurses is usually dramatic, aggressive, uncooperative, and sometimes threatening. Defined this way, Munchausen's syndrome is rare, and most patients are men. The underlying psychiatric illness and the motivating factors vary from patient to patient (13).
There is a much larger group of patients with factitious disease who are repeatedly hospitalized for diagnostic tests and treatment but who are not dramatic or aggressive in their demeanor. After cooperative behavior in the hospital, they quietly return to a job. Nevertheless, disease simulation is central to their emotional life, and their relationship to doctors may be as intense as addiction (14). They soon will repeat the cycle and be readmitted to the hospital for more diagnostic tests. These subtle forms of factitious disease are much more common in women than in men.
It has been estimated that up to 5% of physician-patient encounters may involve factitious diseases (15). However, some experts believe that factitious diseases are underdiagnosed since these patients are adept at hiding their fraudulent behavior (2). The National Institute of Allergy and Infectious Diseases reported that 9% of cases of fevers of unknown origin or recurrent infections were factitious or self-induced (16). In another study, 3.5% of 3300 specimens submitted as urinary stones were artifacts, such as small pebbles of rock (17). Unfortunately, from this report we were not able to determine the fraction of patients who submitted stones that were artifacts.
Table 1 shows a classification of factitious disorders according to the mechanism by which the disorder was induced or simulated. As evident from this table, people can simulate authentic disease in almost all organ systems and become patients of physicians in almost all medical specialties. The type of illness feigned or produced is limited only by the patient's medical knowledge and creativity (19).
Table 1.
A classification of factitious disorders according to the mechanisms employed, with examples of theresulting symptom-complex∗
| • Self-induced infections: wounds, abscesses, bacteremia, sepsis, fever |
| • Surreptitious ingestion of medicines, vitamins, minerals: diarrhea, vomiting, hypokalemia (laxatives and/or diuretics), renal failure, hypomagnesemia, salt poisoning, Bartter's syndrome, hypoglycemia, pheochromocytoma (epinephrine injection), hyperthyroidism, bleeding or purpura from coagulation disorder (dicumarol, heparin), bone marrow depression, liver disease (vitamin A toxicity) |
| • Self-induced injury: unhealed wounds, bruises, deformities, dermatoses (may also be induced by ingestion of certain drugs), reflex sympathetic dystrophy |
| • Phlebotomy (self or animal): anemia, melena, hematochezia, hematemesis, hematuria |
| • Thermometer manipulation or substitution of thermometer: fever |
| • Simulation of the clinical manifestations of specific diseases or syndromes (sometimes using falsified medical records or contamination of body fluids): cancer, AIDS, cystic fibrosis, pancreatitis, insanity, depression, multiple sclerosis, seizures, pain syndromes, renal stones, proteinuria |
∗Organization was modified from that of Reich and Gottfried (18).
The purpose of this article is to present a clinical experience with subtle forms of factitious disorders at Baylor University Medical Center (BUMC).
FACTITIOUS DIARRHEA DUE TO SURREPTITIOUS INGESTION OF LAXATIVES: A PROTOTYPE OF FACTITIOUS DISORDERS
In 1980, we reported on 27 patients with intractable diarrhea who had been referred to us by other gastroenterologists because the etiology of their chronic diarrhea could not be determined. Many of these patients had hypokalemia, and most were suspected of having an undiscovered neuroendocrine tumor that was causing diarrhea via neuropeptide hormone release. Surreptitious laxative ingestion was discovered in 7 of these 27 patients (26%), and an additional 2 patients (7%) were surreptitiously taking diuretics (20).
The seven patients with surreptitious laxative abuse were women, ranging in age from 25 to 58 years (Table 2). The diagnosis of laxative ingestion was based on alkalinization of the stool or the urine to test for phenolphthalein (which turns the stool or urine pink when the pH is about 9) and on results of a secret search of the patient's personal possessions. Dr. Sam Marynick, who was an intern working with us at the time, did one of the room searches and found laxatives in a hole cut out of a Bible. Dr. Marynick was a good room searcher.
Table 2.
Seven patients with diarrhea due to surreptitious laxative intake∗
| Age | Sex | Duration of diarrhea (y) | BMs per day | Stool weight(g/day) | Laxative |
| 26 | F | 1.5 19 | 993 | Phenolphthalein | |
| 58 | F | 7 | 17 | 2301 | Phenolphthalein |
| 33 | F | 7 | † | 2561 | Anthraquinone‡ |
| 25 | F | 1.5 11 | 391 | Phenolphthalein | |
| 48 | F | 4 | 3 | 427 | Anthraquinone‡ |
| 53 | F | 3 | 8 | 325 | Phenolphthalein and anthraquinone‡ |
| 28 | F | 10 | 11 | 783 | Phenolphthalein and milk of magnesia |
∗From reference 20.
†This patient had had a colectomy
‡Melanosis coli was found on rectal biopsy in the three patients taking anthraquinones. BM indicates bowel movement.
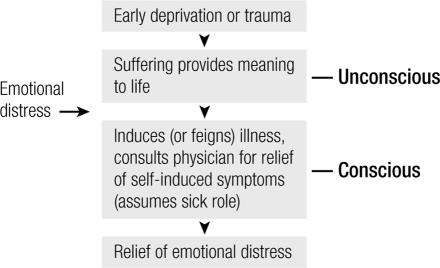
Three of the patients were taking phenolphthalein, two were taking an anthraquinone laxative, and two were taking phenolphthalein plus either an anthraquinone or milk of magnesia. All three of the patients who were taking an anthraquinone had melanosis coli on histological examination of their rectosigmoid biopsies (Figure 1).
Figure 1.
The histologic appearance of melanosis coli, showing pigment-laden macrophages between the crypts in the lamina propria. The pigment is probably lipofuscin released by damaged epithelial cells. This is highly suggestive of long-term anthraquinone use. The effect is reversible within 1 year of discontinuing anthraquinone ingestion. The pigment-laden macrophages may be present histologically even when the endoscopic appearance of mucosa is normal. Hematoxylineosin stain, ×120. Reproduced with permission from reference 21.
Surreptitious laxative ingestion can produce four main symptom complexes: diarrhea, metabolic abnormalities, abdominal pain, and weight loss. Depending on what a patient focuses on, laxative abuse can present as what appears to be a primary gastrointestinal, endocrine, renal, or neoplastic disease.
All the patients shown in Table 2 were studied in the 1960s and 1970s, and this was a time when many new diagnostic tests became available. These included immunoassays for gastrin and vasoactive intestinal polypeptide(VIP), colonoscopy and biopsy, abdominal sonography, and computed tomography (CT) scans. When these tests were applied to patients with chronic diarrhea, they often revealed abnormalities that suggested the presence of neuroendocrine tumors or inflammation of gastrointestinal mucosa. Although it was not well recognized at the time, many of these “abnormalities” actually represented false-positive results (22), which often led to exploratory laparotomy, pancreatic resection, small intestinal or colon resection, or prolonged treatment with corticosteroids (20, 23–27). The result was an epidemic of severe and serious iatrogenic disease. Parenthetically, it is interesting to note that none of our 27 patients had a tumor of any kind, and none ever developed ulcerative colitis, Crohn's disease, or celiac sprue.
For two reasons, it has become much more difficult to diagnose surreptitious laxative abuse in recent years. First, phenolphthalein was removed from the market and was replaced by bisacodyl (28), which is now the active ingredient in over-the-counter laxatives such as Correctol and Ex-Lax and is also available as Dulcolax. Unlike phenolphthalein, bisacodyl does not turn pink upon alkalinization, and there is no other simple laboratory test for this drug. Second, as discussed later in this article, ethical considerations have discouraged use of the secret room search (29), and such a search has become impractical since patients with idiopathic diarrhea are usually no longer admitted to the hospital. Unfortunately, patients continue to abuse laxatives as before, as illustrated by a recent and ongoing case study.
Case study 1: A young woman with diarrhea, hypokalemia, and weight loss
Diarrhea in this patient began a few days after she underwent reconstructive jaw surgery. Extensive evaluations at two institutions failed to reveal a cause of her illness. Approximately 1 year after the onset of diarrhea, the patient was referred to BUMC.
At BUMC, her stool weight measured 1008 grams per day. (Normal stool weight for women is 87 ± 8 g/day.) The diarrhea was secretory in nature without steatorrhea. All previous biopsies, x-rays, and other tests were reviewed, and upper and lower endoscopies were repeated. No abnormalities were found. There was no evidence of melanosis coli, microscopic colitis, or small bowel disease; serum gastrin and VIP concentrations were within normal limits; and stool culture revealed no pathogens. The patient denied ingestion of laxatives, and a urine and stool laxative screen by Toxi-Lab assay was negative. We did not search the patient's personal belongings. She was sent home with advice on symptom management and with an offer to return at any time.
Approximately 2 years after the onset of diarrhea, the patient went to another tertiary medical center. Diagnostic tests were repeated there, but no diagnosis was forthcoming. However, after a colonoscopy she had severe bleeding and required multiple units of blood—showing that these tests can have serious complications. Several months later, her weight had dropped to 108 pounds, and total parenteral nutrition was begun.
After the diarrhea had been present for approximately 3 years, the patient returned to BUMC. By that time, we had shown that the Toxi-Lab assay for laxatives was not accurate. We therefore had her urine analyzed by thin-layer chromatography, and it tested positive for bisacodyl, suggesting that she was taking bisacodyl surreptitiously to induce her diarrhea.
Confrontation
We then had to decide whether or not to confront the patient about our suspected diagnosis. If we confronted her, we also had to decide whether to tell her husband, who was with the patient continuously during her evaluations at BUMC. Some of the benefits of confrontation might include confirming the suspected diagnosis, convincing the patient to stop inducing illness in herself, and avoiding future iatrogenic complications. There are also some downsides to confrontation. Confrontation may ruin the doctor-patient relationship, may harm the patient's marriage, and may not accomplish any of the above-mentioned goals.
The benefits and risks of confrontation have been analyzed by Reich and Gottfried (18), who reviewed 41 cases of various types of factitious disease from a single institution. Thirty-three of the 41 patients were confronted with evidence that their disorders were self-induced. None signed out of the hospital or became suicidal. Although only 13 of the 33 patients acknowledged that their illness was self-induced, most improved after confrontation and 4 became asymptomatic. These findings are in general agreement with our experience with patients who self-induce diarrhea, except that a higher fraction of our patients have left the hospital against our advice and a lower fraction have admitted to fraudulent behavior.
In case 1, we went forward with a “supportive confrontation” (Table 3) (30–32), and we did it in the presence of her husband. With a few tears, she calmly said that she had “absolutely not” been taking laxatives and added, “I don't even know what bisacodyl is.” Her husband was not able to find laxatives in the house, and he believed his wife. The husband later searched her closet and found an empty box of Correctol for Women, which contains bisacodyl. Only then was he convinced. The husband and her local physician agreed to obtain psychiatric help for the patient.
Table 3.
Principles of a supportive confrontation of patients suspected of factitious disease∗
| Basis for this confrontation approach: |
| • Factitious disease represents the patient's attempt to cope with emotional distress (although the patient may not recognize this). |
| • The patient is in desperate need of help. |
| • An understanding and supportive attitude by the staff will make it possible for the patient to cope with and live through the shame and shattered self-image that will result from the confrontation. |
| Procedure: |
| • Let the patient know what you suspect but without outright accusation. |
| • Support the suspicion with facts. |
| • Provide empathetic and face-saving comments such as “Maybe you took it in your sleep,” “What you did was a cry for help, and we understand,” “We realize you must be in great distress,” and “We want to continue to take care of you.” |
| • Avoid probing to uncover the patient's underlying feelings and motivations so as to minimize disruption of emotional defenses that are essential to her function. |
| • Assure the patient that only those who need to know will be informed of the suspicion of factitious disease. |
| • Make sure the staff demonstrate continued acceptance of the patient as a person worthy of their help. The attending physician should not abandon the patient but should continue to show interest and concern. |
| • Encourage psychiatric help, but if the patient resists, do not force the issue. |
Shortly after the patient left Dallas to return home, we spoke with members of her family to try to determine the patient's motivation for surreptitious laxative ingestion. They told us that there was no evidence of an eating disorder or sexual abuse. For the last 6 years, the patient had worked in a doctor's office, where her knowledge of medicine had increased. We were told, “She's always been a great believer in medicine, and she doesn't see the risks. For example, she's had multiple orthopaedic surgeries without any clear need, and the jaw surgery was done for a questionable indication.” These surgeries made the patient the center of attention. “She's married to a loving and caring husband but is unable to have children. The diarrheal illness started about 3 months after her diagnosis of infertility.” Parenthetically, it is interesting to note that factitious disease often begins shortly after a stressful event (32, 33).
The family and some of her local physicians were contacted again in 2005 to get an update on the patient's condition. Generally things were much better for the entire family. It was a wise decision to confront the patient. However, the patient felt betrayed. She never accepted the diagnosis, and she would never see a psychiatrist. She still has various medical problems almost constantly, with frequent appointments with specialists. She remains fascinated with illness but is less dramatic about it and receives less attention from it. Two weeks prior to the phone call, the patient had had hip surgery, and in June 2005 she had had a cholecystectomy. Earlier in the year she had had surgery to correct damage caused by teeth grinding. We were told that she's probably not taking laxatives anymore, but several times a year her serum potassium level is low. On one occasion, a diuretic was found in her urine. Based on this information, it seems clear that our patient has not been cured of her disease and that her fascination with medicine, her polysurgical addiction (6), and her compulsion to assume the sick role continue.
A difficult and usually delayed diagnosis
For the patients reported in Table 2, it took a long time for the factitious nature of their disease to be diagnosed—from 1.5 to 10 years. In the case just presented, the delay was 3 years. Why is it so difficult for doctors to recognize factitious disease?
First, patients with subtle forms of factitious disease don't appear different from other patients with similar symptoms caused by authentic disease (20, 26, 34, 35), and the psychiatric abnormalities they have are not recognized by their doctors (36). Stated another way, there is no obvious excessive secondary gain that the patients are seeking. Second, most physicians and nurses rarely consider factitious disease in the differential diagnosis (35). Negative tests for authentic diseases are considered false-negatives, so the tests are repeated—as was done at BUMC and at multiple other medical centers in our first case study—and new doctors are consulted who repeat the diagnostic cycle. Third, the patients convincingly deny self-induced illness if they're asked (23). Fourth, there's a lack of communication between outpatient and inpatient doctors, as well as a failure to study old medical records. Finally, as discussed at the end of this article, psychiatric consultation is usually of no help in establishing or ruling out a diagnosis of factitious disease.
Clues that should suggest factitious disease
Despite the difficulty in diagnosis, several important clues should lead physicians to suspect factitious disease (15, 23, 24, 26, 36–39). Most people with factitious disease are women (except in Munchausen's syndrome, in which most patients are men). Many have been employed in the health care field and therefore have an unusual grasp of medical terminology. Typically they have had numerous previous surgeries, and they have the resulting surgical scars. It helps to count the number of surgical procedures and to review the pathology reports for evidence of authentic disease or lack thereof. These patients often lack appropriate concern about their health problems; they tolerate their intractable illness with equanimity and are unrealistically cooperative. They endure the discomfort of diagnostic procedures and surgery without complaint. They are also very good mimics and actors, and they may have a past history of feigning illness (if past medical records are consulted).
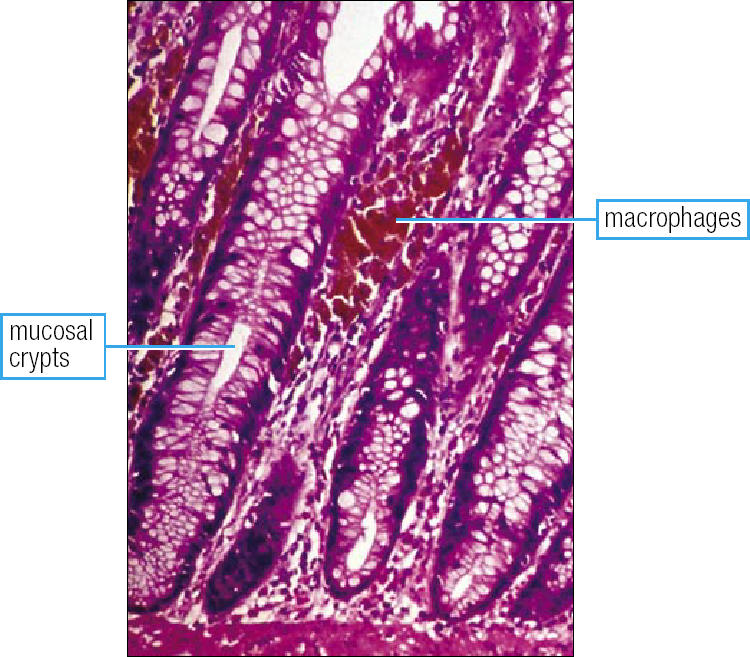
Pathogenesis of factitious disease
Psychiatrists have studied a small number of patients with various factitious diseases and have proposed the model that is depicted in Figure 2. The theory comprises an unconscious motivation and a conscious fraudulent act (11, 14). The unconscious motivation is believed to result from some early deprivation or trauma, from which the patient subconsciously learns that suffering and illness provide relief from emotional discomfort and give meaning to life (11). Later in life, at times of emotional distress, the patient feigns or induces illness so as to assume the sick role. She then establishes a relationship with doctors, nurses, and other health professionals, with the ostensible purpose of obtaining relief from the very symptoms she is either inducing or feigning. This provides the patient with a unique identity as a professional patient (11). It is proposed that by focusing on a physical illness, the patient avoids underlying painful emotions (33). There is no apparent symbolic significance to the selection of the illness that is induced or feigned, and different symptoms and diseases have been used by a patient at different times (40).
Figure 2.
Proposed pathogenesis for factitious disease. Adapted from references 11 and 14.
This proposed pathogenic model has some important limitations and implications. First, neither the patient nor her physicians ever learn anything about the early deprivation/ trauma that presumably initiated the illness-seeking behavior. We never learn, and the patient presumably doesn't know, what deep secrets are being protected by the factitious disease (11). Second, attributing the basic motive to the unconscious reduces the blame that can be placed on the patient (11). If physicians accept the notion of a strong unconscious compulsion, they are less likely to stand in judgment of the patient's self-destructive and fraudulent behavior. It can be argued that, as sick people with an abnormal psyche, these patients deserve the same consideration as patients with other psychiatric disorders (40).
Regardless of the validity of the pathogenic hypothesis shown in Figure 2, it is generally believed that patients with factitious disease are fully aware of what they are doing and that they know right from wrong. They only rarely have features of a major mental disorder, in spite of their bizarre behavior (18). Their IQ is usually normal or high, and only a very few are psychotic. Some are depressed and some may have thoughts of suicide (11, 26, 33, 37, 39, 41). As a group, they are sometimes described as being immature, sexually inhibited, and lacking in interpersonal skills. These patients usually refuse to see or work with a psychiatrist, and they typically resist all efforts to get to the bottom of their apparently unconscious motivation. Sutherland and Rodin wrote in 1990 that there have been no systematic evaluations regarding the efficacy of psychiatric intervention in patients with factitious disease (42). As far as we are aware, this statement remains valid in 2006.
The main tangible emotional gains that patients receive from assuming the sick role are believed to be sympathy, warmth, and nurturance; a heroic image for tolerating illness so bravely; relief from an expected achiever role; and control over their lives (11, 23). Kind, tolerant, and empathetic doctors and nurses provide a natural haven for patients with such needs (43).
The distinction between factitious disease, which we are discussing here, and some related disorders is depicted in Table 4. Although these distinctions are perfectly clear as written, in our opinion the line separating them in clinical practice can be extremely thin.
Table 4.
Factitious disease and related disorders: some definitions and distinctions∗
| • Factitious disease: Conscious and intentional feigning or production of symptoms, due to a psychological need to assume the sick role in order to obtain emotional gain. |
| • Malingering: The conscious and intentional production or exaggeration of symptoms for material gain, such as money, lodging, food, drugs, avoidance of military service, or escape from punishment. |
| • Somatization: Recurrent and multiple symptoms (pain, gastrointestinal, sexual, pseudoneurological) that have no organic basis, believed to be due to unconscious expressions of suppressed emotional conflict or stress. Unlike in factitious disease, the symptoms are not created by voluntary conscious behavior. |
| • Hypochondriasis: Obsession with fears that one has a serious, undiagnosed disease, presumably based on misinterpretation of bodily sensations. |
Effects on the physician-patient relationship and the need for an accurate diagnosis
The traditional doctor-patient relationship is a cooperative and complementary partnership in which the patient and physician respectively fulfill their obligations and privileges, as prescribed by society. The doctor must act on behalf or in the best interest of the patient's welfare, including curing the patient whenever possible, not harming the patient, and maintaining the patient's confidence (46, 47).
The patient's role consists of three basic features. First, it is not the sick person's fault that he or she became ill. Second, patients are excused from their “ordinary daily obligations and expectations.” Finally, patients must make every attempt to regain health, including a requirement to “faithfully and unreservedly communicate to their physician the supposed cause of their disease” (46, 48–50).
The physician-patient relationship is based on trust that each will act according to their established roles. The patient's medical history directs diagnostic studies and medical and surgical therapy. However, in factitious disorders the sick role is attained via fraudulent means, and the patient intentionally deceives the physician by presenting false medical data and history and by withholding information regarding the cause of the disease. Of course, the physician does not suspect or know this. As a result, unneeded and inappropriate diagnostic tests and therapies are prescribed and willingly accepted by the patient, and these may, in turn, result in iatrogenic disease. Thus, “the factitious disease patient's partner in illness is the doctor. The greatest damage to these patients is due to doctors' actions, rather than from any direct action by the patient” (43).
This analysis emphasizes the importance of recognizing patients with factitious disease so that medical mistakes and iatrogenic disease are avoided. In addition, the costs of factitious disease are enormous, and they are all paid for by society (2, 15, 51). As Dr. Herb Leiman has pointed out, the facilitator of factitious disease is good medical insurance.
SURREPTITIOUS LAXATIVE INGESTION FOR WEIGHT CONTROL
Case study 2: A young woman with weight loss, diarrhea, nausea, and vomiting
This patient was referred to BUMC following extensive gastrointestinal evaluations at two other medical centers, neither of which revealed the cause of her symptoms. On admission her serum potassium concentration was 2.2 mEq/L, her blood urea nitrogen level was 40 mg/dL, and her creatinine level was 2.0 mg/dL. Stool examination revealed severe secretory diarrhea, and the alkalinization test for phenolphthalein was strongly positive.
When the patient was confronted with the discovery of phenolphthalein in her stool, she readily admitted that she had been ingesting Correctol. One of the residents on this case, Dr. Michael Carmichael, then conducted an interview that was videotaped. It contained the following questions and responses:
Patient: When I first went into the hospital and had tests run, they found nothing at all.
Doctor: Okay. Were you taking any medicines at that time?
Patient: No medicines, no.
Doctor: Were you taking laxatives at that time?
Patient: Yes.
Doctor: Okay. What happened after that, after you left the hospital?
Patient: I was better for a while and then I got worse a few months later and went into another hospital and had the same tests done again. The only thing they found was that I had gastritis.
Doctor: And yet, the doctors in these hospitals did quite a few tests on you, and even some tests that I'm sure were painful and expensive and a lot of trouble for you. Did you think about that? I'm curious about what you thought about all of that.
Patient: I really thought, tried to tell myself that there must be something else wrong.
Doctor: Did the doctors ever ask you at that time about laxatives and if you were taking them?
Patient: No.
Doctor: If the doctors had told you that you needed an operation, say, to find out what was wrong with you, what do you think your reaction would have been to that?
Patient: I believe I would have gone along with whatever they said.
Doctor: Why?
Patient: I really don't know.
Doctor: Can you tell us a little more about taking the laxatives and specifically why you picked laxatives as opposed to something else?
Patient: I felt that I could eat anything I wanted to and for the first time not have to worry about what I ate and still not gain any weight.
Doctor: So it was to keep your weight down.
Patient: Right.
Doctor: Okay. You were taking Correctol, I think. Isn't that correct?
Patient: Yes.
Doctor: How many did you take, would you say, in a day's time on average?
Patient: At the worst time, I guess about 40 a day.
Doctor: Forty tablets a day. That's a lot of tablets.
Patient: Yes.
Doctor: How did you feel when we told you that we thought the problem with the weight loss was because you were taking laxatives? What did you think when we brought this up?
Patient: I was so relieved. I've never felt that relieved in my life. I wanted somebody to know, but I couldn't bring myself to tell anyone.
In other parts of the interview, the patient said she had been overweight from the ages of 7 to 14. She was teased, became self-conscious, and developed a negative self-image. At that point, she went on a starvation diet and controlled her weight. However, when she gained about 5 pounds in her 20s, she turned to laxatives as a way to eat what she wanted. The patient reported loving food but feeling that she couldn't have it without weight gain.
Following withdrawal of the laxatives, the patient became edematous and gained weight, which was extremely disturbing to her. However, within about 1 week she began to mobilize her edema and her weight fell. She willingly accepted psychotherapy by Dr. Jake Peden, chief of psychiatry at BUMC.
Laxative abuse in patients with bulimia
This patient had a variant of anorexia nervosa, and she attempted to control her weight with laxatives. This is called “bulimia” or “bulimia nervosa.” The dictionary definition of bulimia is an abnormal increase in the sensation of hunger (limos = hunger) (52). The rationale for using laxatives is that the resulting purge reduces the absorption of recently ingested calories (35). Dr. George Bolin contacted 10 Dallas health food stores and found that nine of them recommended laxatives for weight control (53). Typically, patients take the laxatives about five times per week after food binges, but some patients use laxatives daily.
Patients who use laxatives to control their weight feel guilty about this practice and try to keep it a secret, but they do not deny laxative abuse when they are directly asked (35). Many such patients develop an apparent craving for laxatives (54). When they stop taking laxatives, they often retain excess body fluid for a period of time (35, 55). Although these patients usually have serious psychiatric problems, most of them lead outwardly normal lives. In several cases, like in our patient, they repeatedly consult doctors for their laxative-induced symptoms but don't tell the doctors that they are taking laxatives. Our patient seemed to believe that something other than laxatives was causing her symptoms, and she wanted her doctors to look hard to find the other cause. If the doctors knew she was taking laxatives, they would be biased and would not search thoroughly for other causes. Most alarmingly, she would have been willing to undergo any test or have any surgical procedure that a doctor suggested. Unlike in case 1, iatrogenic disease in case 2 could have easily been prevented by just asking the patient if she took laxatives.
Effect of purging on caloric absorption
Our patient participated in a research study to determine the degree to which purging with Correctol reduced absorption of ingested dietary calories. The calories in her food and in her stool were measured by bomb calorimetry. During a control study, without Correctol, she ingested 1611 calories per day, and she absorbed 1466 of those calories. When she ingested 50 Correctol tablets with her meals, she developed severe diarrhea, and absorption of her ingested food calories was reduced to 1278 calories (53). Thus, the severe laxative-induced diarrhea caused caloric absorption to be reduced by only 188 calories, less than the calories in two small bananas or in one 35-gram candy bar. Although the reduction in caloric absorption was relatively trivial, the 50 tablets of Correctol did cause acute weight loss due to watery diarrhea. In fact, she put out 6.1 liters of stool, which weighed 13.6 pounds (53).
In both case 1 and case 2, ingestion of laxatives was associated with severe chronic weight loss, and yet ingestion of laxatives has only a trivial effect on absorption of recently ingested calories. We believe that laxative abuse causes weight loss by making patients extremely ill, with volume depletion, abdominal pain, diarrhea, nausea, and sometimes vomiting. With this chronic self-induced illness and its symptoms, the patients are probably not able to eat normally, and most of their nonfluid weight loss is most likely due to reduced food intake.
The role of laxatives in the case of Karen Carpenter
People magazine published an article about Karen Carpenter's battle against anorexia nervosa and the role that laxatives played (56). At the time of her death, she had been suffering from anorexia for 8 years—apparently since reading a passing reference to her chubbiness in a newspaper.
The magazine reported: “Distraught she reached out to Pat Boone's daughter, Cherry. ‘Karen was having particular problems with laxatives. She could not believe she could ever get to the point where she was not dependent on them.’ Cherry herself had often taken laxatives by the box to ‘drop 10 or 15 pounds overnight’” (56).
POTENTIALLY LETHAL FORMS OF FACTITIOUS DISEASE
Case study 3: A young woman with bacteremia
This patient was referred to BUMC for evaluation of recurrent urinary tract infections and bacteremia, mainly due to Escherichia coli and Staphylococcus aureus. Her central lines were complicated by bilateral subclavian thrombosis and tension pneumothorax. She also had a skin disorder with blisters. An extensive workup showed no evidence of immunocompromise, no source of sepsis, and a completely normal genitourinary tract. Her past history included cesarean section, hysterectomy, and hypertension. She was employed as a medical technologist and was married, with two children. She had no history of narcotic abuse.
Based on these clinical and social features, one of the several doctors on this case suspected that the patient was inducing her own illness, and he decided to secretly search her personal possessions. This is always done with trepidation. In this case, the upside would be discovery of materials that indicate self-induced disease, which would provide an explanation for her recurrent septicemia. The downside is that the doctor may find nothing unusual. In such instances there will be feelings of guilt, assuaged only by the hope that the patient will not know that the search took place and that his intentions were honorable. It's not a comfortable feeling.
While the patient was having an x-ray, her room was searched. Her purse contained a Petri dish with growing bacterial colonies, as well as needles, a syringe, and a tourniquet. The colonies were subcultured and the Petri dish replaced. Later that day, the patient was asked whether she might be harming herself by injection. She denied this, saying that she wanted to get better. Still later that day, the doctor told the patient that he knew she had some incriminating items in her purse. She then opened her purse so the doctor could see inside, and the items were apparently no longer present. To prove her point, the patient turned her purse upside down. At that point, one needle and a syringe fell out, which she had apparently overlooked when she returned from her x-ray and suspected that someone had searched her purse. The patient was upset about the room search but not visibly angry. She readily agreed to see a psychiatrist but continued to deny self-injection.
The next day, the patient tearfully confessed that she had had bacteriological materials in her purse, but she said she used them only to aspirate and culture some blisters on her skin. She still denied self-injection with bacteria and said she wanted the doctors to “keep looking for the cause of my problems.”
Ethical conflicts in case 3
A secret room search confirmed the doctor's suspicion of self-induced septicemia and may have saved the patient's life. Evidence in support of this last assertion is twofold. First, similar patients have died as a result of self-induced injection of bacterial cultures (18). And second, even when patients with self-induced bacteremia deny self-injection when they are confronted with evidence obtained from a room search, the confrontation often causes them to stop this practice. Thus, in case 3, there were good reasons to believe that a room search and a subsequent confrontation were in the patient's best interest. However, for two related reasons, it seems unlikely that such a search will be carried out in the future in our hospital, even if we are faced with a patient whom we suspect is inducing a disease that is likely to be fatal. First, there are ethical and legal objections to a secret search of a patient's personal possessions (29), and these are briefly summarized in Table 5. The second and more compelling reason is that our hospital has, in essence, promised that we will not do it. This “promise” is given to each patient admitted to BUMC, in a document entitled To Our Patients: Your Rights and Responsibilities (57). The patients' rights include the following:
Your doctor should tell you about any proposed procedures, and before procedures are performed, you will be asked for informed consent (p. 3).
You have the right to privacy … and confidentiality (p. 5).
Table 5.
Ethical and legal arguments against a secret search of patients' possessions to look for evidence of factitious disease∗
| Ethical issues: |
| • The patient has a right to self-determination. |
| • The patient has the right to be informed and to approve or disapprove of any diagnostic procedure. |
| • Ordering unnecessary tests as a ruse to get the patient out of the hospital room is repugnant. |
| Legal issues: |
| • The patient's right to control her destiny supersedes society's interest in preserving her life. |
| • A search is beyond the bounds of the implied contract between the doctor and the patient. |
| Privacy issues: |
| • A purse or suitcase is something meant to be private. It might be acceptable to search a hospital nightstand but not the patient's purse. |
∗From reference 29.
The document also lists the patient's responsibilities, including the following:
Give complete and accurate information about your medical history, including past medical problems and all medications you take (p. 7).
You may take only the medications given to you by authorized medical center employees (p. 7).
Even though factitious disease patients don't play by the rules of being a patient, doctors at BUMC must play by the rules our hospital and medical board have promised we will obey. In cases of possible factitious diarrhea, obeying these rules does not create a major problem, because factitious diarrhea is rarely lethal, and stool and urine tests can be done to help make a diagnosis. But what should we do with a patient suspected of factitious septicemia or some other factitious disease that is even more life-threatening?
One possibility is for the doctor to tell the patient of his or her suspicions and to ask for informed consent to perform a search of the patient's personal possessions (29, 58). This would require planning, including preparation of a specific informed consent document for the search procedure. The patient would be told that the search is necessary before further invasive diagnostic tests are done. If the patient agrees to the search, and if it reveals evidence of factitious disease, the suspicion would be confirmed. If the patient does not allow a search, the referring doctor (and possibly the patient's family) could be advised about the likely implications, in hopes that this knowledge would reduce the likelihood of future harmful effects of a putative self-induced disease. If the search reveals nothing, or if the patient refuses to allow the search, the physician might feel compelled to withdraw from the case, provided another doctor can be found who will assume responsibility for the patient.
Treating a search of a patient's belongings just like any other medical procedure sounds simple enough and has been recommended (29, 58), but in practice it might be extremely difficult. Still, it is an alternative to sitting by, suspecting that a patient may be intentionally killing herself by an induced illness. Unfortunately, we know of no reports describing the results and effects of asking patients for consent to search their personal belongings.
The ethical and legal dilemmas related to disclosures of medical information about a patient with factitious disease to other doctors and family members, in order to hopefully protect the patient from self-induced injury, have been well discussed by Kass (12). Physicians who intend to disclose the factitious nature of a patient's disease to another doctor or to a family member should so inform the patient.
FEIGNING CANCER WITH THE HELP OF FABRICATED MEDICAL RECORDS
Case study 4: A young woman seeking chemotherapy
A young woman provided the following medical history to a BUMC oncologist. She said she had recently returned to Texas from another state where she had undergone treatment for a carcinoma of the small intestine. This was discovered after an episode of small bowel obstruction, when a CT scan revealed a grapefruit-sized mass in her abdomen. She was treated with fluorouracil and leucovorin and then had surgery to resect the mass. The patient was now seeking a Dallas oncologist to continue her chemotherapy.
Her reported social history included the following. She was adopted, with no known biological relatives. She had smoked cigarettes since age 13, she was married and had one child, and she worked as a licensed vocational nurse in a nursing home.
On physical examination, the patient appeared to be in good health. Her body mass index was 24.5. There were surgical scars on the abdomen. She had alopecia that was attributed to recent chemotherapy. The physical examination revealed no other abnormalities. Results of a complete blood count were normal. The oncologist's plan was to obtain her outside records and pathology slides for review and then resume the patient's chemotherapy.
Shortly thereafter the patient gave the oncologist a surgical pathology report from an out-of-state hospital. The report described a resected portion of small intestine which was obstructed due to a tumor. On histological examination the tumor consisted of “heterogenty [sic] cells and a large cell lymphoma. There were also adenocarcinomas, in Stage III.” In addition to these medical improbabilities and the unusual terminology, the typing on the report appeared to have been altered, with alignment errors. Moreover, on parts of the report it appeared as though the name of the patient and the attending physician had been altered by pasting and photocopying. The oncologist believed that the report was fabricated. No legitimate-appearing medical records were ever received.
The patient never returned to see the oncologist. However, she gave his name to other doctors she subsequently visited, indicating he was an oncologist who had previously treated her for cancer. Therefore, the oncologist received telephone calls and medical records from some of her subsequent visits with other doctors, providing a probably partial trail of her continuing effort to pose as a cancer patient. In one instance she was admitted to an out-of-state hospital because of abdominal and flank pain. The patient gave a history of active ovarian cancer. An intensive series of studies were carried out, all of which were normal. A psychiatrist examined the patient and thought that she most likely had an organic etiology of her pain. In his opinion the patient's mental status was appropriate.
Records from an emergency department visit at BUMC were received by the out-of-state hospital. That note stated that the patient had been seen in BUMC's emergency department, at which time she was complaining of right flank pain and a history of urinary calculi. It further stated that the patient was well known to the hospital staff as an individual who had no documentable urological disease and that the surgical scars on the patient's abdomen were a consequence of a motor vehicle accident rather than from cancer surgery. Being unable to document a history of ovarian cancer or a urological abnormality, it was suspected that the patient had no organic disease but was presenting a fraudulent history. A representative of “her insurance company” stated that she had not been insured with them for almost a year. Her husband was also contacted, and he stated that he received calls from various hospitals at least monthly inquiring about the insurance status of his wife. When the patient was confronted with this information, she left the hospital against medical advice.
Two years later the patient was admitted to another Texas hospital with fever and pain in the right flank. In this visit, the patient's history included a right ureteral stent and cancer of the colon. She was placed on intravenous antibiotics, and she continued to complain of pain requiring multiple doses of Demerol. A plain film of the kidneys, ureters, and bladder and an ultrasound revealed a stent in the patient's upper ureter. After 48 hours of antibiotics and pain medications, the physician considered a stent removal and change. He called a urologist in Dallas who had supposedly inserted the stent a month earlier and discovered that the patient had given him a “name of an oncologist who was nonexistent.” When the physician confronted the patient, she stated that she was having marital problems and that was the reason for her admission. The physician discharged her to return to Dallas for follow-up and to seek psychological counseling.
One year later, the patient was hospitalized for pain at still another Texas hospital. The physician treating her called the BUMC oncologist asking for her background information. The physician told the oncologist that he “could find absolutely nothing wrong with her.”
Six years later, the patient was seen by a different BUMC physician who specializes in gynecological oncology. The patient provided the following medical history. She was diagnosed with ovarian cancer in 1991. She was initially managed in another Texas city where she underwent laparoscopy, followed by total abdominal hysterectomy and bilateral salpingo-oophorectomy with colon resection and colostomy. She went to M. D. Anderson Hospital where she was treated with radiation and chemotherapy, which was followed by a negative second-look laparotomy and colostomy closure. At about that time she developed a ureteral stricture and underwent placement of a stent and later required a percutaneous nephrostomy. Her weight was 178 pounds, and the physical examination (including pelvic exam) was normal. The physician's impression was “history of advanced recurrent ovarian carcinoma status post chemotherapy followed by negative second look laparotomy.” The plan was to obtain her records from M. D. Anderson Hospital, which apparently never arrived.
Previous reports of factitious cancer
We did a PubMed search for factitious cancer and found 81 articles. Some of the case reports were remarkably similar to our case 4. Patients feigning cancer often enter a new institution seeking to continue treatment for their “cancer,” claiming they were referred by doctors in another city or state. They provide a convincing history, have scars compatible with previous surgical treatment for cancer, and often provide a pathology report. They claim that their other medical records will be sent shortly. A physical examination and laboratory studies are done, and the patient is scheduled to return as soon as the other medical records are received.
Alternatively, or in addition, some patients feign cancer and gain entrance into cancer support groups. One such patient participated in classes on death and dying. The class was so moved by her courage that it raised money for her to ride in a hot air balloon, one of her “final wishes” (59).
Several motivations apparently cause people to feign cancer. One is secondary material gain (malingering, perhaps to obtain narcotics). A second is an unconscious need to deceive the medical system and be subjected to diagnostic tests and therapeutic procedures. Third, some may seek the social status associated with the diagnosis of cancer and take advantage of displays of sympathy and gifts from friends, coworkers, and others (59). Fourth, some people apparently feign cancer because someone they loved had cancer. Finally, one woman later stated that she was hoping to die as a result of immunosuppression (19). Of course, several of these motives may be present simultaneously in a person who feigns cancer.
Whatever the motivation, the onset of feigned cancer seems to commonly occur after rejection by a loved one or after some other type of loss. Loneliness and isolation apparently are the precipitating factors in many people who feign cancer.
Perhaps more than any other groups of physicians, doctors who specialize in cancer treatment carefully examine previous medical records. Therefore, fabrication of medical records is usually required before a patient with factitious cancer would be accepted for chemotherapy by an oncologist or for elective cancer surgery by a surgical oncologist. Patients may steal and alter authentic records from other patients' medical charts and pass them off as their own (59). In one case a patient went to the extent of electronically scanning records and modifying them, making it even more difficult to recognize their fraudulence (19). Gaining access to pathology reports, medical terminology, diagnostic and treatment plans, and symptomatology would be easiest for hospital employees, probably explaining why the best and most complete forgeries are from people who work in hospitals. In spite of the efforts of oncologists to carefully review medical records, fabrications have been good enough in some cases to allow people to obtain chemotherapy (19).
Diagnosis of factitious cancer is usually made by detection of inconsistencies in the medical history, by evidence of fabrication of medical records, by lies patients tell about their health insurance, or by doctors who fortuitously begin to doubt the patient's story. A story of prolonged survival with a usually lethal cancer has helped reveal factitious cancer in some cases. It is likely that many cases of factitious cancer are never discovered, and with advances in computer technology the quality of forged medical records will probably improve in the future.
LEGAL ACTIONS RELATED TO FACTITIOUS DISEASE
We conducted a literature search to determine what lawsuits have been filed by patients with factitious disease. No lawsuits were found related to invasion of privacy, breach of confidentiality, or failure to obtain informed consent. However, there were cases related to failure to diagnose factitious disease, resulting in iatrogenic disease (e.g., complications of chemotherapy after the patient feigned cancer; amputation of a leg in a patient feigning reflex sympathetic dystrophy) (51, 60). One of the arguments plaintiffs have used against their doctors is that strong evidence of the factitious etiology of their disease was present in the medical records, but the doctor did not carefully read those records. It has therefore been concluded that factitious disease is not a reliable defense against a bad outcome (61). In other words, fraudulent conduct by a patient does not dissolve the legal and ethical aspects of the physician-patient relationship (12). This reemphasizes the need for physicians to learn how to recognize and manage patients with factitious disease.
In Arizona, health care providers successfully sued a patient with factitious disease. This patient kept getting care, claiming she had insurance. She then impersonated an insurance representative in an effort to convince providers of her insurance coverage. When she didn't have insurance, the hospital did not get paid and then sued. The woman was found guilty and was assessed 1000 hours of community service and a fine of $106,997—which, according to the records, would take her about 178 years to pay off (58, 62). Some people think there ought to be more of this type of action, which is now legal in North Carolina and Arizona (62).
FACTITIOUS DISEASE INDUCED IN ANOTHER PERSON
Case study 5: An 18-year-old man with symptoms of intestinal pseudo-obstruction
An 18-year-old man with modest mental retardation was admitted to BUMC. Until age 15, the patient had attended school for the disabled and participated in Boy Scouts. He then developed nausea, vomiting, diarrhea, and difficulty urinating. A diagnosis of intestinal pseudo-obstruction (63) was made because he apparently had motility derangements of both the intestine and urinary system. Upon arrival at BUMC, the patient was bedridden, was receiving total parenteral nutrition, and needed bladder catheterization three times a day. However, in the opinion of BUMC radiologists, the accompanying x-rays showed no objective evidence of intestinal pseudo-obstruction or hypomotility of the urinary system. Laxative and toxicology screening tests were negative, but high-performance liquid chromatography revealed emetine in the urine and stool.
The patient had a “devoted mother” who stayed with him almost constantly. She denied giving emetine to her son. By court order, the mother was limited to a 1-hour visitation per day. Within 1 week, the patient was out of bed, walking, and eating and urinating normally. He was discharged to a foster home, and 6 months later he was doing well.
It was our conclusion that the patient's mother was giving the patient ipecac, which is sold over the counter in 30-cc bottles. The two main alkaloid components of ipecac are emetine, which is responsible for muscular and cardiac toxicity, and cepheline, which causes vomiting (64). Repeated doses may decrease the ability of ipecac to induce vomiting, which would lead to further absorption of the ingested drug and therefore more of the cardiac and muscular toxicity. Excretion of absorbed emetine is slow, so accumulation is likely with repeated doses. This BUMC case study was published in 1989 (65). It is an example of Munchausen syndrome by proxy, the background of which is discussed in the next section.
Munchausen syndrome by proxy
In 1977, Meadow, a pediatrician, called attention to a previously neglected form of child abuse and named it Munchausen syndrome by proxy (66). Attaching this term to child abuse had enormous legal ramifications. With the catchy name, it has been relatively easy to educate lawyers, judges, and health care workers about mothers who abuse their children by inducing illness in them. If a doctor or hospital representative goes to a judge with a suspected case of Munchausen syndrome by proxy, the judge will promptly order separation of the child from the mother to see if the child's illness improves in the absence of the mother (confirming the suspicion) and to protect the child from possible additional harm by the mother. There is an ongoing battle between mothers who believe that they have been wrongly accused of child abuse vs pediatricians and pediatric hospitals that regard Munchausen syndrome by proxy as a form of child abuse that is often overlooked and needs to be aggressively detected (43, 51, 67). This is well illustrated by recent events involving Sir Roy Meadow himself, who was judged to have given erroneous testimony in the trial of a mother who was jailed for supposedly smothering her two baby sons (68, 69).
Munchausen syndrome by proxy provides several secondary gains to the mother. She flourishes in the hospital environment and thrives on the accolades she receives as a devoted parent (66, 70). The child's illness may lead to a closer relationship between the mother and her husband (66, 70, 71). The abusers are usually not psychotic, and almost all meet the legal definition of sanity (61, 72). In most cases no psychopathology is evident during psychiatric examination(67, 73). Thus, the child's illness is the only notable symptom of the mother's disorder (73).
Some clues to Munchausen syndrome by proxy are as follows (43, 66, 70–74):
The child's apparent disease is extremely rare.
Numerous doctors are unable to make a diagnosis; experienced physicians have never seen a similar case.
The mother is less worried than the medical team and lifts their spirits after each unsuccessful attempt to make a diagnosis.
There may be a history of factitious disease or somatization in the mother.
A sibling may have a similar illness or may have died from a similar illness.
The father is usually detached and not involved in the care of the sick child.
Several strategies can be used to detect Munchausen syndrome by proxy (43, 51, 66, 75). If appropriate, the child can be directly asked what medications the mother has given. In our case study, the young man was mentally impaired, and we didn't ask him. The physicians can also inquire about the mother's medical and emotional history, to see if she has any evidence of previous factitious disease. The medical records can be examined to see if a temporal relationship exists between the illness and the presence of the parent. The child can be constantly observed in the hospital—either by the nurses in an intensive care unit or by a hidden video camera. Court orders are not required for hidden video cameras when they are placed by medical personnel, even though they are required if placed by the police (51). A secret search of the mother's possessions is acceptable when this disorder is suspected, because a third party may be injured and because the child is the patient and not the mother.
When this syndrome is suspected, it must be reported, even when there is no objective evidence that the mother is abusing the child (51). Court decisions against a mother for this form of child abuse are often made on circumstantial evidence.
KEEPING FACTITIOUS DISEASE IN PERSPECTIVE
Case study 6: A 31-year-old man with postprandial abdominal pain and weight loss
When this young man was admitted to BUMC, his past medical history as well as physical examination, upper endoscopy, colonoscopy, CT scan, sonography, and endoscopic retro-grade cholangiopancreatography provided no clues to his illness. Although he had a small benign gastric ulcer, his symptoms did not respond to potent antiulcer medications, so it was thought that the ulcer was not the cause of his pain. In addition, ulcer pain is usually relieved by eating food, whereas food provoked pain in this patient.
On June 2, the patient had a psychiatric consultation. The psychiatrist noted major depression with melancholia, recurrent type, with somatization, and an amphetamine was prescribed. The drug seemed to help, as the patient's spirits were better the following day.
On June 5, the patient was having severe abdominal pain. Still, his abdomen was soft and bowel sounds were normal, so there was no evidence of an acute abdomen. Demerol was given. Three days later, the patient continued to have pain after meals. The progress notes state: “Pattern of complaints and his response to antidepressant are indicative of psychogenic pain problem coupled with dependent/oppositional personality disorder” and “Patient continues to be quite regressed. He makes the most secondary gain of each and every somatic concern.”
By June 12, the patient lay in the fetal position with his severe abdominal pain. He was noted to have periumbilical tenderness but no rebound tenderness and to be severely depressed. The progress notes add: “His mom and friends hovering over him. He does seem depressed but the pain syndrome seems psychogenic in origin (not a depressive equivalent) and secondary to his dependent narcissistic personality structure.”
On June 15, a feeding tube was placed, and he was transferred to the psychiatry unit. Later he was found unresponsive. An x-ray showed free air under the diaphragm, and the patient died a short time later.
Lessons learned from case 6
While the patient was alive, no authentic physical disease was identified to explain his severe pain and weight loss. This led his doctors to make a diagnosis of “psychogenic pain,” implying that his pain was primarily caused and maintained by psychological distress (44). However, even though the patient was only 31 years old, an autopsy showed that his superior mesenteric artery was completely occluded by atherosclerosis and that he had ischemic necrosis of his small intestine (Figure 3). In retrospect, the patient's abdominal pain was due to abdominal angina. Patients with abdominal angina experience severe pain after meals, and food is avoided in order to reduce pain, resulting in weight loss. As the disease advances, the pain may become continuous, rather than only after meals, and this indicates the onset of intestinal infarction. Abnormalities on physical examination are mild in comparison with the severe pain. Presumably because his illness could not be diagnosed or treated and because of the severe pain, the patient developed depression and the other psychiatric abnormalities described by the psychiatrist.
Figure 3.
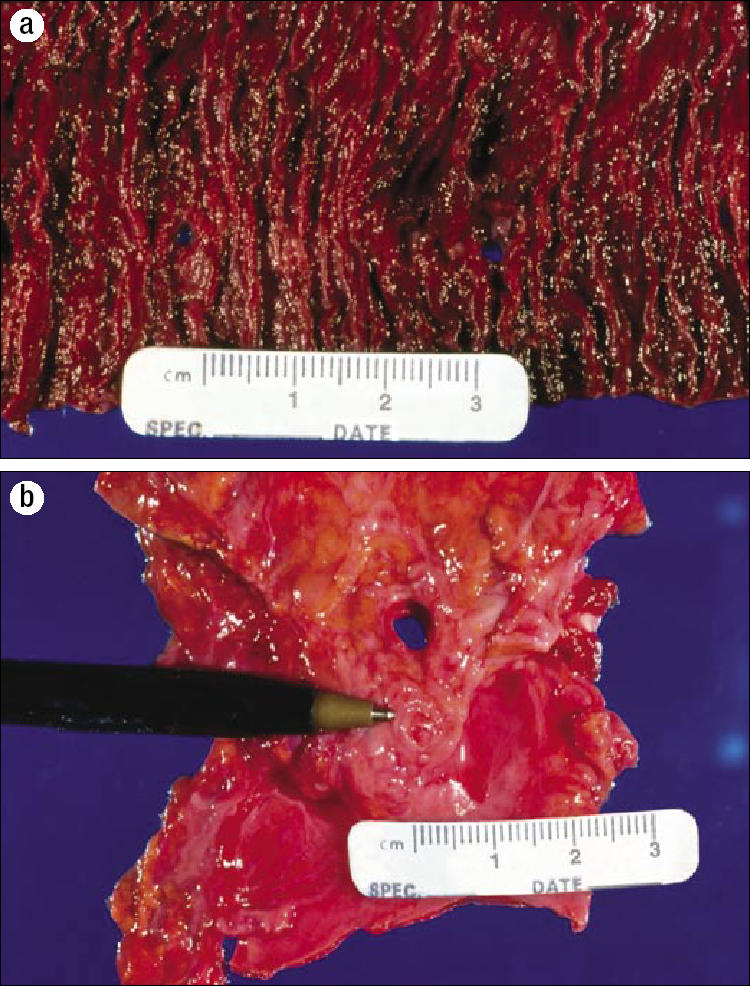
Mesenteric artery occlusion caused by extensive atherosclerosis. (a) The mucosal surface of a segment of jejunum showing ischemic necrosis and two small perforations. (b) Anterior external aspect of the aorta showing takeoff of patent celiac artery (top) and totally occluded superior mesenteric artery (tip of the pen), located 1 cm below the celiac artery.
It has been stated that a diagnosis of factitious disease (and presumably the related disorders shown in Table 4 as well as psychogenic pain) is made only after exclusion of organic illness (40). However, organic disease can rarely be excluded with certainty, a point that may be more evident to internists than to psychiatrists. Therefore, when factitious disease (or related disorders) is suspected mainly because an organic illness cannot be discovered, it would be wise to search for positive clues, as described on page 199. To do this, old medical records need to be examined, and the physician needs to speak to the patient's relatives. In the present case, there was nothing in the past medical records to suggest factitious disease, the other disorders described in Table 4, or psychogenic pain.
This case, as well as some of the earlier cases, raises questions about the roles of the primary physician and a consulting psychiatrist in the diagnosis of factitious disease. The advice of Nadelson§ rings true: “The psychiatrist must encourage the referring physician to confront the patient on the basis of clinical evidence, recognizing that the psychiatrist's own diagnostic acumen may fall short of divining the hidden truth” (14).
Acknowledgments
We are grateful to Ms. Carol Santa Ana (Byrne), Dr. Kaky Little, Dr. Bill Santangelo, Dr. Larry Schiller, Dr. Joe Shelton, Dr. Douglas Orr, Dr. Richard Meyer, Dr. Joseph Guileyardo, Dr. Marvin Stone, and Dr. Mike Emmett for their help with the patient studies that were presented. We are indebted to Cynthia Orticio, Martha Savage, and Beverly Peters for expert assistance in the preparation of this material for publication.
Footnotes
∗Galen was probably the most influential medical writer of all time. For 1500 years his works were the unimpeachable authority on all medical subjects (1).
†Gavin (pronounced to rhyme with ravine) was a great sanitarian and was a friend/coworker of Charles Dickens, Florence Nightingale, and John Snow. He died at age 40 from an accidental gunshot wound (3).
‡Richard Asher, physician to the Central Middlesex Hospital of London, had a special interest in medical words and in the importance of using them correctly. “The modern hematologist, instead of describing in English what he can see, prefers to describe in Greek what he can't.” He emphasized the dominant role the name of a disease or symptom can have on the way we think about the disease or symptom. “A rose without a name may smell as sweet, but it has far less chance of being smelt” (7). In addition to Munchausen's syndrome, he coined the name myxedema madness (8). He is remembered for his seven sins of medicine (9) and for many other reasons (8).
References
- 1.Lyons AS, Petrucelli RJ., II . An Illustrated History. New York: Abradale Press; 1987. Medicine; pp. 250–261. [Google Scholar]
- 2.Feldman MD. Untangling the Web of Munchausen Syndrome, Munchausen by Proxy, Malingering, and Factitious Disorder. New York: Brunner-Routledge; 2004. Playing Sick? pp. 18–32. [Google Scholar]
- 3.Spriggs EA. Hector Gavin, MD, FRCSE (1815–1855)—his life, his work for the sanitary movement, and his accidental death in the Crimea. Med Hist. 1984;28(3):283–292. doi: 10.1017/s0025727300035948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gavin H. On Feigned and Factitious Diseases, Chiefly of Soldiers and Seamen; on the Means Used to Simulate or Produce Them, and on the Best Modes of Discovering Imposters; Being the Prize Essay in the Class of Military Surgery, in the University of Edinburgh Session, 1835-6, with Additions. London: John Churchill; 1843. [Google Scholar]
- 5.Elwyn TS, Ahmed I. Factitious disorder. eMedicine, November 6, 2002. Available at http://www.emedicine.com/MED/topic3125.htm; accessed March 30, 2006.
- 6.Menninger KA. Polysurgery and polysurgical addiction. Psychoanalytic Quarterly. 1934;(3):173–199. [Google Scholar]
- 7.Asher R. Making sense. Lancet. 1959;(2):359–365. doi: 10.1016/s0140-6736(59)91633-2. [DOI] [PubMed] [Google Scholar]
- 8.Rowat BMT. Richard Asher and the seven sins of medicine. Humane Medicine. 1985;1(2) Available at http://www.humanehealthcare.com/Article.asp?art_id=126; accessed April 17, 2006. [Google Scholar]
- 9.Asher R. The seven sins of medicine. Lancet. 1949;(2):358–360. doi: 10.1016/s0140-6736(49)90090-2. [DOI] [PubMed] [Google Scholar]
- 10.Asher R. Munchausen's syndrome. Lancet. 1951;1(6):339–341. doi: 10.1016/s0140-6736(51)92313-6. [DOI] [PubMed] [Google Scholar]
- 11.Lipsitt DR. Introduction. In: Feldman MD, Eisendrath SJ, editors. The Spectrum of Factitious Disorders. Washington, DC: American Psychiatric Press Inc; 1996. pp. xix–xxviii. [Google Scholar]
- 12.Kass FC. Identification of persons with Munchausen's syndrome: ethical problems. Gen Hosp Psychiatry. 1985;7(3):195–200. doi: 10.1016/0163-8343(85)90066-0. [DOI] [PubMed] [Google Scholar]
- 13.Spiro HR. Chronic factitious illness. Munchausen's syndrome. Arch Gen Psychiatry. 1968;18(5):569–579. doi: 10.1001/archpsyc.1968.01740050057010. [DOI] [PubMed] [Google Scholar]
- 14.Nadelson T. The Munchausen spectrum. Borderline character features. Gen Hosp Psychiatry. 1979;1(1):11–17. doi: 10.1016/0163-8343(79)90073-2. [DOI] [PubMed] [Google Scholar]
- 15.Wallach J. Laboratory diagnosis of factitious disorders. Arch Intern Med. 1994;154(15):1690–1696. [PubMed] [Google Scholar]
- 16.Aduan RP, Fauci AS, Dale DC, Herzberg JH, Wolff SM. Factitious fever and self-induced infection: a report of 32 cases and review of the literature. Ann Intern Med. 1979;90(2):230–242. doi: 10.7326/0003-4819-90-2-230. [DOI] [PubMed] [Google Scholar]
- 17.Gault MH, Campbell NR, Aksu AE. Spurious stones. Nephron. 1988;48(4):274–279. doi: 10.1159/000184941. [DOI] [PubMed] [Google Scholar]
- 18.Reich P, Gottfried LA. Factitious disorders in a teaching hospital. Ann Intern Med. 1983;99(2):240–247. doi: 10.7326/0003-4819-99-2-240. [DOI] [PubMed] [Google Scholar]
- 19.Bruns AD, Fishkin PA, Johnson EA, Lee YT. Munchausen's syndrome and cancer. J Surg Oncol. 1994;56(2):136–138. doi: 10.1002/jso.2930560219. [DOI] [PubMed] [Google Scholar]
- 20.Read NW, Krejs GJ, Read MG, Santa Ana CA, Morawski SG, Fordtran JS. Chronic diarrhea of unknown origin. Gastroenterology. 1980;78(2):264–271. [PubMed] [Google Scholar]
- 21.Misiewicz JJ, Bartram CI, Cotton PB, Mee AS, Price AB, Thompson RPH. Slide Atlas of Gastroenterology. 9. Colon II. London: Gower Medical Publishing; 1985. [Google Scholar]
- 22.Schiller LR, Rivera LM, Santangelo WC, Little KH, Fordtran JS. Diagnostic value of fasting plasma peptide concentrations in patients with chronic diarrhea. Dig Dis Sci. 1994;39(10):2216–2222. doi: 10.1007/BF02090374. [DOI] [PubMed] [Google Scholar]
- 23.Ewe K, Karbach U. Factitious diarrhoea. Clin Gastroenterol. 1986;15(3):723–740. [PubMed] [Google Scholar]
- 24.Morris AI, Turnberg LA. Surreptitious laxative abuse. Gastroenterology. 1979;77(4 Pt 1):780–786. [PubMed] [Google Scholar]
- 25.Krejs GJ, Walsh JH, Morawski SG, Fordtran JS. Intractable diarrhea. Intestinal perfusion studies and plasma VIP concentrations in patients with pancreatic cholera syndrome and surreptitious ingestion of laxatives and diuretics. Am J Dig Dis. 1977;22(4):280–292. doi: 10.1007/BF01072184. [DOI] [PubMed] [Google Scholar]
- 26.Cummings JH, Sladen GE, James OFW, Sarner M, Misiewicz JJ. Laxative-induced diarrhoea: a continuing clinical problem. Br Med J. 1974;1(907):537–541. doi: 10.1136/bmj.1.5907.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.LaRusso NF, McGill DB. Surreptitious laxative ingestion. Delayed recognition of a serious condition: a case report. Mayo Clin Proc. 1975;50(12):706–708. [PubMed] [Google Scholar]
- 28.Josefson D. US to ban sale of many laxatives over the counter. BMJ. 1997;315(7109):627. [PMC free article] [PubMed] [Google Scholar]
- 29.Plumeri PA. The room search. J Clin Gastroenterol. 1984;6(2):181–185. doi: 10.1097/00004836-198404000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Feldman MD. Playing Sick. :218–227. [Google Scholar]
- 31.Eisendrath SJ, Feder A. Management of factitious disorders. In: Feldman MD, Eisendrath SJ, editors. The Spectrum of Factitious Disorders. Washington, DC: American Psychiatric Press; 1996. pp. 195–213. [Google Scholar]
- 32.Wedel KR. A therapeutic confrontation approach to treating patients with factitious illness. Social Work. 1971;16(2):69–73. [Google Scholar]
- 33.Eisendrath SJ. Current overview of factitious physical disorders. In: Feldman MD, Eisendrath SJ, editors. The Spectrum of Factitious Disorders. Washington, DC: American Psychiatric Press; 1996. pp. 21–36. [Google Scholar]
- 34.Bytzer P, Stokholm M, Andersen I, Klitgaard NA, Schaffalitzky de Muckadell OB. Prevalence of surreptitious laxative abuse in patients with diarrhoea of uncertain origin: a cost benefit analysis of a screening procedure. Gut. 1989;30(10):1379–1384. doi: 10.1136/gut.30.10.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fine KD, Krejs GJ, Fordtran JS. Diarrhea. In: Sleisenger MH, Fordtran JS, editors. Gastrointestinal Disease: Pathophysiology, Diagnosis, Management. 5th ed. Philadelphia: WB Saunders; 1993. pp. 1062–1065. [Google Scholar]
- 36.Moriarty KJ, Silk DBA. Laxative abuse. Dig Dis. 1988;6(1):15–29. doi: 10.1159/000171181. [DOI] [PubMed] [Google Scholar]
- 37.Slugg PH, Carey WD. Clinical feature and follow-up of surreptitious laxative users. Cleve Clin Q. 1984;51(1):167–171. doi: 10.3949/ccjm.51.1.167. [DOI] [PubMed] [Google Scholar]
- 38.Eisendrath SJ. Factitious disorders. In: Goldman HH, editor. Review of General Psychiatry. Norwalk: Appleton and Lange; 1995. pp. 368–374. [Google Scholar]
- 39.Kramer P, Pope CE. Factitious diarrhea induced by phenolphthalein. Arch Intern Med. 1964;(114):634–636. doi: 10.1001/archinte.1964.03860110104010. [DOI] [PubMed] [Google Scholar]
- 40.Rabin PL, Graham BS. Counterfeit calculi. South Med J. 1984;77(3):304–307. doi: 10.1097/00007611-198403000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Oster JR, Materson BJ, Rogers AI. Laxative abuse syndrome. Am J Gastroenterol. 1980;74(5):451–458. [PubMed] [Google Scholar]
- 42.Sutherland AJ, Rodin GM. Factitious disorders in a general hospital setting: clinical features and a review of the literature. Psychosomatics. 1990;31(4):392–399. doi: 10.1016/S0033-3182(90)72133-0. [DOI] [PubMed] [Google Scholar]
- 43.Meadow SR. Who's to blame—mothers, Munchausen or medicine? J R Coll Physicians Lond. 1994;28(4):332–337. [PMC free article] [PubMed] [Google Scholar]
- 44.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition (DSM-IV) Washington, DC: American Psychiatric Association; 1994. pp. 445–475. [Google Scholar]
- 45.Cely-Serrano MS, Wilms Floet A. Somatoform disorder: hypochondriasis. eMedicine, May 31, 2005. Available at http://www.emedicine.com/ped/topic2911.htm; accessed March 30, 2006.
- 46.Parsons T. The Social System. Glencoe, IL: Free Press; 1951. [Google Scholar]
- 47.Ford CV, Abernethy V. Factitious illness: a multidisciplinary consideration of ethical issues. Gen Hosp Psychiatry. 1981;3(4):329–336. doi: 10.1016/0163-8343(81)90042-6. [DOI] [PubMed] [Google Scholar]
- 48.Parsons T. Action Theory and the Human Condition. New York: Free Press; 1978. [Google Scholar]
- 49.Shilling C. Culture, the ‘sick role’ and the consumption of health. Br J Sociol. 2002;53(4):621–638. doi: 10.1080/0007131022000021515. [DOI] [PubMed] [Google Scholar]
- 50.American Medical Association . First code of medical ethics. Reprinted from Proceedings of the National Medical Convention 1846-1847. In: Reisen SJ, Dyck AJ, Curran WJ, editors. Ethics in Medicine, Historical Perspectives and Contemporary Concerns. Cambridge, MA: MIT Press; 1977. [Google Scholar]
- 51.Yorker BC. Liability associated with factitious disorders. J Nursing Law. 1998;5(4):7–22. [Google Scholar]
- 52.Friel JP. Dorland's Illustrated Medical Dictionary. 25th ed. Philadelphia: WB Saunders; 1974. p. 234. [Google Scholar]
- 53.Bo-Linn GW, Santa Ana CA, Morawski SG, Fordtran JS. Purging and calorie absorption in bulimic patients and normal women. Ann Intern Med. 1983;99(1):14–17. doi: 10.7326/0003-4819-99-1-14. [DOI] [PubMed] [Google Scholar]
- 54.Bulik CM, Epstein LH, Kaye W. Treatment of laxative abuse in a female with bulimia nervosa using an operant extinction paradigm. J Subst Abuse. 1990;2(3):381–388. doi: 10.1016/s0899-3289(10)80010-0. [DOI] [PubMed] [Google Scholar]
- 55.Korzets Z, Hasdan G, Podjarny E, Bernheim J. Excessive fluid gain in a chronic laxative abuser: “pseudo-idiopathic” oedema. Nephrol Dial Transplant. 2002;17(1):161–162. doi: 10.1093/ndt/17.1.161. [DOI] [PubMed] [Google Scholar]
- 56.Levin E. Karen Carpenter: death comes at 32 to the beloved singer. People Weekly, February 21, 1983.
- 57.Baylor Health Care System . To Our Patients: Your Rights and Responsibilities. Dallas, TX: BHCS; 2005. [Google Scholar]
- 58.Feldman MD. Playing Sick. :185–200. [Google Scholar]
- 59.Baile WF, Jr, Kuehn CV, Straker D. Factitious cancer. Psychosomatics. 1992;33(1):100–105. doi: 10.1016/S0033-3182(92)72027-1. [DOI] [PubMed] [Google Scholar]
- 60.Lipsitt DR. The factitious patient who sues. Am J Psychiatry. 1986;143(11):1482. doi: 10.1176/ajp.143.11.1482a. [DOI] [PubMed] [Google Scholar]
- 61.Feldman MD, Ford CV. Inside the Strange World of Factitious Disorders. New York: John Wiley; 1994. Patient or Pretender. [Google Scholar]
- 62.Feldman MD. Factitious disorders and fraud. Psychosomatics. 1995;36(5):509–510. doi: 10.1016/S0033-3182(95)71638-3. [DOI] [PubMed] [Google Scholar]
- 63.Schuffler MD. Chronic intestinal pseudo-obstruction. Gastrointestinal Disease. In: Sleisenger MH, Fordtran JS, editors. Pathophysiology/Diagnosis/Management. 7th ed. Vol. 2. Philadelphia: WB Saunders; 2002. pp. 2140–2150. [Google Scholar]
- 64.Friedman EJ. Death from ipecac intoxication in a patient with anorexia nervosa. Am J Psychiatry. 1984;141(5):702–703. doi: 10.1176/ajp.141.5.702. [DOI] [PubMed] [Google Scholar]
- 65.Santangelo WC, Richey JE, Rivera L, Fordtran JS. Surreptitious ipecac administration simulating intestinal pseudo-obstruction. Ann Intern Med. 1989;110(12):1031–1032. doi: 10.7326/0003-4819-110-12-1031. [DOI] [PubMed] [Google Scholar]
- 66.Meadow R. Munchausen syndrome by proxy. The hinterland of child abuse. Lancet. 1977;2(8033):343–345. doi: 10.1016/s0140-6736(77)91497-0. [DOI] [PubMed] [Google Scholar]
- 67.Feldman MD. Playing Sick. :121–148. [Google Scholar]
- 68.Innes J. Expert who let down parents and his own profession is struck off. The Scotsman, July 16, 2005. Available at http://news.scotsman.com/topics.cfm?tid=892&id=1636472005; accessed April 17, 2006.
- 69.Mintowt-Czyz L. Paediatrician cleared of misconduct over cot deaths evidence. The Scotsman, February 18, 2006. Available at http://news.scotsman.com/uk.cfm?id=253642006; accessed April 17, 2006.
- 70.Meadow R. Munchausen's syndrome. When a doctor turns detective. Nurs Mirror. 1982;154(26):17–20. [PubMed] [Google Scholar]
- 71.Epstein MA, Markowitz RL, Gallo DM, Holmes JW, Gryboski JD. Munchausen syndrome by proxy: considerations in diagnosis and confirmation by video surveillance. Pediatrics. 1987;80(2):220–224. [PubMed] [Google Scholar]
- 72.Ostfeld BM, Feldman MD. Factitious disorder by proxy: clinical features, detection and management. In: Feldman MD, Eisendrath SJ, editors. The Spectrum of Factitious Disorders. Washington, DC: American Psychiatric Press; 1996. pp. 83–108. [Google Scholar]
- 73.In re J.R., No. 4-248/04-0231, 2004 Iowa App. LEXIS 650 (Iowa Ct. App. April 28, 2004).
- 74.Fleisher D, Ament ME. Diarrhea, red diapers, and child abuse: clinical alertness needed for recognition; clinical skill needed for success in management. Clin Pediatr. 1977;16(9):820–824. doi: 10.1177/000992287701600916. [DOI] [PubMed] [Google Scholar]
- 75.Rogers D, Tripp J, Bentovim A, Robinson A, Berry D, Goulding R. Non-accidental poisoning; an extended syndrome of child abuse. Br Med J. 1976;1(6013):793–796. doi: 10.1136/bmj.1.6013.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Book review of Trained to Kill: Soldiers at War by Theodore Nadelson. Available at http://www.press.jhu.edu/books/title_pages/3306.html; accessed April 10, 2006.
- 77.Statz S. Book review of Trained to Kill: Soldiers at War by Theodore Nadelson. Available at http://www.bookslut.com/nonfiction/2005_10_006826.php; accessed April 10, 2006.