Abstract
OBJECTIVE
To determine whether outpatient cholesterol management varies by gender or race among patients with atherosclerosis, and assess factors related to subsequent cholesterol control.
DESIGN
Retrospective cohort study.
SETTING
Primary care clinics affiliated with an academic medical center.
PARTICIPANTS
Two hundred forty-three patients with coronary heart disease, cerebrovascular disease, or peripheral vascular disease and low-density lipoprotein cholesterol (LDL-C)>130 mg/dl.
MEASUREMENTS AND MAIN RESULTS
The primary process of care assessed for 1,082 office visits was cholesterol management (medication intensification or LDL-C monitoring). Cholesterol management occurred at 31.2% of women's and 38.5% of men's visits (P =.01), and 37.3% of black and 31.7% of white patients' visits (P =.09). Independent predictors of cholesterol management included female gender (adjusted risk ratio [ARR], 0.77; 95% confidence interval [CI], 0.60 to 0.97), seeing a primary care clinician other than the patient's primary care physician (ARR, 0.23; 95% CI, 0.11 to 0.45), and having a new clinical problem addressed (ARR, 0.60; 95% CI, 0.48 to 0.74). After 1 year, LDL-C <130 mg/dl occurred less often for women than men (41% vs 61%; P =.003), black than white patients (39% vs 58%; P =.01), and patients with only Medicare insurance than with commercial insurance (37% vs 58%; P =.008). Adjustment for clinical characteristics and management attenuated the relationship between achieving an LDL-C <130 mg/dl and gender.
CONCLUSIONS
In this high-risk population with uncontrolled cholesterol, cholesterol management was less intensive for women than men but similar for black and white patients. Less intense cholesterol management accounted for some of the disparity in cholesterol control between women and men but not between black and white patients.
Keywords: cholesterol, physician's practice patterns, coronary disease, gender factors, African Americans
Female1–5 and black patients4–11 are less likely than male and white patients, respectively, to undergo cardiac catheterization and revascularization. Clinical differences may explain a portion of the observed differences in procedure use between men and women,3,12,13 whereas socioeconomic factors,14,15 procedural availability,16 and patient preferences17–19 may explain some of the differences observed between black and white patients. Even after adjustment for these differences, gaps in treatment by gender and race remain. Clinicians' decision making may be subject to subtle biases, as was suggested by one study of simulated patients in which black women were least likely to be referred for cardiac catheterization.20
Patients' gender and race may also affect clinicians' decisions about cardiovascular drug treatment. Women at high risk for cardiovascular events appear to be less likely than men to achieve control of cholesterol21–24 or other coexisting cardiac risk factors.25 While some studies suggest that women with coronary artery disease are less likely to be given effective medications such as aspirin, beta-blockers, and thrombolytics in the hospital setting,26 studies examining gender differences in inpatient and outpatient use of cholesterol-lowering medication have had mixed results.24,26–30 Black adults are less likely than white adults to have cholesterol screening or use cholesterol-lowering medications,27,31–33 and are less likely to achieve target cholesterol levels and control of other cardiac risk factors.23,25,34 Most prior studies have been cross-sectional in design, however, so the role of clinicians' treatment decisions in these disparities is not well understood. Also, group disparities in intermediate clinical outcomes such as cholesterol level could be due to differences in clinical care or could be from other causes.35
Our goal was to examine ambulatory care of patients with cardiovascular disease and elevated low-density lipoprotein cholesterol (LDL-C) to assess whether cholesterol management decisions and subsequent control of LDL-C differed by patients' gender or race. We addressed the following questions: is gender or race associated with the intensity of medical therapy and cholesterol monitoring in the office setting? What other factors are associated with the intensity of cholesterol management? Do patients of different gender or race receiving care from the same clinics achieve similar cholesterol control over time?
METHODS
Identification of Patient Population
We selected patients from all of the primary care internal medicine practices affiliated with an academic medical center in Boston, MA (4 hospital-based practices and 6 community-located practices). The Institutional Review Board of Brigham and Women's Hospital approved the study.
We identified patients with coronary heart disease (CHD), peripheral vascular disease (PVD), or cerebrovascular disease (CVD) by electronically searching a physician-maintained coded patient problem list in an electronic medical record for the following terms: angina, myocardial infarction, claudication, transient ischemic attack, stroke, percutaneous transluminal coronary angioplasty, coronary artery bypass surgery, carotid endarterectomy, peripheral artery angioplasty, or peripheral artery bypass. We included patients with at least one visit to a general internist between November 14, 1999 and November 13, 2000. We identified 1,608 patients with CHD, CVD, or PVD who had office visits with general internists during this time interval, of whom 409 (25.4%) had no LDL-C determination in the prior year, 337 (21.0%) had LDL-C measured at >130 mg/dl, 441 (27.4%) had a value between 100 and 130 mg/dl, and 421 (26.2%) had a value below 100 mg/dl. We included patients whose most recent LDL-C measurement in the prior year was >130 mg/dl.
A physician (S.D.P.) reviewed patients' electronic medical records. Patients who did not have a qualifying diagnosis or procedure in an office note on or before the index visit were excluded. Patients with angina but no ischemia on stress tests were excluded. Patients with stroke were excluded if they only had a hemorrhagic or small-vessel ischemic stroke seen on brain imaging. Patients with a transient ischemic attack or large-vessel ischemic stroke were excluded if they had atrial fibrillation, valvular heart disease, or cardiomyopathy as a risk factor for stroke and did not have carotid artery stenosis on an imaging study. Of the 337 patients with LDL-C >130 mg/dl, we excluded 75 patients who did not have a confirmed atherosclerosis diagnosis and 19 patients who on review did not have available office notes or whose records documented that their primary care was obtained elsewhere. The remaining 243 patients constituted the study cohort. We designated the first visit in the time interval with a preceding LDL-C of >130 mg/dl as the index visit.
Data Collection
For patients with confirmed CHD, PVD, or CVD a physician reviewed office notes in the electronic medical record from visits with a general internist, cardiologist, nurse practitioner, or diabetes specialist within 1 year following the index visit using a structured chart review instrument as well as other documentation in the medical record from these providers or their office staff. For each visit, we recorded the type of provider, up to 4 problems addressed in the visit, current cholesterol-lowering medications, adverse reactions to cholesterol-lowering medications, patient nonadherence to cholesterol-lowering therapy, and patient refusal of cholesterol-lowering therapy. We also collected information on severe noncardiac comorbidities (active cancer, severe pulmonary disease, end-stage renal disease, dementia or memory loss, and chronic active liver disease) as well as diabetes mellitus, hypertension, current smoking, heart failure, and psychiatric illness (depression, bipolar disorder, schizophrenia, or psychosis). We classified patients as nonadherent to treatment for hypercholesterolemia if their medical record during the 1 year of review mentioned that the patient stopped or reduced a medication for hypercholesterolemia on their own accord or declined to take a medication when recommended. A visit was considered to address a new clinical problem if a symptom or condition was mentioned in the clinician's note and this problem had not been previously noted more than 30 days before the visit. Changes in medical management for hypercholesterolemia were categorized as adding a new medication, increasing a current medication, resuming or increasing a medication a patient had discontinued or reduced, reducing or discontinuing a medication, or substituting one medication for another. Age, gender, race/ethnicity, and type of health insurance were abstracted from the electronic record. Providers were classified by gender, specialty, and level of training.
Process of Care Measures at Office Visits
For individual visits we evaluated 3 processes of care: LDL-C monitoring, intensification of medical therapy, and the combined measure of intensification of medical therapy or LDL-C monitoring. Because appropriate management of hypercholesterolemia depends on both medication adjustment and laboratory monitoring, and because a composite measure provided us with greater statistical power for group comparisons, a priori we chose this combination as the primary visit–level measurement of treatment intensity. We considered visits ineligible for assessment of the process measures if a preceding LDL-C measurement was <100 mg/dl or a medication change occurred in the prior 6 weeks. The LDL-C monitoring measure was met if the note mentioned any cholesterol testing was to be done following that visit or there was a new LDL-C measurement in the electronic record within 14 days after the office visit (but prior to subsequent visits). We considered the intensification process measure met if there was documentation that a provider added a cholesterol-lowering medication, increased the dose, resumed a medication the patient had discontinued, or substituted a medication with greater expected LDL-C lowering for another medication.36 This criterion was also met if there was documentation of intensification occurring by telephone or letter within 1 month after the visit but prior to the next visit.
Outcome at one Year
We determined whether there was an LDL-C below 130 mg/dl within 1 year from the index visit. We chose the threshold of an LDL-C <130 mg/dl as the primary patient outcome because there was expert agreement during the time of our study that patients with atherosclerosis and LDL-C above 130 mg/dl should be offered medical therapy,37 and the 130 mg/dl threshold has been adopted by the Health Plan and Employer Data and Information Set as a measure of quality of care for patients following a myocardial infarction.38
Statistical Analysis
For descriptive analyses, we used the χ2 test for categorical variables, Student's t test for normally distributed continuous variables, and the Wilcoxon rank sum test for nonnormally distributed continuous variables.
To assess the adjusted association of gender and race with outcomes, we used multivariable logistic regression with generalized estimating equations (PROC GENMOD, SAS 8.2, SAS Institute, Cary, NC) to account for clustering at the level of the patient for analysis of visit processes of care and at the level of the primary care provider for the patient outcome at 1 year.39 Because age was not linearly associated with the study outcomes, we treated it as a categorical variable. When data were missing, an indicator variable was used to denote missing data in multivariable models. We added other explanatory variables that were associated with the outcome in univariate analysis (P <.1) to models that included patient gender, race, and age, in a stepwise fashion, and retained variables in the final multivariable models if they were statistically significant with a P value <.05 or if their removal changed the estimated parameters for the effects of patient gender or race by at least .1 in the logistic model. For the model predicting LDL-C below 130 mg/dl within 1 year, we also tested a model with terms for lab testing and medication intensification occurring during the year. To make the effect sizes easier to interpret, we converted odds ratios to adjusted risk ratios.40 All tests of significance were two-sided.
RESULTS
Of the 243 patients with LDL-C >130 mg/dl, 129 (53.1%) were women and 114 (46.9%) were men. White patients comprised 56% of the cohort, black patients 28%, and patients of other race 8% (Table 1). Compared with men, women were older, more likely to be black, more likely to receive care at a hospital-based practice, and not to have commercial health insurance. They were less likely to have CHD, to have undergone coronary artery bypass graph surgery, and to be taking a cholesterol-lowering medication prior to the index visit. White patients were less likely than black patients to have Medicare or Medicaid as their only form of health insurance, to receive care at a hospital-based practice, or to have hypertension or diabetes.
Table 1.
Characteristics of Patients with Atherosclerosis and LDL-C Measured>130 mg/dl
| Characteristics at Index Visit | Total (N =243) | Women (n =129) | Men (n =114) | P Value |
|---|---|---|---|---|
| Race, n (%) | .05 | |||
| Black | 67 (28) | 44 (34) | 23 (20) | |
| White | 137 (56.4) | 70 (54) | 67 (59) | |
| Other race | 20 (8.2) | 8 (6) | 12 (11) | |
| Unknown | 19 (7.8) | 7 (5) | 12 (11) | |
| Mean age, y (SD) | 66.6 (11.4) | 68.7 (11.5) | 64.3 (10.9) | .003 |
| Health insurance, n (%) | .13 | |||
| Commercial insurance | 150 (61.7) | 71 (55) | 79 (69) | |
| Medicare only | 54 (22) | 35 (27) | 19 (17) | |
| Medicaid/MA Free Care | 35 (14) | 21 (16) | 14 (12) | |
| Uninsured | 4 (2) | 2 (2) | 2 (2) | |
| Practice location, n (%) | .02 | |||
| Hospital-based | 169 (70) | 98 (76) | 71 (62) | |
| Community-based | 74 (30) | 31 (24) | 43 (38) | |
| LDL-C before index visit, mean (SD) | 156.5 (24.9) | 158.1 (24.8) | 154.8 (24.9) | .30 |
| Type of atherosclerosis, n (%) | .01 | |||
| CHD | 191 (78.6) | 92 (71) | 99 (87) | |
| PVD (no CHD) | 32 (13) | 23 (18) | 9 (8) | |
| CVD only | 20 (8.2) | 14 (11) | 6 (5) | |
| Myocardial infarction, n (%) | 83 (34) | 38 (29) | 45 (39) | .10 |
| CABG, n (%) | 56 (23) | 21 (16) | 35 (31) | .008 |
| Angioplasty/coronary stent, n (%) | 44 (18) | 19 (15) | 25 (22) | .15 |
| Diabetes, n (%) | 86 (35) | 49 (38) | 37 (32) | .37 |
| Hypertension, n (%) | 173 (71.2) | 95 (74) | 78 (68) | .37 |
| Current smoking, n (%) | 51 (21) | 26 (20) | 25 (22) | .73 |
| Heart failure, n (%) | 45 (19) | 23 (18) | 22 (19) | .77 |
| Psychiatric illness, n (%) | 60 (25) | 32 (25) | 28 (25) | .96 |
| Major noncardiac comorbidity, n (%) | 36 (15) | 21 (16) | 15 (13) | .49 |
| Cholesterol medication at index visit, n (%) | 145 (59.7) | 69 (53) | 76 (67) | .04 |
LDL-C, low-density lipoprotein cholesterol; SD, standard deviation; CHD, coronary heart disease; CVD, cerebral vascular disease; PVD, peripheral vascular disease; CABG, coronary artery bypass graph surgery.
Process of Care Measures at Office Visits
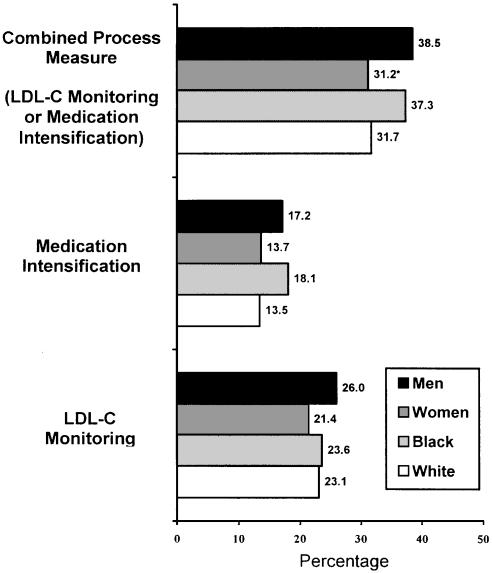
During 1 year of follow-up, these 243 patients made 1,389 office visits to 162 providers: 126 general internists (80 attending physicians and 46 residents), 8 nurse practitioners, 26 cardiologists, and 2 diabetes specialists. Of the visits, 1,076 (77.5%) were with the patients' primary care general internist, 65 (4.7%) with other general internists, 70 (5.0%) with nurse practitioners, 169 (12.2%) with cardiologists, and 60 (9.7%) with diabetes specialists. Visits to cardiologists were less frequent among women and nonwhite patients. New problems were addressed at 650 (46.8%) visits. Of the 1,389 visits, 307 were excluded from analysis because either they had a preceding medication change in the 6 weeks prior or a new LDL-C level was <100 mg/dl. Among the 1,082 visits eligible for cholesterol management, the combined process measure of medication intensification or LDL-C monitoring occurred at 198/635 (31.2%) visits with women and 172/447 visits with men (38.5%; P =.01; Fig. 1). LDL-C monitoring occurred following 252/1,082 (23.3%) visits (21.4% for women and 26.0% for men; P =.08) and medication intensification occurred at 159/1,082 (15.2%) visits eligible for this outcome (13.7% for women and 17.2% for men; P =.11). Medication intensification tended to occur more often at visits of black patients compared to white patients (18.1% vs 13.5%; P =.06).
FIGURE 1.
Frequency of cholesterol management processes of care occurring at eligible office visits. *P =.01 compared to men.
In multivariate analysis adjusting for factors related to treatment intensity, the combined visit process measure occurred less often for visits with women (adjusted risk ratio [ARR], 0.77; 95% confidence interval [CI], 0.60 to 0.97; Table 2). Individually, medication intensification and LDL-C monitoring were both less frequent in women, but these differences were not statistically significant. Cholesterol management occurring at visits was not associated with patients' race. Visits with higher preceding LDL-C levels were more likely to result in LDL-C monitoring, medication intensification, or the combined outcome. Visits with primary care site providers who were not the primary care physician were much less likely to result in cholesterol management, whereas management outcomes for visits with cardiologists and primary care internists were similar. Visits by nonadherent patients and to hospital-based practices were more likely to result in the combined outcome and in medication intensification. Visits where new problems were addressed were less likely to result in all the cholesterol management outcomes. Taking more potent drugs to lower LDL-C before a visit was associated with more frequent LDL-C monitoring at the visit and less frequent medication intensification.
Table 2.
Predictors of Cholesterol Processes of Care at Office Visits*
| Characteristic | Medication Intensification or LDL-C Monitoring | Medication Intensification | LDL-C Monitoring |
|---|---|---|---|
| Adjusted Risk Ratio | Adjusted Risk Ratio | Adjusted Risk Ratio | |
| (95% CI) | (95% CI) | (95% CI) | |
| Female gender | 0.77 (0.60 to 0.97)† | 0.72 (0.49 to 1.05) | 0.88 (0.67 to 1.12) |
| White | 1 | 1 | 1 |
| Black | 0.99 (0.73 to 1.30) | 1.02 (0.66 to 1.52) | 1.01 (0.75 to 1.32) |
| Other race | 0.99 (0.75 to 1.26) | 0.85 (0.44 to 1.56) | 1.07 (0.71 to 1.54) |
| Age | |||
| <65 years | 0.99 (0.76 to 1.24) | 0.97 (0.64 to 1.44) | 0.80 (0.56 to 1.10) |
| 65–74 years | 1 | 1 | 1 |
| ≥75 years | 0.79 (0.58 to 1.04) | 0.88 (0.53 to 1.41) | 1.02 (0.77 to 1.34) |
| LDL-C before visit (per 10 mg/dl) | 1.11 (1.06 to 1.15)‡ | 1.12 (1.07 to 1.16)‡ | 1.10 (1.05 to 1.14)‡ |
| Time since prior visit | |||
| <30 days | 0.61 (0.45 to 0.92)§ | – | 0.47 (0.27 to 0.74)‡ |
| 30–180 days | 0.78 (0.57 to 1.03) | – | 0.72 (0.48 to 1.02) |
| >180 days | 1 | – | 1 |
| Cholesterol medication potency prior to visit | |||
| (LDL-C lowering %) None | – | 1 | 1 |
| <40 | – | 0.52 (0.33 to 0.82)§ | 1.33 (0.97 to 1.79) |
| ≥40 | – | 0.44 (0.27 to 0.69)§ | 2.48 (1.91 to 3.12)‡ |
| Medication nonadherence | 1.39 (1.11 to 1.76)§ | 2.74 (1.99 to 3.65)‡ | – |
| New problem at visit | 0.60 (0.48 to 0.74)‡ | 0.44 (0.33 to 0.61)‡ | 0.75 (0.58 to 0.96)† |
| Type of provider | |||
| Primary care physician | 1 | – | 1 |
| Other clinician at PC site | 0.23 (0.11 to 0.45)‡ | – | 0.23 (0.09 to 0.56)‡ |
| Cardiologist | 1.13 (0.77 to 1.54) | – | 1.03 (0.68 to 1.48) |
| Diabetes specialist | 1.48 (0.94 to 1.99) | – | 0.81 (0.14 to 2.56) |
| Hospital-based practice | 1.36 (1.04 to 1.72)† | 1.82 (1.25 to 2.59)§ |
Variables in multivariable models were selected through stepwise selection as described in the methods. Variables removed from multivariable models during the selection procedure include variables where no value is given in the table and for all 3 models: type of health insurance, type of atherosclerosis, prior myocardial infarction, coronary artery bypass graft, percutaneous revascularization, diabetes, hypertension, smoking, heart failure, psychiatric illness, major noncardiac comorbidity, resident status of provider, and gender of provider.
P <.03.
P <.001.
P <.01.
LDL-C, low-density lipoprotein cholesterol; PC, primary care; CI, confidence interval.
Outcomes at one Year
During the year after the index visit, women had fewer LDL-C measurements (median 1 vs 2; P =.01) and were less likely to have a measured LDL-C <130 mg/dl compared to men (41% vs 61%; P =.003) (Table 3). Black patients were less likely to have an LDL-C <130 mg/dl compared to white patients (39% vs 58%; P =.01). Patients with only Medicare were less likely than patients with commercial insurance to meet this goal (37% vs 58%; P =.008).
Table 3.
Characteristics Observed by 1-Year Follow-up
| Characteristic | Total | Women | Men | P Value | White | Black | P Value |
|---|---|---|---|---|---|---|---|
| Visits per year, median (IQR) | 5 (3–7) | 5 (3–7) | 5 (3–7) | .19 | 5 (3–7) | 6 (4–8) | .06 |
| Statin intolerance, n (%) | 50 (21) | 32 (25) | 18 (16) | .08 | 29 (21) | 17 (25) | .50 |
| Medication nonadherence, n (%) | 61 (25) | 33 (26) | 28 (25) | .85 | 28 (20) | 22 (33) | .05 |
| Seen by cardiologist, n (%) | 71 (29) | 30 (23) | 41 (36) | .03 | 48 (35) | 12 (18) | .01 |
| Frequent new problems at visits, n (%)* | 75 (31) | 42 (33) | 33 (29) | .54 | 49 (36) | 14 (21) | .03 |
| LDL-C tests in 1 year, median (IQR) | 1 (1–2) | 1 (0–2) | 2 (1–2) | .02 | 1 (1–2) | 1 (1–2) | .74 |
| Medication increases or additions in 1 year, median (IQR) | 1 (0–1) | 1 (0–1) | 1 (0–1) | .29 | 0 (0–1) | 1 (0–2) | .02 |
| On cholesterol-lowering medication at last visit, n (%) | 185 (76.1) | 95 (74) | 90 (79) | .33 | 104 (75.9) | 52 (78) | .79 |
| LDL-C<130 mg/dl within 1 year of index visit, n (%) | 122 (50.2) | 53 (41) | 69 (61) | .003 | 79 (58) | 26 (39) | .01 |
| Days to achievement of LDL < 130 mg/dl for patients reaching LDL-C < 130 mg/dl, median (IQR) | 77 (31–189) | 77 (35–181) | 77 (20–189) | .98 | 77 (20–189) | 80 (45–140) | .59 |
| LDL-C<100 mg/dl within 1 year of index visit, n (%) | 56 (23) | 25 (19) | 31 (27) | .15 | 37 (27) | 12 (18) | .15 |
At least two thirds of visits had a new problem addressed.
LDL-C, low-density lipoprotein cholesterol; IQR, interquartile range.
Table 4 shows results from sequential logistic models predicting the achievement of an LDL-C measured <130 mg/dl within 1 year. After terms for lab testing and medication intensification that occurred during the year were added to the model that included gender, race, and age, the difference between men and women was attenuated and no longer statistically significant, but the difference between black and white patients remained highly significant (Model 2). In the model that also includes other significant predictors of having an LDL-C <130 mg/dl within 1 year, black patients were significantly less likely than white patients to achieve this goal (ARR, 0.35; 95% CI, 0.15 to 0.71), but the difference between men and women was not statistically significant (ARR for women vs men 0.78; 95% CI, 0.45 to 1.11). Achieving an LDL-C <130 mg/dl within 1 year was positively associated with having had a myocardial infarction and negatively associated with having only Medicare insurance, having medication nonadherence documented in the medical record, and having a new clinical problem addressed at two thirds or more visits (Table 4).
Table 4.
Predictors of Achieving LDL-C Below 130 mg/dl in 1 Year
| Characteristic | Adjusted Risk Ratio (95% CI) | Adjusted Risk Ratio (95% CI) | Adjusted Risk Ratio (95% CI) |
|---|---|---|---|
| Model 1* | Model 2† | Model 3‡ | |
| Female gender | 0.65 (0.44 to 0.87)§ | 0.73 (0.46 to 1.03) | 0.78 (0.45 to 1.11) |
| Race | |||
| White | 1 | 1 | 1 |
| Black | 0.72 (0.48 to 0.97)‖ | 0.41 (0.22 to 0.71)§ | 0.35 (0.15 to 0.71)§ |
| Other race | 0.63 (0.28 to 1.10) | 0.61 (0.19 to 1.24) | 0.82 (0.26 to 1.38) |
| Age, y | |||
| < 65 | 0.66 (0.46 to 0.88)§ | 0.69 (0.40 to 1.02) | 0.51 (0.23 to 0.91)‖ |
| 65–74 | 1 | 1 | 1 |
| ≥75 | 0.76 (0.50 to 1.02) | 0.79 (0.45 to 1.14) | 0.56 (0.23 to 1.05) |
| LDL-C tests done in 1 year¶ | |||
| 0–2 | 1 | 1 | |
| ≥3 | 4.52 (3.63 to 5.12)§ | 2.98 (2.68 to 3.11)§ | |
| Medication increases in 1 year¶ | |||
| 0–1 | 1 | 1 | |
| ≥2 | 1.68 (1.23 to 2.02)§ | 1.64 (1.20 to 1.88)# | |
| Health insurance | |||
| Commercial insurance | 1 | ||
| Medicare only | 0.46 (0.18 to 0.91)‖ | ||
| Medicaid/ MA Free Care | 0.75 (0.23 to 1.38) | ||
| Uninsured | 1.08 (0.22 to 1.64) | ||
| Myocardial infarction | 1.60 (1.09 to 1.97)‖ | ||
| Medication nonadherence | 0.21 (0.07 to 0.54)§ | ||
| Resident PCP | 1.38 (0.95 to 1.65) | ||
| New problem at >2/3 of visits | 0.48 (0.24 to 0.81)§ | ||
Results adjusted for gender, race, and age.
Results adjusted for gender, race, age, LDL-C testing, and medication increases in 1 year.
Results adjusted for all variables in Model 2 and variables selected through stepwise selection as described in the methods with the following variables excluded: type of atherosclerosis, coronary artery bypass graft, percutaneous revascularization, diabetes, hypertension, smoking, heart failure, psychiatric illness, major noncardiac comorbidity, statin intolerance, number of visits, initial LDL-C, primary care practice location, seen by a cardiologist during the year, and gender of primary care physician.
P <.005.
P <.05.
To account for the differences in the amount of time each patient was not at goal, these values were calculated as the number of lab tests or medication increases that occurred during the time prior to achievement of the LDL-C goal divided by the fraction of the year the patient was not at goal.
P <.01.
LDL-C, low-density lipoprotein cholesterol; PCP, primary care provider; CI, confidence interval.
DISCUSSION
For patients with atherosclerosis and elevated LDL-C, examination of care occurring at individual visits shows women were less intensely managed for hypercholesterolemia compared to men in adjusted analyses. Both female and black patients were more likely than male and white patients, respectively, to still have high cholesterol after 1 year despite many medical encounters. The difference between women and men in cholesterol control at 1 year decreased after accounting for differences in cholesterol management during the year, but racial differences did not.
The gender differences we observed for hypercholesterolemia treatment are similar to the observed differences between men and women in the use of invasive cardiovascular procedures.1–5,12,13 Our findings suggest the less aggressive approach clinicians take to cholesterol management in women is not based on clinical risk. Cholesterol treatment guidelines acknowledge women's lower risk for the initial development of atherosclerotic disease but not for recurrent events.37,41 Inappropriately assuming women with clinical atherosclerosis require less aggressive management of cardiac risk factors because women have lower risk for initial events may explain our results to some extent, and future research should explore this possibility. Cross-sectional studies have had conflicting results as to whether cholesterol-lowering medications are used at different rates for men or women following a myocardial infarction.27,29,30 Even though women and men in our population used cholesterol-lowering medications at similar rates by the end of 1 year of follow-up, examination of management choices at individual visits revealed less intensive management for women compared to men. While our study was not large enough to quantify how much of this difference was due to less frequent increases in medications versus laboratory monitoring, both tended to occur less often for women.
There are several possible reasons why black patients who received similar cholesterol management at their clinic visits were less likely to achieve cholesterol control over time compared to white patients. Socioeconomic factors associated with race have explained some of the differences in cardiovascular procedure rates,5,14,15 and could be important determinants of medical treatment outcomes as well. We did not have access to financial information other than type of health insurance. The financial burden of prescription medication for hypercholesterolemia may have been larger for black patients than for white patients, leading to lower rates of medication adherence (67% vs 80%), but this alone did not explain the differences in achieving target LDL-C after 1 year. However, we were only able to account for physician-recorded nonadherence, which may not be ascertained or recorded consistently, or which may be admitted to less frequently among patients of certain races. Other possible explanations for racial differences in cholesterol control include differences in health beliefs, or in other aspects of the physician-patient relationship. Future research should explore whether interventions aimed at addressing these factors diminish racial differences in the control of cardiac risk factors.
Medication nonadherence was documented in the medical record for 25% of patients. Nonadherent patients were much less likely to have controlled LDL-C after 1 year, despite being more likely to have medication intensification recommended at office visits. Nonadherence and treatment discontinuation represent major obstacles to cholesterol control,42,43 but did not in our study account for the differences observed by gender or race unless medical noncompliance was underreported by women or black patients, or was documented less often by their care providers.
Although having a prior myocardial infarction was not associated with treatment at office visits, it was strongly associated with achieving an LDL-C <130 mg/dl within 1 year. It is possible that patients with a prior myocardial infarction receive stronger recommendations from physicians about cholesterol management or are more likely to follow through with recommendations than are patients with other manifestations of atherosclerosis.
Our findings have implications for the organization of primary care delivery. Both having a new clinical problem addressed and being seen by someone in primary care other than the regular primary care physician decreased the likelihood that hypercholesterolemia would be managed. While patients with frequent new problems may differ from other patients in ways that explain the observed differences in cholesterol management and outcomes, it is also possible that scheduling visits dedicated to cardiovascular disease management could lead to more successful risk factor reduction. Similarly, because preventive care can be accomplished during visits for other reasons,44 increasing patients' access to their own primary care physician for acute care or illness care should be tested as a means of improving the delivery of chronic disease care.45
Our findings add to existing evidence that lack of prescription drug coverage poses a major obstacle to cholesterol control.46 Even though insurance type was not associated with management occurring at office visits, patients with only Medicare insurance were much less likely to reach an LDL-C <130 mg/dl compared to patients with commercial insurance. Patients with Medicaid insurance or Massachusetts Free Care coverage (both of which include a prescription drug benefit) were not significantly less likely to reach this goal compared to those with commercial insurance. Improving patients' access to affordable medications may lead to better cholesterol control among patients who face high out-of-pocket costs.
Our study has several strengths, including its evaluation of all visits occurring over a 1-year period and analysis of detailed clinical information from individual office visits, but there are also several limitations. We examined all patients with documented elevated cholesterol instead of only incident cases of hypercholesterolemia. Physicians' experience with patients occurring before the time interval we analyzed could have influenced the treatment decisions we observed but may not have been captured by the portion of the medical record we examined. We examined the electronic medical record only and did not have other ways to verify adherence to prescribed medication. We used an LDL-C quality measure (<130 mg/dl) as our main clinical outcome. Cholesterol lowering well below this target has been shown to be beneficial for high-risk patients,47–49 and therefore many patients who achieved the quality benchmark we used may still not be receiving optimal care. We were limited by the number of patients available for study at our sites, and we did not have statistical power to adequately evaluate differences in the individual components of cholesterol management. Also, while we included community- and hospital-based practices, these sites were affiliated with a single medical center, and therefore our findings may not be generalizable to other populations. We did not have socioeconomic information available other than type of health insurance, and it is possible that unmeasured economic factors confound the associations we observed.
In a population of patients with atherosclerosis and hypercholesterolemia, women received less intense management of their cholesterol than men, and this difference partially explained their lower likelihood of achieving adequate cholesterol control. Black and white patients were offered similar cholesterol management, yet black patients were still less likely to achieve cholesterol control over time. Interventions to improve the effectiveness of ambulatory care for hypercholesterolemia among high-risk individuals could have substantial benefits in preventing future cardiovascular events and mortality.
Acknowledgments
This work was supported in part by institutional National Research Service Award 5T32HS00020-16 (Dr. Persell) and grant RO1 #1 U18 HS11046 from the Agency for Healthcare Research and Quality, Rockville, MD.
REFERENCES
- 1.Tobin JN, Wassertheil-Smoller S, Wexler JP, et al. Sex bias in considering coronary bypass surgery. Ann Intern Med. 1987;107:19–25. doi: 10.7326/0003-4819-107-1-19. [DOI] [PubMed] [Google Scholar]
- 2.Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med. 1991;325:221–5. doi: 10.1056/NEJM199107253250401. [DOI] [PubMed] [Google Scholar]
- 3.Krumholz HM, Douglas PS, Lauer MS, Pasternak RC. Selection of patients for coronary angiography and coronary revascularization early after myocardial infarction:is there evidence for a gender bias? Ann Intern Med. 1992;116:785–90. doi: 10.7326/0003-4819-116-10-785. [DOI] [PubMed] [Google Scholar]
- 4.Udvarhelyi IS, Gatsonis C, Epstein AM, Pashos CL, Newhouse JP, McNeil BJ. Acute myocardial infarction in the Medicare population:process of care and clinical outcomes. JAMA. 1992;268:2530–6. [PubMed] [Google Scholar]
- 5.Sheifer SE, Escarce JJ, Schulman KA. Race and sex differences in the management of coronary artery disease. Am Heart J. 2000;139:848–57. doi: 10.1016/s0002-8703(00)90017-6. [DOI] [PubMed] [Google Scholar]
- 6.Oberman A, Cutter G. Issues in the natural history and treatment of coronary heart disease in black populations:surgical treatment. Am Heart J. 1984;108:688–94. doi: 10.1016/0002-8703(84)90656-2. [DOI] [PubMed] [Google Scholar]
- 7.Maynard C, Fisher LD, Passamani ER, Pullum T. Blacks in the coronary artery surgery study (CASS):race and clinical decision making. Am J Public Health. 1986;76:1446–8. doi: 10.2105/ajph.76.12.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wenneker MB, Epstein AM. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;261:253–7. [PubMed] [Google Scholar]
- 9.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269:2642–6. [PubMed] [Google Scholar]
- 10.Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329:621–7. doi: 10.1056/NEJM199308263290907. [DOI] [PubMed] [Google Scholar]
- 11.Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary-revascularization procedures. Are the differences real? Do they matter? N Engl J Med. 1997;336:480–6. doi: 10.1056/NEJM199702133360706. [DOI] [PubMed] [Google Scholar]
- 12.Kostis JB, Wilson AC, O'Dowd K, et al. for the MIDAS Study Group. Sex differences in the management and long-term outcome of acute myocardial infarction:a statewide study. Circulation. 1994;90:1715–30. doi: 10.1161/01.cir.90.4.1715. [DOI] [PubMed] [Google Scholar]
- 13.Bickell NA, Pieper KS, Lee KL, et al. Referral patterns for coronary artery disease treatment:gender bias or good clinical judgment? Ann Intern Med. 1992;116:791–7. doi: 10.7326/0003-4819-116-10-791. [DOI] [PubMed] [Google Scholar]
- 14.Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335:791–9. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 15.Daumit GL, Hermann JA, Coresh J, Powe NR. Use of cardiovascular procedures among black persons and white persons:a 7-year nationwide study in patients with renal disease. Ann Intern Med. 1999;130:173–82. doi: 10.7326/0003-4819-130-3-199902020-00002. [DOI] [PubMed] [Google Scholar]
- 16.Gregory PM, Rhoads GG, Wilson AC, O'Dowd KJ, Kostis JB. Impact of availability of hospital-based invasive cardiac services on racial differences in the use of these services. Am Heart J. 1999;138:507–17. doi: 10.1016/s0002-8703(99)70154-7. [DOI] [PubMed] [Google Scholar]
- 17.Schecter AD, Goldschmidt-Clermont PJ, McKee G, et al. Influence of gender, race, and education on patient preferences and receipt of cardiac catheterizations among coronary care unit patients. Am J Cardiol. 1996;78:996–1001. doi: 10.1016/s0002-9149(96)00523-1. [DOI] [PubMed] [Google Scholar]
- 18.Sedlis SP, Fisher VJ, Tice D, Esposito R, Madmon L, Steinberg EH. Racial differences in performance of invasive cardiac procedures in a Department of Veterans Affairs Medical Center. J Clin Epidemiol. 1997;50:899–901. doi: 10.1016/s0895-4356(97)00089-9. [DOI] [PubMed] [Google Scholar]
- 19.Whittle J, Conigliaro J, Good CB, Joswiak M. Do patient preferences contribute to racial differences in cardiovascular procedure use? J Gen Intern Med. 1997;12:267–73. doi: 10.1046/j.1525-1497.1997.012005267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 21.Schrott HG, Bittner V, Bittinghoff E, et al. Adherence to national cholesterol education program treatment goals in postmenopausal women with heart disease:the Heart and Estrogen/Progestin Replacement Study (HERS) JAMA. 1997;277:1281–6. [PubMed] [Google Scholar]
- 22.Pearson TA, Laurora I, Chu H, Kafonek S. The Lipid Treatment Assessment Project (L-TAP):a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–67. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 23.Maviglia SM, Teich JM, Fiskio J, Bates DW. Using an electronic medical record to identify opportunities to improve compliance with cholesterol guidelines. J Gen Intern Med. 2001;16:531–7. doi: 10.1046/j.1525-1497.2001.016008531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller M, Byington R, Hunninghake D, Pitt B, Furberg CD. Sex bias and underutilization of lipid-lowering therapy in patients with coronary artery disease at academic medical centers in the United States and Canada. Arch Intern Med. 2000;160:343–7. doi: 10.1001/archinte.160.3.343. [DOI] [PubMed] [Google Scholar]
- 25.Qureshi AI, Suri MF, Guterman LR, Hopkins LN. Ineffective secondary prevention in survivors of cardiovascular events in the US population:report from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2001;161:1621–8. doi: 10.1001/archinte.161.13.1621. [DOI] [PubMed] [Google Scholar]
- 26.Nohria A, Vaccarino V, Krumholz HM. Gender differences in mortality after myocardial infarction: why women fare worse than men. Cardiol Clin. 1998;16:45–57. doi: 10.1016/s0733-8651(05)70383-0. [DOI] [PubMed] [Google Scholar]
- 27.Ayanian JZ, Landrum MB, McNeil BJ. Use of cholesterol-lowering therapy by elderly adults after myocardial infarction. Arch Intern Med. 2002;162:1013–9. doi: 10.1001/archinte.162.9.1013. [DOI] [PubMed] [Google Scholar]
- 28.Majumdar SR, Gurwitz JH, Soumerai SB. Undertreatment of hyperlipidemia in the secondary prevention of coronary artery disease. J Gen Intern Med. 1999;14:711–7. doi: 10.1046/j.1525-1497.1999.02229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCormick D, Gurwitz JH, Lessard D, Yarzebski J, Gore JM, Goldberg RJ. Use of aspirin, beta-blockers, and lipid-lowering medications before recurrent acute myocardial infarction:missed opportunities for prevention? Arch Intern Med. 1999;159:561–7. doi: 10.1001/archinte.159.6.561. [DOI] [PubMed] [Google Scholar]
- 30.Fonarow GC, French WJ, Parsons LS, Sun H, Malmgren JA. Use of lipid-lowering medications at discharge in patients with acute myocardial infarction:data from the National Registry of Myocardial Infarction 3. Circulation. 2001;103:38–44. doi: 10.1161/01.cir.103.1.38. [DOI] [PubMed] [Google Scholar]
- 31.Naumburg EH, Franks P, Bell B, Gold M, Engerman J. Racial differentials in the identification of hypercholesterolemia. J Fam Pract. 1993;36:425–30. [PubMed] [Google Scholar]
- 32.Ayanian JZ, Landon BE, Landrum MB, Grana JR, McNeil BJ. Use of cholesterol-lowering therapy and related beliefs among middle-aged adults after myocardial infarction. J Gen Intern Med. 2002;17:95–102. doi: 10.1046/j.1525-1497.2002.10438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nelson K, Norris K, Mangione CM. Disparities in the diagnosis and pharmacologic treatment of high serum cholesterol by race and ethnicity:data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2002;162:929–35. doi: 10.1001/archinte.162.8.929. [DOI] [PubMed] [Google Scholar]
- 34.Jha AK, Varosy PD, Kanaya AM, et al. Differences in medical care and disease outcome among black and white women with heart disease. Circulation. 2003;108:1089–94. doi: 10.1161/01.CIR.0000085994.38132.E5. [DOI] [PubMed] [Google Scholar]
- 35.Kerr EA, Smith DM, Hogan MM, et al. Building a better quality measure: are some patients with ‘poor quality’ actually getting good care? Med Care. 2003;41:1173–82. doi: 10.1097/01.MLR.0000088453.57269.29. [DOI] [PubMed] [Google Scholar]
- 36.Nissen D, editor. Mosby's Drug Consult. St. Louis, MO: Mosby, Inc.; 2003. [Google Scholar]
- 37.Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults. Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II) JAMA. 1993;269:3015–23. [PubMed] [Google Scholar]
- 38.Lee TH, Cleeman JI, Grundy SM, et al. Clinical goals and performance measures for cholesterol management in secondary prevention of coronary heart disease. JAMA. 2000;283:94–8. doi: 10.1001/jama.283.1.94. [DOI] [PubMed] [Google Scholar]
- 39.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 40.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 41.Pearson TA, Blair SN, Daniels SR, et al. for the American Heart Association Science Advisory and Coordinating Committee. AHA guidelines for primary prevention of cardiovascular disease and stroke:2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation. 2002;106:388–91. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 42.Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288:455–61. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- 43.Frolkis JP, Pearce GL, Nambi V, Minor S, Sprecher DL. Statins do not meet expectations for lowering low-density lipoprotein cholesterol levels when used in clinical practice. Am J Med. 2002;113:625–9. doi: 10.1016/s0002-9343(02)01303-7. [DOI] [PubMed] [Google Scholar]
- 44.Flocke SA, Stange KC, Goodwin MA. Patient and visit characteristics associated with opportunistic preventive services delivery. J Fam Pract. 1998;47:202–8. [PubMed] [Google Scholar]
- 45.Murray M, Bodenheimer T, Rittenhouse D, Grumbach K. Improving timely access to primary care:case studies of the advanced access model. JAMA. 2003;289:1042–6. doi: 10.1001/jama.289.8.1042. [DOI] [PubMed] [Google Scholar]
- 46.Federman AD, Adams AS, Ross-Degnan D, Soumerai SB, Ayanian JZ. Supplemental insurance and use of effective cardiovascular drugs among elderly Medicare beneficiaries with coronary heart disease. JAMA. 2001;286:1732–9. doi: 10.1001/jama.286.14.1732. [DOI] [PubMed] [Google Scholar]
- 47.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 48.Collins R, Armitage J, Parish S, Sleight P, Peto R. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet. 2004;363:757–67. doi: 10.1016/S0140-6736(04)15690-0. [DOI] [PubMed] [Google Scholar]
- 49.Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]