Abstract
After treatment in an emergency department (ED), patients often wait several hours for hospital admission, resulting in dissatisfaction and increased wait times for both admitted and other ED patients. We implemented a new direct admission system based on telephone consultation between ED physicians and in-house hospitalists. We studied this system, measuring admission times, length of stay, and mortality. Postintervention, admission times averaged 18 minutes for transfer to the ward compared to 2.5 hours preintervention, while pre- and postintervention length of stay and mortality rates remained similar.
Keywords: patient admission, emergency medicine, hospitalist
Emergency department (ED) visits and patient acuity have steadily increased throughout the last decade, leading to a greater percentage of patients admitted to the hospital.1 Correspondingly, ED congestion and length of stay (LOS) have worsened, with admitted patients often waiting several hours for transfer out of the ED after treatment.1,2 In addition to dissatisfying patients, this also increases the LOS of ED “treat-and-release” patients.3 Many hospitals rely on physician staff from departments outside of the ED, or “consultants,” to evaluate and admit patients from the ED, contributing to admission delays.4 Removing consultants from the process and having the ED triage and transfer patients directly to inpatient hospital services can reduce admission delays.4 This strategy precludes what may be valuable input from consultants prior to the admission. Hospitalists may represent a solution to this problem; the use of hospitalists (inpatient-based attending physicians) has exploded recently, with 5,000 practicing in the United States currently and an estimated 20,000 practicing in 10 years.5 Using hospitalists, we designed an admission process that combines the advantages of consultant participation with that of rapid direct admissions. This is accomplished by having ED physicians admit patients directly to the general medical unit after a telephone consultation with a hospitalist. We evaluate this process using a prepost comparison of the time from ED decision to admit a patient until the time the patient arrived on the medical service (hereafter called “admission cycle time”), hospital LOS, and in-hospital mortality rates.
METHODS
Setting
Johns Hopkins Bayview Medical Center (JHBMC) is a 706-bed teaching hospital serving a population of >300,000 people. Over 12,000 ED patients are admitted annually, more than half to the department of medicine (DOM).
Design
This study is an observational double-cohort study, with pre- and postintervention cohorts.
Sample
Preintervention admission cycle times were measured for all patients in November 1997. Preintervention patient mortality and LOS were measured for all evaluated patients discharged from the medical services that had been admitted through the ED for calendar year 1998 (total ED visits = 41,180; admitted patients = 5,766). After the new triage and admission system was begun, admission cycle times were monitored for all patients during January and February 2000. Postintervention patient mortality and LOS were measured for calendar year 2000 (total ED visits = 47,906; admitted patients = 8,210).
Measures
Mortality and LOS data were extracted from ongoing medical center performance improvement databases. An administrator monitored admission cycle times via tracking forms completed by ED staff, and monitored DOM physician evaluation of patients after arrival on the wards via chart review. Patients whose admission decision was made during periods when inpatient beds were unavailable were excluded from analysis. Given the relationship between lack of inpatient bed availability and ED overcrowding, the percentage of time that inpatient beds were unavailable in pre- and postintervention time periods was estimated from the proportion of “yellow alert” hours, when ED beds were unavailable and the ED was on diversion.6,7
Data Analysis
Pre- and postintervention mortality rates were compared using the χ2 for difference in proportions. Inpatient LOS was compared for the pre- and postintervention groups using Student's t test. Case mix index using APR-DRG, a widely used severity of illness and risk of mortality adjustment, was also compared for the pre- and post- groups to allow better interpretation of any differences in mortality or LOS.8
Intervention
Prior to our intervention, the ED to medicine admission process was as follows:
Once the ED attending decided to admit a patient to general medicine, s/he paged the medical resident for admission. The medicine resident evaluated the patient in the ED and s/he wrote admitting orders. The patient then left the ED. The DOM and the ED collaborated to design the following new triage and admission system: The ED attending upon deciding to admit a patient pages an admission pager to discuss the case with the hospitalist. The hospitalist reviews the case by telephone and documents pertinent data on an admission form. Once the hospitalist accepts the admission, the ED attending writes brief admitting orders on a preprinted admission order sheet. Upon arriving at the medical unit, the patient's location is paged to the admission pager, initiating an evaluation by the appropriate medical service. Monthly meetings occur between the DOM and the ED to discuss improvements to the admission process.
RESULTS
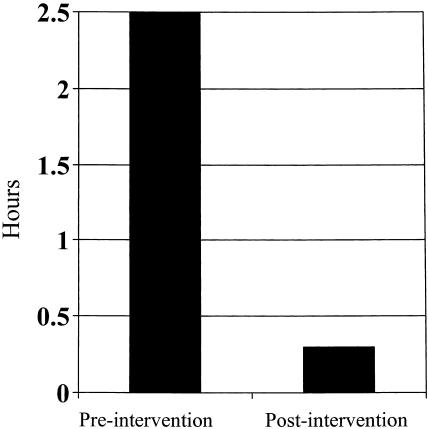
Prior to the intervention, beds were available approximately 82% of the time; the admission cycle time during these hours averaged 2 hours and 27 minutes. After the intervention, beds were available approximately 62% of the time, with average admission cycle times of only 18 minutes (Fig. 1). In the postintervention period, time until DOM physician evaluation averaged 20 minutes after patient arrival on the medical ward. Mortality rates prior to and after the intervention were similar: 3.54% and 3.58%, respectively (difference, 0.04%; 95% confidence interval, 0.037 to 0.043). The postintervention LOS of 4.15 days was slightly more than the 3.98-day LOS prior to our intervention (difference, 0.17 days; 95% confidence interval, 0.01 to 0.34). The case mix index for patients admitted from the ED and discharged from the Medicine services was 2.3 both pre- and postintervention. For comparison, hospital-wide LOS for all services was 4.3 days preintervention and 4.5 days postintervention. The LOS for the same time periods excluding the study population from analysis was 5.3 days preintervention and 5.5 days postintervention.
FIGURE 1.
Medical admission cycle times, in hours, pre- and postintervention.
DISCUSSION
A new hospitalist triage and admission intervention for medical patients admitted from the ED reduced admission times by more than 2 hours when a bed was available, and was not associated with increased mortality. The 0.17% increase in LOS seen in our study was accompanied by a similar increase hospital wide, even when our study population was excluded from the analysis. Therefore, we doubt that it was related to the new triage and admission process. Increasing severity of illness was not the cause as captured by the unchanged case mix index, both for Medicine patients admitted through the ED and hospital wide. One possibility is that inappropriate admissions, which are usually brief, were reduced. Another possibility is that interventions previously done in the ED are now being done on the inpatient side, thus inflating LOS. Another possibility that would account for the hospital-wide LOS increase is nursing shortages in the more recent years, causing delays in discharge.
To ensure accurate measurement of the intervention, our study was designed to measure the new triage system without the confounding factor of bed availability. Therefore, we excluded data when the hospital had no available beds. We recognize that bed availability may be an even more significant factor in admission delays in some hospitals. We estimated that our hospital had open beds approximately 61% postintervention, yet the new admission process is a major improvement in ED patient flow despite its effectiveness only during times of available inpatient beds. Its usefulness in other settings will depend on inpatient bed availability. An additional, unexpected benefit is that the regular communication between the ED attendings and the DOM hospitalists fostered greatly improved working relationships between the departments and a more rewarding work environment.
A few notable limitations constrain our study conclusions. First, our database is from an administrative database and not specifically designed for medical research. Although clinical aspects of these data such as diagnoses have often been shown to be inaccurate, mortality rates and LOS are generally considered to be accurate. The administrative case mix index using APR-DRG, a widely used severity of illness and risk of mortality adjustment, is only a proxy for illness severity and there may have been unmeasured differences. However, we have no reason to suspect that these inaccuracies conferred bias that would affect the comparison between our 2 groups. Second, although we examined case mix index, this study does not account for other factors that might affect LOS or mortality independently of the studied admission process. Third, we had control groups only for mortality and LOS that would allow us to compare our study patients to others throughout the hospital; we had no control group for admission cycle times except for the pre- and postintervention comparison. Fourth, we have not examined ED throughput of patients that were not admitted, which may be improved by this intervention as suggested by other authors, and would be of great interest to ED directors. Fifth, the frequency of bed unavailability was estimated from yellow alert hours rather than directly measured. Periods when beds were not open were excluded from our study, and patient admission cycle times during these periods may have been markedly greater than those measured. Finally, we did not examine whether our intervention affected resident education. Transferring the responsibility of triage from the admitting resident to the hospitalist and shifting the initial inpatient evaluation from the ED to the medical ward is a change from the more traditional admission and triage process. One could argue that by removing the resident from triage duty, they lose tools needed to learn important skills. This would be an important area for future study.
In conclusion, using hospitalists, we have developed a safe and efficient admission process that significantly reduces ED admission cycle times.
REFERENCES
- 1.Meggs WJ, Czaplijski T, Benson N. Trends in emergency department utilization. Acad Emerg Med. 1999;6:1030–5. doi: 10.1111/j.1553-2712.1999.tb01188.x. [DOI] [PubMed] [Google Scholar]
- 2.Andrulis DP, Kellermann A, Hintz EA, Hackman BB, Weslowski VB. Emergency departments and crowding in the United States teaching hospitals. Ann Emerg Med. 1991;20:980–6. doi: 10.1016/s0196-0644(05)82976-2. [DOI] [PubMed] [Google Scholar]
- 3.Bazarian JJ, Schneider SM, Newman VJ, Chodosh J. Do admitted patients held in the emergency department impact the throughput of treat-and-release patients? Acad Emerg Med. 1996;3:1113–8. doi: 10.1111/j.1553-2712.1996.tb03370.x. [DOI] [PubMed] [Google Scholar]
- 4.Quick G. Time analysis of consult service emergency department admission process compared with emergency medicine service admission process. J Emerg Med. 1999;17:815–22. doi: 10.1016/s0736-4679(99)00088-8. [DOI] [PubMed] [Google Scholar]
- 5.Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287:487–94. doi: 10.1001/jama.287.4.487. [DOI] [PubMed] [Google Scholar]
- 6.Schneider SM, Gallery ME, Schafermeyer R, Zwemer FL. Emergency department crowding: a point in time. Ann Emerg Med. 2003;42:181–4. doi: 10.1067/mem.2003.258. [DOI] [PubMed] [Google Scholar]
- 7.Schull MJ, Lazier K, Vermeulen M, Mawhinney S, Morrison LJ. Emergency department contributors to ambulance diversion: a quantitative analysis. Ann Emerg Med. 2003;41:477–80. doi: 10.1067/mem.2003.23. [DOI] [PubMed] [Google Scholar]
- 8.Freeman JL, Fetter RB, Park H, et al. Diagnosis-related group refinement with diagnosis- and procedure-specific comorbidities and complications. Med Care. 1995;33:806–27. doi: 10.1097/00005650-199508000-00006. [DOI] [PubMed] [Google Scholar]