Abstract
BACKGROUND
Delays in the care of hospitalized patients may lead to increased length of stay, iatrogenic complications, and costs. No study has characterized delays among general medicine inpatients in the current prospective payment era of care.
OBJECTIVE
To quantify and characterize delays in care which prolong hospitalizations for general medicine inpatients.
DESIGN
Prospective survey of senior residents.
SETTING
Urban tertiary care university-affiliated teaching hospital.
PARTICIPANTS
Sixteen senior residents were surveyed regarding 2,831 patient-days.
INTERVENTIONS
None.
MEASUREMENTS AND MAIN RESULTS
Data were collected on 97.6% (2,762) of patient-days eligible for evaluation. Three hundred seventy-three patient-days (13.5% of all hospital days) were judged unnecessary for acute inpatient care, and occurred because of delays in needed services. Sixty-three percent of these unnecessary days were due to nonmedical service delays and 37% were due to medical service delays. The vast majority of nonmedical service delays (84%) were due to difficulty finding a bed in a skilled nursing facility. Medical service delays were most often due to postponement of procedures (54%) and diagnostic test performance (21%) or interpretation (10%), and were significantly more common on weekend days (relative risk [RR], 1.49; P=.02). Indeed, nearly one fourth of unnecessary patient-days (24% overall, 88 patient-days) involved an inability to access medical services on a weekend day (Saturday or Sunday).
CONCLUSIONS
At our institution, a substantial number of hospital days were judged unnecessary for acute inpatient care and were attributable to delays in medical and nonmedical services. Future work is needed to develop and investigate measures to decrease delays.
Keywords: delays, hospital care, quality improvement, hospitalist, length of stay
The length of stay among inpatients in the United States has decreased dramatically as prospective payment reimbursement mechanisms have created incentives to limit the length of hospitalizations.1 However, anecdotal evidence still suggests that a substantial proportion of hospital days are devoted to nonacute care that could be delivered outside of an inpatient setting. These unnecessary days of hospitalization may undermine current efforts to improve quality of care because hospitalized patients are exposed to risks of iatrogenic complications that may result in substantial morbidity and mortality,2 including infections, deconditioning, falls, and deep venous thrombosis. Additionally, unnecessary days may amplify economic pressures to curtail the amount of inpatient care overall, regardless of its necessity. The costs of health care in the United States in 2002 were over $1 trillion, represent approximately 14% of the U.S. gross domestic product, and are estimated to increase to 18% over the next 10 years.3 Because hospital care is the largest segment of annual health care spending in the United States, 3 it is likely that these economic pressures will only increase in the future.
Despite the importance of identifying and mitigating the factors that unnecessarily prolong length of stay, only one report (Selker et al.) has characterized these barriers for general medicine inpatients.4 This retrospective survey was based on data collected in the mid-1980s, when hospital stays were far longer and modes of inpatient care were not greatly influenced by current prospective payment incentives. This report employed an innovative and thorough taxonomy of delays in medical care, and found that approximately one sixth of all hospital days were medically unnecessary. As a quality improvement (QI) initiative, we sought to adapt the conceptual framework of Selker et al. to current modes of inpatient care, using it to characterize and quantify the delays that unnecessarily prolonged hospitalizations at our institution.
METHODS
We prospectively gathered data describing the medical and nonmedical delays that postponed discharge at our university-affiliated tertiary care hospital. Our investigation involved all inpatients on all 8 general medicine teams that were cared for by medical house staff. Four of the house staff teams employed a hospitalist model of inpatient care in which all patients were cared for by the same attending physician. The remaining 4 teams employed a traditional model of care in which patients were cared for by separate attending physicians.
Data Collection
The investigators maintained patient rosters for each of the house staff teams and these were updated daily. Every day, 1 or more members of the investigation team met with each of the 8 senior residents. On weekdays, senior residents were met after their daily educational case-study session (morning report). On weekends, a single member of the study team contacted each senior resident while they were working on the ward. If the senior resident assigned to a particular team was not in the hospital, the senior resident covering for that team was interviewed.
The first day that the survey was employed was timed to coincide with the first day that a new group of senior residents began their rotation on the general medicine wards. A 30-minute tutorial session was provided, during which the QI initiative was explained, the survey tool was introduced, and a series of sample patient scenarios were given. The investigation team then “walked through” sample patient scenarios with senior residents on an individual basis to ensure comprehension.
Survey Instrument
We developed a survey tool to detect, quantify, and characterize delays that unnecessarily prolonged hospitalization. Although this tool was based on the conceptual framework of Selker et al., it was sufficiently different from that instrument to require pilot testing and subsequent modification.4 The pilot testing occurred over a brief period (8 residents, approximately 152 patient-days). It was then employed over 38 consecutive days, between September 25 and November 1, 2002. Data collection for a single resident (with 12 patients, on average) took approximately 5 minutes.
Determining Whether a Delay Occurred
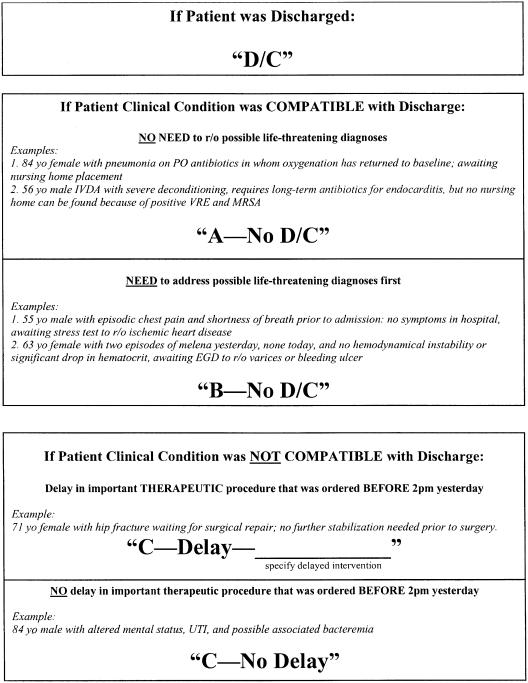
The first page of the survey was designed to determine whether a delay occurred that unnecessarily prolonged hospitalization (Fig. 1). It initially asks about the clinical stability of each patient who was not discharged on the previous day. Clinical status was considered to be compatible with discharge if the patient either 1) had no symptoms, signs, or likely diagnoses that placed the patient at high risk for immediate morbidity or mortality, or 2) had 1 or more of these risks but there was no anticipated risk reduction from hospitalization (e.g., a patient with terminal cancer who was made “comfort measures only”).
Figure 1.
Survey instrument for detecting delays that unnecessarily prolonged hospitalizations by at least 1 day. The first page queries whether a delay occurred, and if so, whether it occurred at a time of possible discharge (coded A-No D/C for nonmedical causes and B-No D/C for medical causes), prior to a time of possible discharge (coded C-Delay), or not at all (coded C-No Delay). The second page was designed to categorize the factors that may have contributed to the delay. The instrument was administered separately for every patient-day (i.e., if a patient was in the hospital for 4 days, his care would have been surveyed 4 separate times).
If a patient's clinical status was compatible with discharge but discharge did not occur, there was potentially a delay in services that prolonged hospitalization. The instrument then inquired about whether there was a medical reason for this delay (e.g., 55-year-old male with episodic chest pain and shortness of breath prior to admission, no symptoms in hospital, awaiting stress test). If the answer to this question was affirmative, the delay was attributed to a postponement of medical services. If the answer to this question was negative, and there was no other apparent medical reason for the delay, it was attributed to a postponement of nonmedical services.
If a patient's clinical status was not compatible with discharge, the instrument then inquired as to whether there was a delay in an intervention that was likely to stabilize the patient (e.g., 71-year-old female with hip fracture cleared for surgery and awaiting surgical repair). We sought to capture these types of delays even though they did not occur at the point of discharge because they may have prolonged hospitalizations by postponing all subsequent events in the stream of care, including the time of discharge.
We instructed the respondents to code conservatively, so that if there was uncertainty about whether a delay was responsible for unnecessary prolongation of length of stay, it was not considered to be responsible. Finally, a postponement in a needed service was only considered a delay if it was ordered at least 1 calendar day prior to the day in question (for services requiring overnight preparation, such as surgical procedures or colonoscopies) or if it was ordered by 2 PM of the day in question (for services that did not require extensive preparation, such as parenteral IV catheter [PICC] line placement).
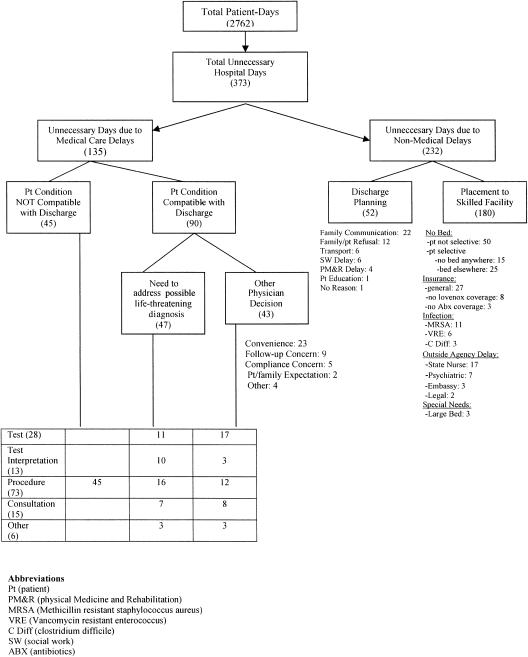
Categorizing Delays
The second page of the survey was only completed if a delay was detected. This section gathered additional information that permitted us to partition care delays in care into 6 mutually exclusive categories using the taxonomy based on Selker et al. Possible medical delays were 1) diagnostic test performance (e.g., stress test, magnetic resonance [MRI], endoscopic retrograde cholangiopancreatography [ERCP], Doppler), 2) diagnostic test interpretation, 3) procedure (e.g., surgery, thoracentesis, ERCP, dialysis), and 4) consultation. Possible nonmedical delays were 5) discharge planning (e.g., arranging transportation), and 6) discharge destination unavailable (e.g., lack of nursing facility beds).
We excluded 3 of the categories in the taxonomy of Selker et al. because they are rarely applicable to current modes of inpatient care. First, we excluded the category of delays due to house staff education or awaiting the start of a research protocol, because under prevailing financial pressures at the current time, patients are seldom retained in the hospital solely for the purpose of education. Second, we excluded the category of delays due to “physician responsibility,” which included “political” admissions and patients retained for convenience. Last, we excluded the category of delays related to patient indecision or refusal of a procedure, because these decisions are the right of the patient, and are overall outside the control of the physician.
In addition to determining whether delays led to untimely postponements of discharge and to categorizing them, the second part of the survey also gathered more detailed information about the environment in which selected types of care delays occurred, including subcategories of 1) concern about follow-up by the health system, 2) concern about follow-up compliance by the patient, 3) convenience of having the patient in the hospital in order to obtain a medical intervention that could be done on an outpatient basis, or 4) demand or expectation by patient or family.
Associations of Delays with Other Factors
We tested two prespecified hypotheses: 1) there would be a greater proportion of unnecessary hospital days on weekends compared to weekdays, and 2) there would be more delays when the hospital census was higher. These hypotheses were based on anecdotal evidence at our institution suggesting that significant delays in care were more common at these times.
We also hoped to test the hypothesis that the hospitalist model of care would decrease the likelihood of unnecessary days compared to the traditional model of care. However, restrictions on the maximum numbers of admissions to on-call teams resulted in some patients with nonhospitalist attending physicians being assigned to hospitalist house staff teams, and vice versa. Because this overflow was not tracked prospectively and may have been unbalanced, we were unable to compare the frequency of delays for hospitalist versus nonhospitalist models of inpatient care.
Statistical Methods
The χ2 test was used to compare the proportion of unnecessary days on weekend days versus weekdays. A univariate linear regression model was used to determine whether the proportion of unnecessary hospital days attributable to delays in care (dependent variable) was associated with the proportion of beds filled (independent variable).
RESULTS
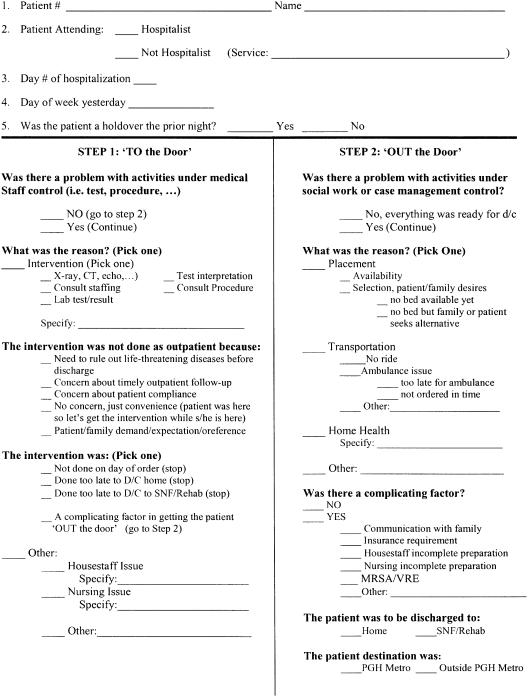
We collected information describing the delays in care that prolonged hospitalizations for all patients admitted to general medicine services over a consecutive period. Surveys were completed on 97.6% (2,762) of the 2,831 patient-days that were eligible for evaluation. We identified a total of 373 patient-days that were judged unnecessary for acute inpatient care and were attributable to delays in needed services (13.5% of all hospital days). Of this total, 63% (232 patient-days) involving 89 patients were due to nonmedical causes, and 37% (135 patient-days) involving 62 patients were due to medical causes. The breakdown of unnecessary days is shown in Fig. 2. Among the 1,001 days accrued by patients that had clinical stability compatible with discharge, 322 (32.2%) were not discharged on that day. Of the 151 patients who had delays, 64 (42%) experienced only 1 unnecessary day. The hospital's average daily occupancy rate during this period was 90.1%. The average length of stay for a medical admission at this hospital was 5.5 days.
Figure 2.
Distribution of unnecessary hospital days. Causes are divided into medical and nonmedical groupings. Each number that follows a cause refers to the number of patient-days that were judged attributable to that cause. Six of the days could not be categorized. Pt, patient; PM&R, physical medicine and rehabilitation; MRSA, methicillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant enterococcus; C Diff, clostridium difficile; SW, social work; ABX, antibiotics.
Nonmedical Delays
Of the 232 unnecessary patient-days that were judged to be attributable to nonmedical delays, the vast majority (N = 180, 84%) were due to difficulty finding a bed in a skilled nursing facility. Of this group, 50 were due to a nonavailability of any bed at a facility within the geographic region, and 40 were due to patient or family requesting a specific facility. The remaining 90 patient-days were attributable to unavailability of isolation beds required by infections with resistant organisms (20), delays in insurance approval (38), delays imposed by an outside agency (29), or other patient special needs (3).
The 52 patient-days unrelated to finding a bed in a skilled nursing facility were attributable to delays in discharge planning. This group included lack of communication with family (22), family or patient refusal to be discharged (12), problems with transport (6), house staff or social worker delay (6), delay by a physical medicine and rehabilitation team approving specific placement (4), delay in patient education (1), and no reason identified (1).
Medical Delays
Of the 135 unnecessary patient-days that were judged to be attributable to medical delays, 73 (54%) were due to delays in procedures, 28 (21%) were due to delays in test performance, 15 (11%) were due to delays in consultations, 13 (10%) were due to delays in test interpretation, and 6 (4%) were attributable to other causes. The majority of these delays (67%) occurred among patients with clinical stability compatible with discharge. The types of delayed procedures that most frequently caused unnecessary patient-days were surgeries (27), stress testing (14), ERCP (8), PICC line placements (8), cardiac catheterizations (6), and lower extremity Doppler exam (6). Particular subspecialties accounted for disproportionate shares of the delays, as shown in Table 1. Of the 135 patient-days, 34 were incurred by surgical services (25.2%), 29 by radiology (21.5%), 24 by cardiology (17.8%), and 16 by gastroenterology (11.9%).
Table 1.
Distribution of Medical Service Delays
| Medical Delays Breakdown | ||||||
|---|---|---|---|---|---|---|
| Consults | Interpretation | Procedure | Test | Miscellaneous | Totals | |
| Surgery | Neurosurgery (3) | CT surgery (1) | Ortho surgery (9) | 34 | ||
| GI surgery (2) | Vasc surgery (7) | |||||
| Ortho surgery (1) | Gen surgery (6) | |||||
| CT surgery (3) | ||||||
| GI surgery (2) | ||||||
| Radiology | MRI (2) MRA (1) | PICC (8) | Dopplers (6) | 29 | ||
| I131 Ablation (4) | MRI (3) | |||||
| Thoracentesis (1) | MRCP (1) RUQ U/S (1) | |||||
| Peritoneal catheter (1) | C-spine films (1) | |||||
| Cardiology | Stress test (1) | Cath (6) TEE (2) | Stress test | 24 | ||
| (9) Stress echo (5) | ||||||
| Echocardiogram (1) | ||||||
| GI | ERCP (8) | Dysmotilty study (1) | 16 | |||
| EGD (3) | ||||||
| Enteroscopy (2) | ||||||
| FEES (2) | ||||||
| Miscellaneous | Pulmonary (3) | Pathology (6) [Duod bx, 2; BM bx, 1; other, 3] | Renal (3) [Dialysis] | Pharmacy (2) [late BP meds] | Pulmonary (7) | |
| Psychiatry (2) | Lab result (2) | Pulm (4) [Bronch] | Blood bank (1) [late transfusion] | Pathology (6) | ||
| Transplant (2) | Electrolytes Blood culture | ENT (1) | Nursing (2) [24-hr calorie count, 1; | Renal (3) | ||
| Neurology (1) Heme/Onc (1) | Ophthalmology (1) | Start tube feeds, 1] Unspecified (1) | Psychiatry (2) | |||
| Transplant (2) | ||||||
| Lab (2) | ||||||
| Pharmacy (2) | ||||||
| Nursing (2) | ||||||
| Heme/Onc (1) | ||||||
| Neurology (1) | ||||||
| ENT (1) | ||||||
| Ophthalmology (1) | ||||||
| Blood bank (1) | ||||||
| Unspecified (1) | ||||||
| Totals | 15 | 13 | 73 | 28 | 6 | 135 |
Each number refers to the quantity of unnecessary patient-days that were judged to be attributable to that delay.
ENT, ear, nose & throat; Heme/Onc, hematology/oncology; Pulm, pulmonary; Ortho surgery, orthopedic surgery; GI surgery, gastroenterological surgery; Vasc surgery, vascular surgery; CT surgery, cardiothoracic surgery; Gen surgery, general surgery.
FEES, fiberoptic enteroscopic study; EGC, esophagogastroduodenoscopy; ERCP, endoscopic retrograde cholangiopancreatography; MRCP, magnetic resonance cholangiopancreatogram; MRI, magnetic resonance; MRA, magnetic resonance angiogram; RUQ U/S, right upper quadrant ultrasound; C-spine, cervical spine; PICC, parenteral IV catheter; Stress Echo, stress echocardiogram; Perit cathether, peritoneal catheter; I131 ablation, iodine 131 ablation.
BM Bx, bone marrow biopsy; Duod Bx, duodenal biopsy; U/S Interp, ultrasound interpretation; Cath, cardiac catheterization.
BP, blood pressure.
Association of Delays with Day of Week and Hospital Census
Delays occurred more frequently on weekend days (17.1%) than weekdays (12.6%), a risk ratio (RR) of 1.36 (P =.01). The weekend predominance was more pronounced for medical delays (RR, 1.49; P =.02) than for nonmedical delays (RR, 1.08; P =.40). Weekend delays were more common on Sundays (20.3% of patient-days) than Saturdays (13.6% of patient-days). Among weekdays, delays were most common on Mondays (15.9%). No relationship of delay frequency with hospital census was apparent (P =.105).
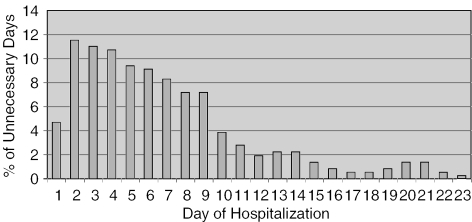
Timing of Delays
Only 17 patient-days judged to be unnecessary (4.6% of the total) occurred on the first hospital day. The highest number (42 patient-days) occurred on the second hospital day (11.2% of total). High proportions also occurred on the third and fourth hospital days (10.7% and 10.4% of total, respectively), after which there was a more rapid decline (Fig. 3). The ninth hospital day was the last day with substantial (>5% of total) numbers of unnecessary patient-days.
Figure 3.
Timing of unnecessary hospital days. Each bar shows the percentage of unnecessary patient-days occurring on each day of hospitalization.
DISCUSSION
Our QI investigation found that 13.5% of all hospital days were judged unnecessary for acute inpatient care and occurred only because of delays in needed services. Of these unnecessary hospital days, the majority (63.2% of unnecessary days, and 8.5% of hospital days overall) were attributable to either delays in discharge planning or placement in a skilled facility. A substantial minority (36.8% of unnecessary days, and 5.0% of days overall) were due to delays in medical care including test performance, test interpretation, procedures, and consultations.
It is interesting to note that although hospital lengths of stay have decreased markedly in the past 20 years, and were 60% longer in the study of Selker et al. than in ours, the proportion of hospital days judged unnecessary for acute inpatient care may have changed comparatively little. Selker et al.4 found that similar proportions of days were unnecessary for acute inpatient care (15.1% using the delay categories in the current study, and 16.6% using all the delay categories in their instrument). Additionally, there may have been little change in the proportion of unnecessary days resulting from nonmedical delays (63% vs 59%, current study versus Selker et al., respectively), and in the proportion of nonmedical delays that result from difficulty finding nursing home placement (84% versus 84%, current study vs Selker et al., respectively). One possible interpretation of this similarity is that while changing economic incentives have increased the pressure to overcome barriers to timely discharges, there has been little systematic effort to remediate the root causes of these barriers (i.e., limited access to diagnostic tests on weekends, limited efforts to establish an efficient clearinghouse to match patient needs with nursing facility bed availability), and therefore most persist, albeit in ameliorated form.
Although Selker et al. and the present study are the only two published reports quantifying and categorizing delays for general medicine inpatients, other reports have quantified delays in care for nonmedical services, or have sought to determine the proportion of hospital days that were “inappropriate,” regardless of whether these resulted from delays in care. Brasel et al.5 sought to identify discharge delays among surgical trauma patients, and 6.7% of hospital days overall were attributable to delays in discharge planning, a result generally consistent with our result of 8.5%. There have been utilization review studies over the past 20 years using disparate tools,6–9 many of which are proprietary and most of which are designed for retrospective assessment. The Appropriateness Evaluation Protocol (AEP), which was first described by Gertman and Restuccia in 1981,8 has been the most frequently used of such tools. In 1994, Baigelman et al.9 performed a prospective study on medical patients that used the AEP criteria to determine “inappropriate” days. This study determined that 49.7% of total days were inappropriate, 20% of these days (9.9% overall) were caused by problems in discharge planning or awaiting placement, and it attributed between 60% and 70% of unnecessary days to physician decision. In a more recent review article, McDonagh et al.10 found that inappropriate days for a general adult medical population using the retrospective tools have ranged from 5.5% to 62% of all hospital days.
The motivation for our QI initiative was to identify causes for unnecessary inpatient-days that would be amenable to improvement. We identified 2 main care processes at our hospital as candidates for potential improvement. First, nearly half of all unnecessary inpatient-days were attributable to delays in the achievement of placement in a skilled facility, and more than half of all unnecessary days occurred after the fourth hospital day. This suggests that our discharge planners have sufficient time to anticipate and address barriers to nursing facility placement before these barriers act to postpone the time of discharge. Therefore, we are working to streamline the care management process by matching specific patient needs with available beds earlier in the course of hospitalization, as well as working to partner with area facilities to increase overall bed availability in the region. These efforts will build upon care processes that were motivated by utilization review studies and are now commonplace, including case management teams,11 discharge planning systems,12,13 and hospitalist physicians.14–16 Our hospital has utilized case managers for several years, and already employs a hospitalist program, suggesting that these processes of care must be supplemented by new measures if the aim is to further decrease the number of unnecessary hospital days.
Second, nearly one fourth of unnecessary inpatient-days (24% overall, 88 patient-days) involved an inability to access medical services on a weekend day (Saturday or Sunday), when surgical and procedural services staffs are lean. In addition, the demand for services that accumulated over the weekend was sufficiently high to saturate weekday service capacities, as evidenced by the unusually large number of delays on Mondays compared to other weekdays. Because of these results, we are working with the hospital administration to increase service availability at these times. There are data from other institutions also suggesting that delays in medical care during weekends are an important factor impacting care processes. Varnava et al.,17 in a study of 2,541 patients with acute myocardial infarction admitted to the coronary care unit, found that day of the week had a significant effect on length of stay. In this study, discharges occurred most often on a Friday (P =.006) and least often over the weekend (P =.001).
Limitations
Our investigation has several limitations. It was performed at a university-affiliated tertiary care hospital and therefore results may not be generalizable to other settings. It was performed over a brief time period, and therefore secular trends that vary over a calendar year may not be reflected in the results. Also, it is likely that we underestimated the actual number of unnecessary hospital days, because we only detected those attributable to delays, and the design of our survey excluded from consideration those delays that were attributable to the primary team. Some imprecision may have been introduced by relying on the judgment of medical trainees rather than attending physicians. Last, the reliability and validity of the instrument used to categorize delays in care has not been established. However, our investigation remains the only prospective study of delays in care among general medicine inpatients, and the only one that has been conducted in the current era of inpatient care.
Conclusion
We found that a substantial number of hospital days were judged unnecessary for acute inpatient care and were attributable to delays in medical and nonmedical services. The proportion of unnecessary hospital days due to delays in our institution did not differ greatly from the only other study that has examined this outcome in a similar patient population, even though the other study was conducted before prospective payment-based incentives began to have a strong impact. These unnecessary inpatient-days may needlessly increase the exposure of patients to iatrogenic infections and other complications, as well as decrease economic efficiency. Future work is needed to develop and evaluate the effectiveness of measures to decrease delays in inpatient care.
Acknowledgments
This work was supported by funds allocated by the University of Pittsburgh Medical Center for quality improvement initiatives.
REFERENCES
- 1.Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality, and costs. J Am Geriatr Soc. 2003;51:364–70. doi: 10.1046/j.1532-5415.2003.51110.x. [DOI] [PubMed] [Google Scholar]
- 2.Shojania KG, Duncan BW, McDonald KM, Wachter RM. Safe but sound: patient safety meets evidence-based medicine. JAMA. 2002;288:508–13. doi: 10.1001/jama.288.4.508. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare and Medicaid Services. US Health Care System. Available at: http://www.cms.hhs.gov/charts/default.asp. Accessed January 2004.
- 4.Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital. Med Care. 1989;27:112–29. doi: 10.1097/00005650-198902000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Brasel KJ, Rasmussen J, Cauley C, Weigelt JA. Reasons for delayed discharge of trauma patients. J Surg Res. 2002;107:223–6. doi: 10.1006/jsre.2002.6512. [DOI] [PubMed] [Google Scholar]
- 6.Gertman PM, Restuccia JD. The appropriateness evaluation protocol: a technique for assessing unnecessary days of hospital care. Med Care. 1981;19:855–71. [PubMed] [Google Scholar]
- 7.The InterQual Review System. Marlborough, MA: InterQual Products Group; 1996. [Google Scholar]
- 8.The Managed Care Appropriateness Protocol. Wellesley, MA: Oak Group; 1996. [Google Scholar]
- 9.Baigelman W, Weld L, Coldiron JS. Relationship between practice characteristics of primary care internists and unnecessary hospital days. Am J Med Qual. 1994;9:122–8. doi: 10.1177/0885713X9400900304. [DOI] [PubMed] [Google Scholar]
- 10.McDonagh MS, Smith DH, Goddard M. Measuring appropriate use of acute beds: a systematic review of methods and results. Health Policy. 2000;53:157–84. doi: 10.1016/s0168-8510(00)00092-0. [DOI] [PubMed] [Google Scholar]
- 11.D'Addario V, Curley A. How case management can improve the quality of patient care. Int J Qual Health Care. 1994;6:339–45. doi: 10.1093/intqhc/6.4.417-a. [DOI] [PubMed] [Google Scholar]
- 12.Evans RL, Hendricks RD. Evaluating hospital discharge planning: a randomized clinical trial. Med Care. 1993;31:358–70. doi: 10.1097/00005650-199304000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Tennier LD. Discharge planning: an examination of the perceptions and recommendations for improved discharge planning at the Montreal General Hospital. Soc Work Health Care. 1997;26:41–60. doi: 10.1300/J010v26n01_03. [DOI] [PubMed] [Google Scholar]
- 14.Halpert AP, Pearson SD, LeWine HE, Mckean SC. The impact of an inpatient physician program on quality, utilization, and satisfaction. Am J Manag Care. 2000;6:549–55. [PubMed] [Google Scholar]
- 15.Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627–32. doi: 10.1016/s0002-9343(01)00976-7. [DOI] [PubMed] [Google Scholar]
- 16.Davis KM, Koch KE, Harvey JK, Wilson R, Englert J, Gerard PD. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Am J Med. 2000;108:621–6. doi: 10.1016/s0002-9343(00)00362-4. [DOI] [PubMed] [Google Scholar]
- 17.Varnava AM, Sedgwick JE, Deaner A, Ranjadayalan K, Timmis AD. Restricted weekend service inappropriately delays discharge after acute myocardial infarction. Heart. 2002;87:216–9. doi: 10.1136/heart.87.3.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–8. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]