Abstract
BACKGROUND
As a result of market forces and maturing technology, generalists are currently providing services, such as colonoscopy, that in the past were deemed the realm of specialists.
OBJECTIVE
To determine whether there were differences in patient characteristics, procedure complexity, and clinical indications when gastrointestinal endoscopic procedures were provided by generalists versus specialists.
DESIGN
Retrospective cohort study.
PATIENTS
A random 5% sample of aged Medicare beneficiaries who underwent rigid and flexible sigmoidoscopy, colonoscopy, and esophagogastroduodenoscopy (EGD) performed by specialists (gastroenterologists, general surgeons, and colorectal surgeons) or generalists (general practitioners, family practitioners, and general internists).
MEASUREMENTS
Characteristics of patients, indications for the procedure, procedural complexity, and place of service were compared between generalists and specialists using descriptive statistics and logistic regression.
MAIN RESULTS
Our sample population had 167,347 gastrointestinal endoscopies. Generalists performed 7.7% of the 57,221 colonoscopies, 8.7% of the 62,469 EGDs, 42.7% of the 38,261 flexible sigmoidoscopies, and 35.2% of the 9,396 rigid sigmoidoscopies. Age and gender of patients were similar between generalists and specialists, but white patients were more likely to receive complex endoscopy from specialists. After adjusting for patient differences in age, race, and gender, generalists were more likely to have provided a simple diagnostic procedure (odds ratio [OR] 4.2; 95% confidence interval [95% CI] 4.0, 4.4), perform the procedure for examination and screening purposes (OR 4.9; 95% CI, 4.3 to 5.6), and provide these procedures in rural areas (OR 1.5; 95% CI 1.4 to 1.6).
CONCLUSIONS
Although generalists perform the full spectrum of gastrointestinal endoscopies, their procedures are often of lower complexity and less likely to have been performed for investigating severe morbidities.
Keywords: colonoscopy, esophagogastroduodenoscopy, sigmoidoscopy, generalist physician, specialist, physician practice patterns
Generalists are currently providing services that in the past were deemed the realm of specialists, particularly in the rural, fee-for-service environment. Gastrointestinal procedures are particularly noteworthy because of significant advances in technology and the incorporation of instruction on gastrointestinal endoscopy into generalist training programs and continuing medical education courses.1–3 The first procedures to be adopted by generalists were rigid and flexible sigmoidoscopies, but more complex and technically demanding endoscopic procedures such as esophagogastroduodenoscopy (EGD) and colonoscopy are now being performed by generalists.4,5 In a study of procedures performed by general internists, 74% performed rigid sigmoidoscopies, 42% performed flexible sigmoidoscopies, 7% performed EGDs, and 3% performed colonoscopies.6 A Washington State survey of family practitioners found that over 50% performed flexible sigmoidoscopies, and many of those not performing them planned to integrate them into future practice.7 The trend toward integrating increasingly complex procedures into generalist practice (e.g., offering full colonoscopy in addition to flexible sigmoidoscopy) is expected to continue.3
The safety and efficacy of rigid and flexible sigmoidoscopy performed by generalist physicians is now well established and has been included in many comprehensive cancer screening programs for over a decade.8 Studies of EGD use by generalists from the Military Health Services System,9 rural practice groups,10 and university-based clinics11 suggest that EGDs can be performed by well-trained generalists with low complication rates and good diagnostic efficacy.12,13 Case series suggest that family practitioners can perform colonoscopy safely14 and usually can visualize the full colon without significant complications.15–18 Gastroenterological specialty societies, however, have questioned whether it is wise to expand the performance of gastrointestinal procedures by generalists, particularly in the cases of colonoscopy and EGD.18 In 1992, two prominent gastroenterological societies sent letters to hospital administrators suggesting that their institutions were at considerable risk if they granted endoscopy privileges to generalist physicians.19
The resolution of the controversy surrounding the diffusion of “specialist” procedures into the generalist domain requires a thorough understanding of the characteristics of the services delivered, the population that received them, and the outcomes achieved by the two provider groups. Previous studies have failed to investigate whether there may be important differences in the types of patients, health of the patients, diagnostic indications for the procedures, or complexity of the procedures performed by generalist and specialist providers. We examined the characteristics of the gastrointestinal endoscopies and the patients who received them to identify differences between the practices of generalists and specialists that should be taken into account in future outcomes studies.
METHODS
We analyzed a random 5% sample of Medicare beneficiaries listed in the 1993 Medicare National Claims History File. Patients under the age of 65 years, patients whose claims were disallowed, and patients whose claims were for services provided outside the continental United States, Alaska, and Hawaii were excluded. In addition, patients who were enrolled in a Medicare health maintenance organization at any time during 1993 were excluded because of incomplete claims reporting under that program.20 This resulted in a final sample of 1,369,179 Medicare beneficiaries.
Claims Data
We selected claims for gastrointestinal endoscopies using the Physicians' Current Procedural Terminology-4 (CPT ) codes: esophagogastroduodenoscopy (EGD) (43200–43272), rigid sigmoidoscopy (45300–45321), flexible sigmoidoscopy (45330–45337), and colonoscopy (45355–45385).21 The abstracted Medicare claims included demographic data on the patients, diagnostic codes in the International Classification of Diseases, Ninth Revision Clinical Modification(ICD-9-CM),22 a self-designated physician specialty code, and the physician's unique provider identification number (UPIN).23 Each of the procedures was further classified as to whether it was performed as a diagnostic procedure alone or accompanied by another service such as biopsy, polypectomy, or other therapeutic intervention (e.g., removal of a foreign body). Diagnostic indications for the procedure were grouped into a limited number of categories by using a modification of the Agency for Health Care Policy and Research's Clinical Classifications for Health Policy Research.24 Specialties providing less than 1% of these procedures were excluded, leaving three specialist groups (gastroenterology, general surgery, and colorectal surgery) and three generalist groups (general internal medicine, family practice, and general practice) in our sample. For some analyses, the groups were collapsed into 4 specialty groups (gastroenterologists, surgeons, general internists, and family/general practitioners). Medicare data were merged with county-level health care resource and population information from the 1993 Area Resource File (ARF) to place the provision of services in a geographic and demographic context.25,26
Physician Specialty Designation
Because accurate specialty designation was essential to our analyses, we used 2 complementary data sources to designate physician specialty: (1) the self-designated physician specialty code in the Medicare data and (2) information on self-designated primary and secondary specialties, training histories, and board certification from the American Medical Association (AMA) Physician Masterfile.27 The latter was linked to the Medicare data via the UPIN. This comprehensive approach to specialty classification avoided mislabeling of physicians and ensured that generalists performing gastrointestinal endoscopy did not differ in training or board certification from other generalists.
Analyses
Descriptive statistics of patient and provider characteristics, the distribution of these procedures, and diagnostic indications were generated. Logistic regression was performed to examine the independent differences in characteristics of patients and procedures controlling for the effects of age, gender, and race. All statistical analyses were performed using the Stata statistical package.28
RESULTS
Physician Specialty Designation
A total of 44,031 physicians performed 167,347 gastrointestinal endoscopies on our sample population. There was some discordance in specialty self-designation between the Medicare data and the AMA Physician Masterfile. The agreement of the 2 sources for provider specialty codes was 31% for general practice, 87% for family practice, 62% for general internal medicine, 95% for gastroenterology, 85% for general surgery, and 94% for colorectal surgery. In most discordant cases, the specialty designation reported to the AMA was more specialized than that reported to Medicare. For example, of the 29% of Medicare-designated general internists who reported another specialty to the AMA, 86% were gastroenterologists.
Because of the disagreements on self-designated physician specialty codes, we created a composite specialty designation based on a hierarchical synthesis of information from the AMA Physician Masterfile and Medicare data. The highest level of evidence for specialty designation was board status. Of the 44,031 physicians, 20.4% were board certified in general surgery, 3.9% in colorectal surgery, 8.6% in family practice, 54.1% in internal medicine, and 36.2% in gastroenterology, with 40.0% having board certification in more than one specialty. In all instances, the most specialized designation superseded any general designation (e.g., a physician who is board certified in both internal medicine and gastroenterology would be classified as a gastroenterologist). Using board designation, we were able to classify 36,653 (83.2%) of the physicians in the sample into one of our 6 specialties. For those without board certification, we relied on training histories (the most specialized training received in a program of at least 1 year's duration) to classify 5,430 (12.3%) of the physicians. For the remaining 1,948 physicians, we relied on their self-designated specialty codes to classify specialty. Of these, 1,009 (2.3%) had agreement between the AMA Physician Masterfile and Medicare self-designated specialty codes, and for the remaining 939 physicians (2.1%), the more specialized of the self-designated codes was used. This exhaustive effort to correctly classify physicians was integral to our examination of practice patterns of generalists and specialists and consistent with the methods used by other investigators in this field.29 An examination of the relation, or concordance rates, between the specialty self-designation codes of Medicare and the AMA Physician Masterfile and the composite codes is presented in Table 1). The composite codes for specialty designation were used in the remainder of our analyses.
Table 1.
Concordance Between Our Composite Coding of Physician Specialty and Coding in the American Medical Association (AMA) Physician Masterfile and the Medicare Database†
| CompositeSpecialty Code* | FamilyPractice, % (n) | GeneralPractice, % (n) | General InternalMedicine, % (n) | Gastroenterology,% (n) | GeneralSurgery, % (n) | ColorectalSurgery, % (n) |
|---|---|---|---|---|---|---|
| Concordance with AMAPhysician MasterfileDesignation | 95 (4,367) | 79 (612) | 91 (7,942) | 95 (19,365) | 98 (8,325) | 88 (2,070) |
| Concordance withMedicare Self-Designated Specialty | 92 (4,437) | 58 (913) | 71 (11,235) | 99 (15,463) | 93 (9,197) | 97 (1,387) |
Concordance is defined as the correlation between specialty self-designation codes of Medicare and the AMA Physician Masterfile. There were 1,350 physicians from the AMA Masterfile who were categorized as either “unspecified” or “other.” Similarly, there were 1,399 physicians whose Medicare self-designated code was “multispecialty clinic or group practice,” which did not correspond to the 6 specialties of interest. After applying our specialty designation methodology, we were able to classify all but 74 (0.2%) of the physicians. Those 74 physicians and the procedures they provided were omitted from the analysis.
Procedure Characteristics
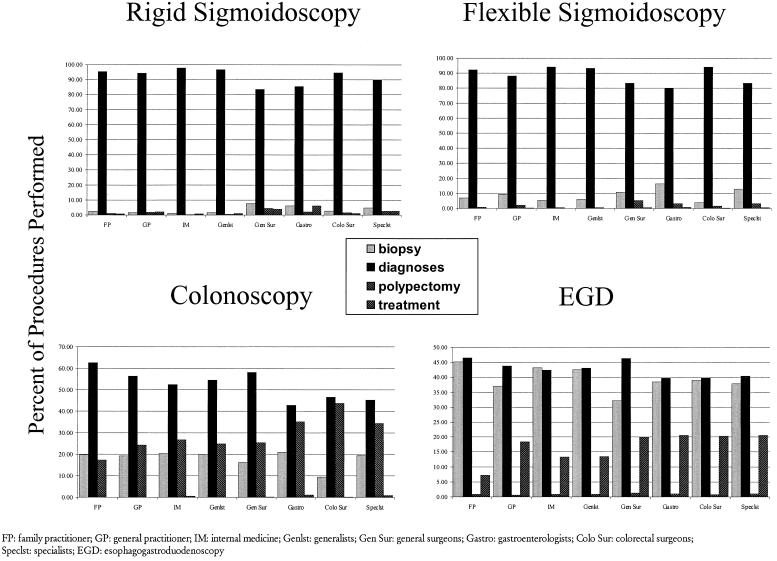
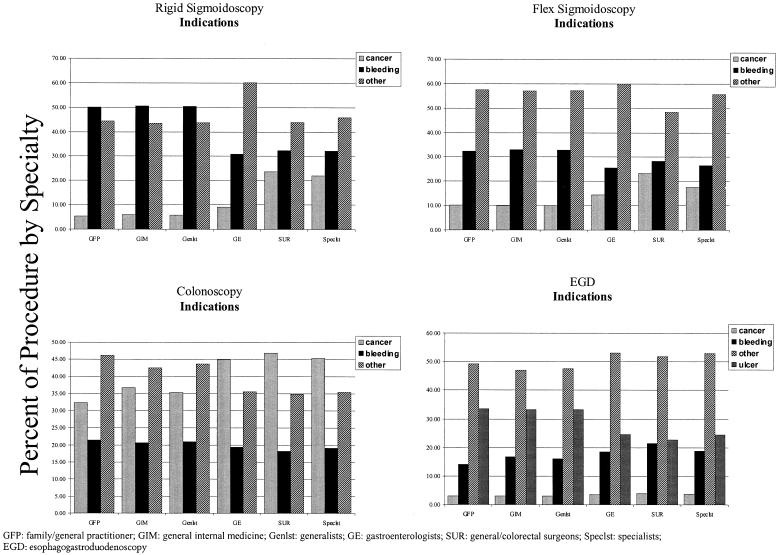
Our sample population had 9,396 rigid sigmoidoscopies (35.2% by generalists), 38,261 flexible sigmoidoscopies (42.7% by generalists), 57,221 colonoscopies (7.7% by generalists), and 62,469 EGDs (8.7% by generalists) (Table 2). For all 4 procedures, while specialists were much more likely than generalists to have performed a procedure for biopsy, polypectomy, or treatment rather than for diagnostic purposes alone (odds ratio [OR]± 4.2; 95% confidence interval [95% CI] 4.0 to 4.4) (Fig. 1). The indications for the procedures varied significantly between generalists and specialists, with specialists being more likely than generalists to perform the procedure to investigate cancer (Fig. 2). Specialists were more likely to have performed the procedures in the hospital or an ambulatory surgical center than in the office (OR 6.9; 95% CI, 6.7 to 7.1). Overall, specialists tended sicker or more complex patients as demonstrated by the more serious indications and higher complexity of the procedures performed (Figs. 1 and 2).
Table 2.
Gastrointestinal Endoscopies Performed by Various Specialties in 5% Medicare Sample*
| Procedure | Family Practice | General Practice | General Internal Medicine | Generalists | Gastroenterology | General Surgery | Colorectal Surgery | Specialists |
|---|---|---|---|---|---|---|---|---|
| Colonoscopy(n = 57,221) | 6551.1 | 7371.3 | 3,0195.3 | 4,4117.7 | 41,75873 | 7,43413 | 3,6186.3 | 52,81092.3 |
| EGD(n = 62,469) | 5200.8 | 7641.2 | 4,1286.6 | 5,4128.7 | 50,96281.6 | 5,9679.6 | 1280.2 | 57,05791.3 |
| Flexible sigmoidoscopy(n = 38,261) | 4,88612.8 | 8922.3 | 10,56627.6 | 16,34442.7 | 14,17737 | 3,3118.6 | 4,42911.6 | 21,91757.3 |
| Rigid sigmoidoscopy(n = 9,396) | 6967.4 | 3754 | 2,23623.8 | 3,30735.2 | 7558 | 2,00821.4 | 3,32635.4 | 6,08964.8 |
Top number in each cell represents the number of procedures performed. Bottom number represents the percentage of patients that had the procedure performed by that type of physician.
FIGURE 1.
Purpose of gastrointestinal endoscopies, by specialty.
FIGURE 2.
Indications for gastrointestinal endoscopies, by specialty.
Patient Characteristics
The age distribution of patients receiving gastrointestinal endoscopies did not differ between generalists and specialists (Table 3). However, the gender distribution of patients receiving colonoscopy or flexible sigmoidoscopy (but not EGD or rigid sigmoidoscopy) did differ between generalists and specialists.
Table 3.
Characteristics of Medicare Beneficiaries that Received Gastrointestinal Endoscopies*
| Colonoscopy | EGD | Flexible Sigmoidoscopy | Rigid Sigmoidoscopy | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PatientCharac-teristics | GFP | GIM | GE | SUR | OR(95% CI) | GFP | GIM | GE | SUR | OR(95% CI) | GFP | GIM | GE | SUR | OR(95% CI) | GFP | GIM | GE | SUR | OR(95% CI) |
| Mean age(± SD) | 74.8±6.8 | 74.8±6.7 | 74.9±6.5 | 74.8±6.5 | 76.6±7.7 | 76.2±7.3 | 76.2±7.3 | 76.7±7.5 | 73.7±6.3 | 73.7±6.2 | 74.9±6.7 | 74.8±6.6 | 74.4±6.8 | 74.2±6.3 | 75.9±7.0 | 74.6±6.7 | ||||
| % female | 58.2 | 56.9 | 56.2 | 53.3 | 1.07†(1.00, 1.14) | 61.2 | 59.5 | 59.4 | 57.2 | 1.04(0.97, 1.10) | 55.0 | 55.6 | 59.8 | 54.0 | 0.93†(0.89, 0.97) | 53.0 | 53.0 | 61.0 | 53.8 | 0.94(0.86, 1.03) |
| % white | 88.2 | 82.7 | 87.9 | 89.6 | 1.40†(1.28, 1.52) | 85.8 | 79.8 | 85.5 | 85.6 | 1.39†(1.28, 1.50) | 90.6 | 88.9 | 88.9 | 90.4 | 0.98(0.32, 1.05) | 91.9 | 89.2 | 89.4 | 90.7 | 1.06(0.92, 1.23) |
| % died withincalendaryear | 6.4 | 6.2 | 6.5 | 5.2 | 1.01(0.89, 1.16) | 15.4 | 14.3 | 16.4 | 18.5 | 1.18†(1.08, 1.29) | 2.8 | 2.5 | 7.4 | 4.6 | 2.28†(2.04, 2.55) | 4.0 | 2.4 | 4.5 | 4.8 | 1.61†(1.26, 2.06) |
| % admitted within calendar year | 42.0 | 42.1 | 43.7 | 40.8 | 1.05(0.98, 1.12) | 64.8 | 61.4 | 65.0 | 69.6 | 1.16†(1.09, 1.23) | 25.0 | 22.3 | 39.1 | 34.1 | 1.87†(1.78, 1.96) | 22.9 | 21.8 | 37.4 | 36.4 | 2.00†(1.81, 2.21) |
| % living in whole county health care provider shortage area | 10.0 | 8.2 | 4.7 | 7.9 | 0.60†(0.54, 0.68) | 15.4 | 9.8 | 5.5 | 14.0 | 0.56†(0.50–0.62) | 5.6 | 4.1 | 4.2 | 5.2 | 0.98(0.89–1.09) | 5.6 | 3.0 | 3.3 | 4.4 | 1.13(0.90, 1.42) |
| living in a county with any GE | 52.5 | 66.1 | 85.7 | 65.8 | 2.76†(2.58, 2.94) | 45.3 | 63.5 | 84.2 | 47.9 | 2.83†(2.65, 3.01) | 69.0 | 81.4 | 87.7 | 78.8 | 1.66†(1.57, 1.74) | 73.0 | 88.6 | 90.4 | 81.9 | 0.97(0.86, 1.09) |
| % in a high poverty county‡ | 4.6 | 5.3 | 2.8 | 4.0 | 0.62†(0.54, 0.72) | 8.2 | 6.2 | 3.4 | 7.2 | 0.58†(0.51, 0.66) | 2.4 | 1.8 | 2.5 | 2.8 | 1.26†(1.10, 1.45) | 2.5 | 4.0 | 2.7 | 1.8 | 0.54†(0.41, 0.71) |
| % in a countywith highHMOpenetration | 25.9 | 29.1 | 46.8 | 34.3 | 2.08†(1.94, 2.23) | 23.9 | 28.9 | 47.7 | 18.0 | 2.15†(2.00, 2.30) | 34.5 | 47.7 | 52.7 | 48.5 | 1.40†(1.34, 1.46) | 40.1 | 60.4 | 52.7 | 52.0 | 0.93(0.85, 1.02) |
| % in a countywith highproportion ofgeneralists§ | 11.6 | 5.2 | 2.4 | 4.1 | 0.36†(0.31, 0.41) | 12.2 | 4.6 | 2.6 | 6.5 | 0.45†(0.39, 0.51) | 5.8 | 1.8 | 1.9 | 2.5 | 0.63†(0.55, 0.72) | 6.3 | 1.6 | 1.3 | 2.4 | 0.72†(0.55, 0.95) |
| % in a county with high physician proportion‖ | 23.1 | 29.2 | 50.2 | 36.0 | 2.43†(2.26, 2.61) | 18.5 | 28.5 | 49.8 | 20.3 | 2.53†(2.36, 2.72) | 33.9 | 50.3 | 56.8 | 49.0 | 1.47†(1.41, 1.54) | 41.9 | 61.9 | 63.5 | 53.2 | 0.96(0.88, 1.05) |
| % having procedure in hospital or ASC | 76.0 | 81.9 | 92.8 | 93.2 | 3.28†(3.02, 3.57) | 88.5 | 86.8 | 94.4 | 95.6 | 2.53†(2.30, 2.79) | 23.0 | 15.2 | 41.6 | 25.6 | 2.47†(2.35, 2.59) | 15.6 | 6.4 | 21.7 | 17.4 | 2.06†(1.80, 2.37) |
| % in rural county¶ | 9.2 | 5.6 | 2.4 | 5.2 | 0.42†(0.37, 0.48) | 9.8 | 4.7 | 2.6 | 7.9 | 0.53†(0.46, 0.60) | 5.7 | 2.7 | 2.2 | 3.0 | 0.65†(0.58, 0.74) | 4.9 | 1.7 | 1.8 | 2.4 | 0.87(0.66, 1.15) |
Beneficiaries younger than 65 years, those enrolled in HMOs, and those living outside the 50 states and the District of Columbia were excluded from our sample. EGD indicates esophagogastroduodenoscopy; GFP, general/family practitioners; GIM, general internal medicine; GE, gastroenterologists; SUR, general and colorectal surgeons; OR, odds ratio; CI, confidence interval; ASC, ambulatory surgery center. All odds ratios were age- and gender-adjusted and were based on the differences between generalists and specialists, where generalists included general family practitioners and general internal medicine physicians and specialists included gastroenterologists, general surgeons, and colorectal surgeons.
P < .05 for the comparison between generalists and specialists.
“High poverty” is defined as greater than 1 SD above the mean percentage of poverty.
“High proportion of generalists” is defined as greater than 1 SD above the mean for presence of generalists.
“High physician proportion” is defined as greater than 1 SD above the physician-to-population mean.
“Rural” is defined by Medicare Area Resource File as a nonmetropolitan statistical area.
The patients receiving sigmoidoscopy and EGD from specialists had poorer overall health status than those receiving the procedures from generalists, as noted by their greater likelihood to die or be hospitalized within the calendar year. For all 4 procedures, patients receiving these services from generalists were more likely to face difficulty in accessing specialist care as noted by their residence in a federally designated Health Professions Shortage Area, absence of gastroenterologists in their county, a low physician-to-population ratio, and a high proportion of generalists among the physician provider pool. Across all 4 procedures, generalists were more likely to provide these services to patients residing in rural areas and in areas other than the Northeast.
DISCUSSION
The role that specialists play in the provision of generalist services has been well documented.30,31 We have found that the converse, the provision of speciality services by generalists, must also be considered in the evaluation of the physician workforce structure and the quality of care it produces. In our analyses, 41% of sigmoidoscopies and 8% of more complex gastrointestinal endoscopic procedures were performed by generalists. The latter figure is below earlier assessments,5 which relied on a single indicator of physician specialty (the self-designated code in the Medicare files). Our rigorous documentation of physician specialty from multiple sources makes it much more likely that those 8% of complex endoscopies were indeed performed by generalist physicians who did not differ significantly from their generalist colleagues in terms of training or board certification.
We were able to document important differences between generalists and specialists in the patients who received these services. Those differences were particularly marked in comparisons between general/family practitioners and gastroenterologists. Although individual differences were often subtle, the aggregate effect leads to the conclusion that specialists were more likely to see patients who were less healthy (as noted by inpatient status at the time of the procedure and likelihood of dying within the calendar year), had more serious indications for the procedure (e.g., cancer as opposed to screening), and received more complex interventions (e.g., endoscopy with a polypectomy or other therapeutic intervention).
The proportion of complex procedures performed by generalists is likely to increase as maturing technology empowers generalists to integrate an expanding array of procedures into their routine practice.32 The specialists' willingness to teach generalists gastrointestinal procedures and techniques has been beneficial in terms of access, especially in rural areas, as 40% of U.S. health care service areas are without a gastroenterologist.5 Even in areas with many specialists, however, some patients receive complex endoscopic services from generalists.
The important contribution to access by the provision of some of these services by generalists demands careful attention to any disparity in outcome by provider group. Improved access does not imply improved quality because receiving a substandard examination may, in fact, be less desirable than not receiving any examination at all. Our analyses suggest that examinations of the gastrointestinal endoscopy outcomes produced by various provider types should take into account existing differences between generalists and specialists in patient characteristics and clinical indications for these procedures.
Limitations of our study are those of the databases we employed. Our linkage of procedures with the conditions for which they were performed provided an increased level of accuracy in the data. Systematic “overcoding” of procedures by generalists versus specialists introduces another potential bias. Oversight of procedural coding by the Medicare program, however, potentially mitigates biases that may exist. Because routine screening for colorectal cancer with flexible sigmoidoscopy was not covered by Medicare during 1993 (but is currently available through the Medicare reform implemented on January 1, 1998), it is likely that the number of screening flexible sigmoidoscopies performed was underestimated.33 Nevertheless, the data presented are representative of flexible sigmoidoscopy practices of the various specialties for all indications other than routine screening. Because of incomplete claims reporting under Medicare managed care in 1993, we were unable to examine the effect of managed care on the provision of these procedures by generalists and specialists.
In conclusion, generalist physicians make a substantial contribution to patient access to gastrointestinal endoscopy, including more complex procedures such as colonoscopy and EGD. Although numerous benefits may be realized by expanding the procedural domain of generalists, our analyses indicate that performance of gastrointestinal endoscopy by generalists is currently focused on particular populations and procedures of relatively low complexity compared with procedures provided by specialists. Future work will need to critically examine the outcomes of gastrointestinal endoscopies performed by generalists and specialists accounting for these important differences.
Acknowledgments
The authors thank Dr. Henry Krakauer for statistical advice and the anonymous reviewers for their review of earlier drafts of this manuscript. The authors also acknowledge the advice and support of their colleague, Dr. Itzhak Jacoby, who served as a key counselor on this work until his tragic death in November 1999.
Dr. Meyer's work is funded by a Generalist Physician Faculty Scholar Award from the Robert Wood Johnson Foundation.
REFERENCES
- 1.Wigton RS, Blank LL, Nicolas JA, Tape TG. Procedural skills training in internal medicine residencies. Ann Intern Med. 1989;111:932–8. doi: 10.7326/0003-4819-111-11-932. [DOI] [PubMed] [Google Scholar]
- 2.Rodney WM. Flexible sigmoidoscopy and the despecialization of gastrointestinal endoscopy. Cancer (suppl) 1992;70:1266–71. doi: 10.1002/1097-0142(19920901)70:3+<1266::aid-cncr2820701512>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 3.Rodney WM. Flexible sigmoidoscopy and the despecialization of gastrointestinal endoscopy. Cancer. 1992;70:1266–71. doi: 10.1002/1097-0142(19920901)70:3+<1266::aid-cncr2820701512>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 4.Hocutt JE, Rodney WM, Zurad EG, Tucker RS, Norris T. Esophagogastroduodenoscopy for the family physician. Am Fam Phys. 1994;49:109–16. [PubMed] [Google Scholar]
- 5.Meyer GS, Jacoby I, Krakauer H, Powell DW, Aurand J, McCardle P. Gastroenterology workforce modeling. JAMA. 1996;276:689–94. [PubMed] [Google Scholar]
- 6.Wigton RS, Blank LL, Nicolas JA, Tape TG. Procedural skills training in internal medicine residencies. Ann Intern Med. 1989;111:1023–34. doi: 10.7326/0003-4819-111-11-932. [DOI] [PubMed] [Google Scholar]
- 7.Phillips WR. Diagnostic and screening procedures in family practice. Arch Fam Pract. 1993;2:1051–7. doi: 10.1001/archfami.2.10.1051. [DOI] [PubMed] [Google Scholar]
- 8.Wanebo HJ, Fang WL, Mills S, Zfass AM. Colorectal cancer: a blueprint for disease control through screening by primary care physicians. Arch Surg. 1986;121:1347–52. doi: 10.1001/archsurg.121.11.1347. [DOI] [PubMed] [Google Scholar]
- 9.Cremins JE. Esophagogastrocuodenoscopy in a small army community hospital. Mil Med. 1993;158:90–1. [PubMed] [Google Scholar]
- 10.Woodliff DM. The role of upper gastrointestinal endoscopy in primary care. J Fam Pract. 1979;8:715–9. [PubMed] [Google Scholar]
- 11.Pope JB, Mayeaus EJ, Harper MB. Effectiveness and safety of esophagogastroduodenoscopy in family practice: experience at a university medical center. Fam Med. 1995;27:506–11. [PubMed] [Google Scholar]
- 12.Rodney WM, Weber JR, Swedbert JA, et al. Esophagogastruduodenoscopy by family physician, phase II: a national multisite study of 2500 procedures. Fam Pract Res J. 1993;13:121–31. [PubMed] [Google Scholar]
- 13.Hocutt JE, Rodney WM, Zurad EG, Tucker RS, Norris T. Esophagogastroduodenoscopy for the family physician. Am Fam Phys. 1994;49:109–16. [PubMed] [Google Scholar]
- 14.Rodney WM, Dabov G, Cronin C. Evolving colonoscopy skills in a rural family practice: the first 293 cases. Fam Pract Res J. 1993;13:43–52. [PubMed] [Google Scholar]
- 15.Hopper W, Kyker KA, Rodney WM. Colonoscopy by a family physician: a 9-year experience of 1048 procedures. J Fam Pract. 1996;43:561–6. [PubMed] [Google Scholar]
- 16.Pierzhajlo RP, Ackerman RJ, Vogel RL. Colonoscopy performed by a family physician. J Fam Pract. 1997;44:473–80. [PubMed] [Google Scholar]
- 17.Harper MB, Pope JB, Mayeaus EJ, Davis TJ, Myers A, Lirette A. Colonoscopy experience at a family practice residency: a comparison to gastroenterology and general surgery services. Fam Med. 1997;29:575–9. [PubMed] [Google Scholar]
- 18.Rex DK. Colonoscopy by family practitioners. Gastrointest Endosc. 1994;40:383–4. doi: 10.1016/s0016-5107(94)70084-2. [DOI] [PubMed] [Google Scholar]
- 19.Zuber TJ, Pfenninger JL. Interspecialty wars over endoscopy. J Fam Pract. 1993;37:21–2. [PubMed] [Google Scholar]
- 20.Parente ST, Weiner JP, Garnick DW, et al. Developing a quality improvement database using health insurance data: a guided tour with application to Medicare's national claims history file. Am J Med Qual. 1995;10:162–76. doi: 10.1177/0885713X9501000402. [DOI] [PubMed] [Google Scholar]
- 21.Physicians' Current Procedural Terminology (CPT) 4th ed. Chicago, Ill: American Medical Association; 1992. [Google Scholar]
- 22. International Classification of Diseases, 9th Revision, Clinical Modification. Salt Lake City, Utah: Medicode Publications; 1995.
- 23. Health Care Financing Administration Privacy Act of 1974; systems of records. Fed Reg. 1990:55:18179–81. [PubMed]
- 24. Elixhauser A. Clinical Classifications for Health Policy Research, Version 2: Software and User's Guide. Healthcare Cost and Utilization Project (HCUP-3) Research Note 2. Rockville, Md: Agency for Health Care Policy and Research; 1996. AHCPR publication 96-0046.
- 25. User documentation for the Area Resource File. Rockville, Md. Office of Research and Planning Bureau of Heath Professions, Health Resources and Services Administration; February 1993. Rockville, Md.
- 26.Stambler HV. The Area Resource File—a brief look. Public Health Rep. 1988;103:184–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Roback C, Randolph L, Seidman G. Physician Characteristics and Distribution in the United States. Chicago, Ill: American Medical Association; 1992. [Google Scholar]
- 28. Stata Reference Manual, Version 5.0. College Station, Tex: Stata Corp; 1996.
- 29.Rosenblatt RA, Hart G, Baldwin L, Chan L, Schneeweiss R. The generalist role of specialty physicians: is there a hidden system of primary care? JAMA. 1998;279:1364–70. doi: 10.1001/jama.279.17.1364. [DOI] [PubMed] [Google Scholar]
- 30.Aiken LH, Lewis CD, Craig J, Mendenhall RC, Blendon RJ, Rogers DE. The contribution of specialists to the delivery of primary care. N Engl J Med. 1979;300:1363–70. doi: 10.1056/NEJM197906143002404. [DOI] [PubMed] [Google Scholar]
- 31.Spiegel JS, Rubenstein LV, Scott B, Brook RH. Who is the primary physician? N Engl J Med. 1983;308:1208–12. doi: 10.1056/NEJM198305193082007. [DOI] [PubMed] [Google Scholar]
- 32.Rodney WM. Procedural skills in flexible sigmoidoscopy and colonoscopy for the family physician. Prim Care Clin. 1988;15:79–91. [PubMed] [Google Scholar]
- 33.Ackermann RJ. Performance of gastrointestinal tract endoscopy by primary care physicians. Arch Fam Med. 1997;6:52–8. doi: 10.1001/archfami.6.1.52. [DOI] [PubMed] [Google Scholar]