Abstract
OBJECTIVE
To determine the prevalence, sociodemographic determinants, and depression correlates of intimate partner abuse among an ethnically diverse population of women patients.
DESIGN
Cross-sectional telephone survey in English and Spanish of a random sample of women patients aged 18 to 46 years.
SETTING
Three public hospital primary care clinics (general internal medicine, family medicine, and obstetrics/gynecology) in San Francisco, Calif.
PARTICIPANTS
We interviewed 734 (74%) of the 992 eligible participants. Thirty-one percent were non-Latina white, 31% African American, and 36% Latina.
MEASUREMENTS AND MAIN RESULTS
Using questions adapted from the Abuse Assessment Screen, we determined recent and lifetime history of physical, sexual, and psychological abuse. Overall, 15% reported recent abuse by an intimate partner (in the preceding 12 months); lifetime prevalence was 51%. Recent abuse was more common among women aged 18 to 29 years (adjusted odds ratio [OR] 2.1; 95% confidence interval [CI], 1.2 to 3.7), non-Latinas (adjusted OR, 1.7; 95% CI, 1.0 to 2.9), and unmarried women (adjusted OR, 1.65; 95% CI, 1.0 to 2.7). The prevalence of abuse did not differ by education, employment, or medical insurance status of the women. Compared with women with no history of abuse, a greater proportion of recently abused women reported symptoms of depression (adjusted OR, 3.5; 95% CI, 2.2 to 5.5).
CONCLUSIONS
Because a substantial proportion of women patients in primary care settings are abused, screening for partner abuse and depression is indicated. In contrast to other studies, lower socioeconomic status was not associated with partner abuse history.
Keywords: domestic violence, spouse abuse, prevalence, risk factors, socioeconomic status, ethnicity, depression
Every year in the United States, physical violence occurs in an estimated 4 to 6 million intimate relationships.1,2 Although some studies have found that the prevalence of intimate partner violence varies among different race/ethnic and socioeconomic groups, these relationships have yet to be fully established. Five national surveys conducted between 1975 and 1996 consistently found higher rates of violence among African-American2–5 and Latino2,6,7 couples compared with white couples. In addition, all of these national surveys found that partner violence was associated with lower socioeconomic status (SES).2–7
Regional population-based research has produced conflicting results with regard to these sociodemographic associations. While differing definitions of abuse limit study comparability, some research demonstrated higher rates of partner violence among nonwhite couples,8 whereas others showed no significant associations.9,10 In addition, the association between partner violence and low SES has been reproduced in community-based studies.8,11 However, attempts to simultaneously control for race/ethnicity and SES have produced conflicting results. Although some researchers have reported that differing rates of partner violence among racial/ethnic minority groups persisted when SES was controlled,3,4,8 others found that differences in SES completely explain the ethnic disparities.6,9
Clinic-based prevalence studies in primary care settings also have produced conflicting results regarding the associations of race/ethnicity and SES with intimate partner violence. Most researchers found that factors reflecting lower SES were associated with partner violence.12–14 However, studies that examined rates of intimate partner violence among different racial/ethnic groups, found either no difference14 or higher rates reported by white patients compared with nonwhite patients.13,15
Although it is generally believed that partner abuse often leads to serious psychological problems for women victims,16,17 few clinical studies have demonstrated a definitive relationship. In the absence of comparison groups, researchers have found that a large proportion of women with depression and suicidal behavior have been abused.18,19 A large well-controlled cross-sectional patient survey in Baltimore demonstrated significant associations between domestic violence and psychiatric symptoms, including depression, anxiety, and somatization.14,20 In this paper, we examine the prevalence, demographic determinants, and depression symptom correlates of intimate partner abuse in a young, ethnically diverse, low-income group of women clinic patients.
METHODS
Study Population and Subject Recruitment
The sample consisted of female patients who were seen at three outpatient clinics associated with the San Francisco Community Health Network in California. These clinics, which included general internal medicine, family medicine, and obstetrics/gynecology, were chosen because they represent diverse sources of primary care for adult women patients in the public clinic system. Together, these clinics serve approximately 100,000 women aged 18 to 45 years annually.
A sample of 1,390 patients was randomly generated using a computerized medical care utilization database for calendar year 1997. Criteria used to select the sample included female gender; race/ethnicity of either African American, white, or Latina; aged 18 to 45 years; and receipt of care in one of the three primary care clinics in the previous 6 months. Female gender was among the selection criteria because compared with men, women have a higher prevalence of partner abuse and are more likely to sustain physical injuries and incur psychological consequences of intimate partner abuse.21 Asian women were not sampled because of the anticipated difficulties in accommodating the multiple languages spoken.
Data Collection
A telephone survey designed to identify the prevalence of intimate partner abuse was administered to a sample of adult women patients. During the data collection period of October 1997 through March 1998, an introductory letter explaining the nature of the study was sent to all 1,390 potential participants prior to telephone contact. To maximize participation, telephone calls were made at different times of the day and on weekends. Once the patient was contacted, trained female interviewers obtained verbal consent, confirmed eligibility, and established privacy and safety. Women were excluded if they did not have a verifiable telephone number; did not speak English or Spanish; were incapable of completing the survey due to acute illness or disability; or did not meet the above selection criteria. Interviews were conducted in English or Spanish. The study protocol was approved by the Committee for Human Research at the University of California, San Francisco.
Measures
The survey instrument consisted of 3 modules: (1) demographic, socioeconomic, and family characteristics; (2) general health, depression, and clinic utilization; and (3) partner abuse experiences. All respondents were asked to categorize themselves as white, African American, Latina, or “other.” Socioeconomic status was assessed by way of educational attainment, current employment, and medical insurance status. Because the specialty clinic recorded in the utilization database may not have represented the women's usual source of care, respondents were asked to identify the clinic in which they receive primary medical care. Indicators of depression were identified by asking whether the respondent “had been bothered by feeling down, depressed or hopeless” (depressed mood) or “had little interest or pleasure in doing things” (anhedonia) during the past 4 weeks.22 To estimate the level of acculturation among respondents who identified as Latina, we included a validated 4-question scale on language use.23
The questions about partner abuse were adapted from the Abuse Assessment Screen, which has been validated in multiethnic populations through comparisons with the Index of Spouse Abuse and the Conflicts Tactics Scale.24,25 To define physical abuse, we asked, “Have you ever been hit, slapped, kicked, or otherwise physically hurt by your partner or ex-partner?” To define sexual abuse, we asked, “Has your partner or ex-partner ever forced you to have sexual activities?” To assess psychological aspects of abuse, we asked, “Has your partner or ex-partner ever threatened you or made you feel afraid or unsafe?” For each positive response, women were asked whether the abuse occurred in the past 12 months (recent abuse1,2) or in the more distant past (past abuse).
The questionnaire was prepared in English and translated to Spanish incorporating back-translation.26 The questionnaire was pilot tested in both English and Spanish with 75 women public clinic patients; 25 from each of the 3 target ethnic groups. Based on the pilot interviews, the instrument was modified to improve clarity and flow.
Data Analyses
To assess the relationships between ethnicity, SES, and partner abuse, the data were analyzed using SPSS statistical software (Version 8.0 for Windows, SPSS, Inc., Chicago, Ill). For comparison of means, analysis of variance was used to determine statistical significance. For cross tabulations, statistical significance was determined using Yate's corrected χ2or Pearson χ2tests. Statistical significance was defined as P < .05. The principal outcome variable was partner abuse, defined as physical abuse, sexual abuse, or threats/fear, stratified by recent (within the past 12 months), past only (more than 12 months ago), and never. Psychological aspects of abuse were included to capture those at risk for violence and adverse health outcomes. Predictor variables included age, ethnicity, marital status, education, employment, insurance status, and birthplace. We used logistic regression analysis to estimate adjusted odds ratios (OR) and 95% confidence intervals (95% CI) for the factors associated with recent intimate partner abuse. Similar methods were used to assess the association between abuse history and reported depression symptoms.
RESULTS
Study Participants
Of the 1,390 patients selected from the database, we were able to contact 1,075 women; 315 (23%) did not have a verifiable telephone number. Of the 1,075 contacted, 992 were eligible and 83 were excluded because they did not speak English or Spanish, were incapable of completing the survey, or did not meet the original selection criteria. The overall participation rate was 74% (734/992) of the eligible participants.
Overall, 20% of respondents reported that they received primary medical care at the general internal medicine clinic, 29% at the family medicine clinic, 28% at the obstetrics/gynecology clinic, and 23% at other local clinics. The racial/ethnic composition of participants was 31% non-Latina white, 31% African American, and 36% Latina. Demographic and socioeconomic factors varied significantly by race/ethnicity (Table 1). The age of participants ranged from 18 to 46 years, with a mean of 33.5. Over one third (35%) of participants were born outside the United States; 83% of Latina participants were immigrants. Of the 256 immigrants, 32% were from El Salvador, 21% from Mexico, 14% from Nicaragua, 12% from Guatemala, and 21% from other countries. Overall, 27% of participants chose to take the survey in Spanish.
Table 1.
Characteristics of Study Participants
| Racial/Ethnic Identity | ||||
|---|---|---|---|---|
| Characteristic | White (n = 224) | African American (n = 229) | Latina (n = 265) | Total*(N = 734) |
| Mean age, y (SD)† | 34.5 (7.2) | 32.7 (7.9) | 33.3 (7.4) | 33.5 (7.5) |
| U.S.-born, %‡ | 88 | 98 | 17 | 65 |
| Marital status, %‡ | ||||
| Married/cohabitant | 34 | 23 | 61 | 41 |
| Separated/divorced | 15 | 10 | 12 | 12 |
| Never married | 52 | 67 | 28 | 47 |
| Children at home, %‡ | 25 | 65 | 80 | 58 |
| Mean years education (SD)§ | 14.0 (2.7) | 12.1 (1.7) | 9.6 (4.2) | 11.8 (3.6) |
| Employed, %‖ | 51 | 37 | 53 | 47 |
| Medically insured, %‖ | 46 | 57 | 41 | 48 |
| Reported fair or poor health, %‡ | 23 | 34 | 45 | 35 |
| Reported depression symptoms, % | ||||
| Depressed mood | 58 | 47 | 53 | 53 |
| Anhedonia | 42 | 43 | 38 | 41 |
| Both symptoms | 36 | 34 | 30 | 33 |
Total includes white, African American, Latina, and 16 “other.”
P < .05 significance level for 3 race/ethnic groups based on analysis of variance (ANOVA) test.
P < .001 significance level for 3 race/ethnic groups based on Pearson χ2 test.
P < .001 significance level for 3 race/ethnic groups based on ANOVA test.
P < .01 significance level for 3 race/ethnic groups based on Pearson χ2 test.
Less than half of participants were married or living with their partner (Table 1). Latinas were most likely to be married or cohabitating. Of never married women, 40% reported that they had a current partner who did not live with them. Over half of the respondents reported having children living in their homes. Educational attainment ranged from none to postgraduate; the mean was 11.8 years of education. Almost half were employed, and over half had no medical insurance. Self-reported “fair or poor” general health and symptoms of depression were common among study participants.
Prevalence of Intimate Partner Abuse
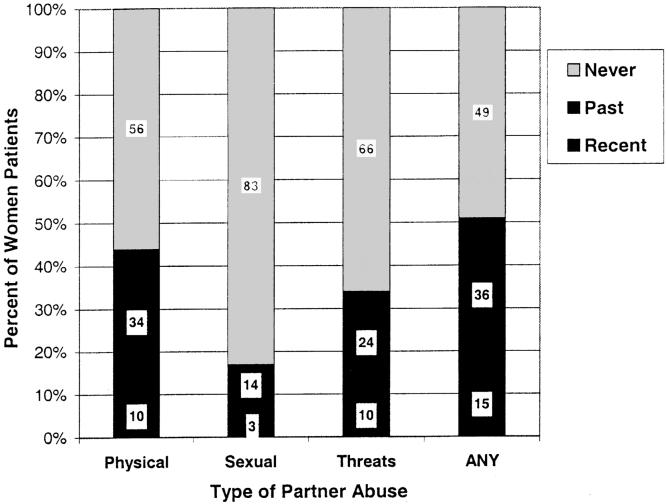
The prevalence of recent and lifetime intimate partner abuse is shown in Figure 1. Overall, 10% of women reported being physically abused in the past 12 months, 3% reported sexual abuse, 10% reported threats by a partner or expartner, and 15% reported at least one of these forms of abuse. Lifetime prevalence of physical abuse was 45%; lifetime prevalence of sexual abuse was 17%; and lifetime prevalence of threats was 34%.Over half (51%) reported at least one form of abuse had occurred in their lifetime. Of the 107 women reporting some type of abuse in the past 12 months, 31% reported physical or sexual abuse, but no threats or fear; 21% reported threats and fear in the absence of physical or sexual abuse; and 48% reported both physical/sexual abuse and threats.
FIGURE 1.
Intimate partner abuse in 734 women seen in public clinics, San Francisco, 1997. Physical abuse was defined as having been hit, slapped, kicked, or otherwise physically hurt by a partner or ex-partner. Sexual abuse was defined as having been forced to have sexual activities by a partner or ex-partner. Threats included when a partner or ex-partner made the patient feel afraid or unsafe. Recent was defined as the previous 12 months.
Sociodemographic Determinants of Intimate Partner Abuse
The prevalence of recent partner abuse was similar among patients who reported different sources of primary care: 14% at the general internal medicine clinic, 13% at the family medicine clinic, 15% at the obstetrics/gynecology clinic, and 16% at other clinics (P = .722). As shown in Table 2), age, ethnicity, and marital status were significantly associated with recent partner abuse. The prevalence of recent abuse was highest among women aged 18 to 29 years (P = .013). There was no difference in the prevalence between white and African-American women; however, significantly fewer Latinas reported recent abuse (P = .009). The prevalence of abuse was higher among U.S.-born women (16% of U.S.-born women and 11% of immigrants; P = .086) and more acculturated Latinas (15% of more acculturated and 9% of less acculturated Latinas; P = .202); however, these differences were not statistically significant.
Table 2.
Sociodemographic Determinants of Recent Intimate Partner Abuse (IPA), N = 734
| Factor | n | Prevalence of Recent IPA, % | Crude Odds Ratio (95% Confidence Interval) | Model 1* Adjusted Odds Ratio (95% Confidence Interval) | Model 2† Adjusted Odds Ratio (95% Confidence Interval) |
|---|---|---|---|---|---|
| Age, y | |||||
| 18–29 | 230 | 20 | 2.08 (1.19 to 3.64) | 2.14 (1.20 to 3.79) | 2.11 (1.18 to 3.77) |
| 30–39 | 303 | 14 | 1.34 (0.77 to 2.35) | 1.49 (0.84 to 2.64) | 1.46 (0.82 to 2.62) |
| 40–46 | 201 | 10 | 1.0 | 1.0 | 1.0 |
| Ethnicity | |||||
| White | 224 | 18 | 1.92 (1.13 to 3.24) | 1.73 (1.00 to 2.98) | 1.90 (1.03 to 3.51) |
| African American | 229 | 18 | 1.87 (1.10 to 3.15) | 1.56 (0.90 to 2.72) | 1.62 (0.90 to 2.94) |
| Latina | 265 | 10 | 1.0 | 1.0 | 1.0 |
| Marital status | |||||
| Married | 294 | 10 | 1.0 | 1.0 | 1.0 |
| Unmarried | 429 | 18 | 1.95 (1.18 to 3.23) | 1.59 (0.98 to 2.57) | 1.66 (1.01 to 2.72) |
| Education | |||||
| <12 years | 231 | 13 | 1.0 | — | 1.0 |
| 12 years | 246 | 15 | 1.15 (0.68 to 1.94) | — | 0.95 (0.54 to 1.67) |
| >12 years | 254 | 15 | 1.22 (0.73 to 2.03) | — | 0.99 (0.54 to 1.79) |
| Employed | 336 | 13 | 1.0 | — | 1.0 |
| Unemployed | 385 | 16 | 1.19 (0.79 to 1.81) | — | 1.18 (0.76 to 1.83) |
| Insured | 349 | 13 | 1.0 | — | 1.0 |
| Uninsured | 384 | 16 | 1.24 (0.82 to 1.88) | — | 1.38 (0.89 to 2.14) |
Model 1 adjusted for age, ethnicity, and marital status.
Model 2 adjusted for age, ethnicity, marital status, education, employment, and insurance.
Compared with married and cohabitating women, a significantly higher proportion of unmarried women reported recent abuse (P = .007). Because the prevalence of abuse did not vary significantly between categories of unmarried women (18% of never married and 15% of separated or divorced women; P = .584), these categories were combined. The prevalence of recent abuse did not vary significantly by education, employment, or medical insurance.
Based on logistic regression analysis controlling for the demographic factors that were significantly associated with recent abuse on bivariate analysis, women who were younger, non-Latina ethnicity, and unmarried were found to have a higher likelihood of recent partner abuse (Table 2), model 1). Although education and employment were colinear (P = .002), they were inversely correlated with the outcome variable. Insurance status was not significantly associated with education (P = .158) and employment (P = .191). When all three SES factors were included in the logistic regression model (Table 2), model 2), age, ethnicity, and marital status remained significant predictors of recent abuse. Comparable regression models with SES factors added individually or in combination produced similar results. Analogous analytic approaches using recent physical or sexual abuse (i.e., not including threats or fear) as the outcome variable produced almost identical results (data not shown).
Association of Abuse with Depression Symptoms
Compared with women with no history of partner abuse, reported depression symptoms were significantly higher among women abused in the past and recently abused women (Table 3). On bivariate analysis, the association was linear for all categories of depression symptoms (P < .001). Reported depression symptoms were significantly higher among older women and unmarried women; however, symptoms did not vary significantly by ethnicity, education level, employment, medical insurance, or immigration status. After adjusting for age and marital status using logistic regression, the strength of the associations increased (Table 3). Notably, among recently abused women, reported depression symptoms did not vary by the different types of partner abuse (data not shown).
Table 3.
Differences in Reported Depression Symptoms Among Women with Different Histories of Intimate Partner Abuse
| Self-reported Symptoms of Depression | ||||||
|---|---|---|---|---|---|---|
| Depressed Mood | Anhedonia | Both Symptoms | ||||
| Partner Abuse History | %* | Adjusted Odds Ratio†(95% Confidence Interval) | %* | Adjusted Odds Ratio†(95% Confidence Interval) | %* | Adjusted Odds Ratio†(95% Confidence Interval) |
| Never abused | 42 | 1.0 | 30 | 1.0 | 22 | 1.0 |
| Abused in past | 59 | 1.82 (1.30 to 2.54) | 47 | 1.75 (1.24 to 2.49) | 40 | 2.10 (1.46 to 3.01) |
| Recent abuse | 73 | 4.12 (2.51 to 6.76) | 60 | 3.33 (2.08 to 5.33) | 51 | 3.47 (2.18 to 5.52) |
Crude proportion reporting symptom, difference between categories of abuse are significant at P < .001 based on Pearson χ2 test.
Logistic regression adjustment for age and marital status.
Self-reported general health and clinic utilization were not significantly associated with a history of partner abuse; however, approximately one third (34%) of ever abused women reported seeking care for abuse-related problems.
DISCUSSION
In this sample of ethnically diverse, low-income women patients, the prevalence of physical abuse in the past 12 months was 10%. This estimate is comparable to those from national surveys.1,2,7 By expanding the definition of abuse to include sexual abuse, threats of violence, and fear, we found that the 12-month prevalence of intimate partner abuse was 15%. This prevalence of partner abuse was similar among primary care women patients regardless of the specialty clinic attended.
We did not expect to find a significant discrepancy between reported physical/sexual abuse and reported fear. However, among women reporting abuse in the past 12 months, 39% of physically/sexually abused women did not report experiencing threats or fear. The reasons for this discrepancy are unclear. Perhaps many women experiencing violence were in denial about the seriousness and risk. Alternatively, the violence they experienced may have been minor, occurred under unique circumstances, or had discontinued by the time they were interviewed. Of additional note, 31% of women who reported threats and fear in the past 12 months did not report concurrent physical or sexual abuse. It is unclear whether these women are at higher risk for future violence or adverse mental health consequences. These findings underscore the importance in both research and clinical practice to include measures of psychological abuse, perceptions of seriousness and risk, and the context of abusive or violent behavior.
Our finding that there was no difference in the prevalence of partner abuse between African American and white women is inconsistent with prior prevalence studies.2–5,8 By sampling from a group of public clinic patients, the socioeconomic variability within our sample was reduced. Our findings may indicate that African American-white differences found in other study populations were confounded by SES. Alternatively, instruments designed to assess partner abuse may vary in their sensitivity and specificity in measuring abuse among different racial/ethnic groups.
In our study population, ethnicity was a significant predictor of partner abuse and was independent of SES factors. Compared with white and African-American women, a smaller proportion of Latinas reported recent partner abuse. Although consistent with one national survey,4 several studies have found that the 12-month prevalence of partner violence among Latinas was higher than among whites.2,6,7 One reason for this discrepancy may be that by providing interviews in Spanish, we included a greater proportion of less acculturated immigrant women. Although the differences did not reach statistical significance, our results indicated that prevalence of recent abuse was lower for less acculturated Latinas compared with more acculturated Latinas. Similar results were obtained in a study that found the prevalence of partner violence was over 50% higher for U.S.-born Latinos compared to immigrant Latinos.10 These ethnic differences may be influenced by cultural beliefs and norms regarding violence, gender, and the family. Alternately, our measures may be less sensitive in the less-acculturated group because of underreporting or misinterpretations.
In contrast to prior studies,1,2,4,5,11,12,14 we found no association between recent partner abuse and SES measured as education, employment, and medical insurance status. One explanation for discrepant findings between studies may be the use of inexact and inconsistent measures of SES. Standard measures generally include household income, education, and employment; however, some researchers have included variables such as medical insurance status, the receipt of welfare benefits, and the partner's education and employment.2,11,14 Given the distribution of responses for the SES variables within our sample, we are confident that these factors have only a minimal effect on reported partner abuse history. However, by sampling from public clinic patients, we may have selected for homogeneity in unmeasured SES factors.
In this patient population, younger age and unmarried status were found to be independently predictive of recent partner abuse. The higher prevalence of partner violence among younger women has been well established in national surveys.1,4,5,7 Our finding that unmarried women are at higher risk of abuse is consistent with other clinic-based patient surveys.13,14 In addition, regional community-based studies have found significantly higher rates of violence toward separated and divorced,8,11 and never married women.11 Unfortunately, most national surveys have been limited to persons who are married or cohabitating,1,2,4,7 thus women who are assaulted or abused by former intimate partners or dating partners are excluded from the analyses. Given the evidence that these women are at the highest risk for abuse and violence, these groups should be included in future research on intimate partner abuse and violence.
Future research to examine the relationship between intimate partner abuse and sociodemographic factors needs to combine well-designed sampling strategies and validated measures of race/ethnicity and social class. Determinants of SES should include data for the victim, partner, and household. Furthermore, measures of abuse and SES should be validated in multiethnic populations to ensure cross-cultural validity and reliability. Although our research produced interesting findings, further research is needed to ascertain these relationships in different populations and to explore the underlying social and cultural factors, including immigration and acculturation, that potentially impact the occurrence of partner abuse.
Consistent with prior research on psychiatric symptoms among abused women patients,14,20 we found a significant association between reported depression symptoms and partner abuse history. Unlike the prior study, our research focused exclusively on violence and abuse perpetrated by intimate partners. In addition, our findings confirm the association among ethnically diverse low-income women patients. Although the temporal or causal relationship cannot be established, understanding that partner abuse often coexists with physical and mental health problems is essential to improving the quality of health services for abused patients. In general, women who are identified in a clinic setting as abused should be evaluated for depression.
The findings in this study are subject to limitations. The sample was drawn from three clinics in an urban area and cannot be generalized to all ethnically diverse primary care clinics. While our study had an adequate response rate, we were unable to sample the estimated 10% of low-income patients without telephones,27 which limited the representation of our sample. In addition, this study is limited by self-reporting of extremely sensitive issues which could underestimate the prevalence.
Primary care providers encounter many patients who have a history of intimate partner abuse. Our finding that 15% of women primary care patients have been abused (physically, sexually, or psychologically) by an intimate partner in the past year and an additional 36% have been abused at some time in their lives is cause for concern and action. The U.S. Preventive Services Task Force, as well as many national health care organizations, recommends routine inquiry for intimate partner abuse by health care providers.28 Health care professionals who provide primary care to women in any type of medical setting have the opportunity and obligation to ascertain the occurrence and severity of intimate partner abuse. Furthermore, clinicians should provide abused patients with referrals to available resources and, if requested, intervene in ways that maintain their safety and confidentiality and encourage empowerment.
Acknowledgments
This research was supported by the Picker Commonwealth Foundation and by a grant from the Center for Aging in Diverse Communities, funded by the National Institute on Aging.
We wish to thank Drs. Kevin Grumbach and Elizabeth McLoughlin for assistance with study design, Wendy Sheldon and Liza Pressor for data collection, Gregory Nah for data management, and Dr. Michele Manos for manuscript review. In addition, we thank the many San Francisco domestic violence advocates for their input into the survey content and design and the women who participated in this study.
REFERENCES
- 1.Straus M, Gelles R. Societal change and change in family violence from 1975 to 1985 as revealed by two national surveys. J Marriage Fam. 1986;48:465–79. [Google Scholar]
- 2.Plichta SB. Violence and abuse: implications for women's health. In: Falik MM, Collins KS, editors. Women's Health: The Commonwealth Fund Survey. Baltimore, Md: Johns Hopkins University Press; 1996. pp. 237–70. In: [Google Scholar]
- 3.Hampton RL, Gelles RJ, Harrop JW. Is violence in black families increasing? A comparison of 1975 and 1985 national survey rates. J Marriage Fam. 1989;51:969–80. [Google Scholar]
- 4.Sorenson SB, Upchurch DM, Shen H. Violence and injury in marital arguments: risk patterns and gender differences. Am J Public Health. 1996;86:35–40. doi: 10.2105/ajph.86.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Justice. Violence by Intimates: Analysis of Data on Crimes by Current or Former Spouses, Boyfriends, and Girlfriends. Washington, DC: U.S. Department of Justice; 1998. pp. 1–46. Pub no. NCJ–167237. [Google Scholar]
- 6.Straus MA, Smith C. In: Violence in Hispanic families in the United States: incidence rates and structural interpretations. Straus MA, Gelles RJ, editors. New Brunswick, NJ: Transaction Publishers; 1990. pp. 341–71. In Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. [Google Scholar]
- 7.Kantor GK, Jasinski JL, Aldarondo E. Sociocultural status and incidence of marital violence in Hispanic families. Violence Victims. 1994;9:207–22. [PubMed] [Google Scholar]
- 8.Neff JA, Holamon B, Schluter TD. Spousal violence among Anglos, Blacks, and Mexican Americans: the role of demographic variables, psychosocial predictors, and alcohol consumption. J Fam Violence. 1995;20:1–21. [Google Scholar]
- 9.Lockhart LL. A reexamination of the effects of race and social class on the incidence of marital violence: a search for reliable differences. J Marriage Fam. 1987;49:603–10. [Google Scholar]
- 10.Sorenson SB, Telles CA. Self-reports of spousal violence in a Mexican-American and non-Hispanic White population. Violence Victims. 1991;6:3–15. [PubMed] [Google Scholar]
- 11.Buehler J, Dixon B, Toomey K. Lifetime and annual incidence of intimate partner violence and resulting injuries—Georgia, 1995. Morb Mort Week Rep. 1998;47:849–53. [PubMed] [Google Scholar]
- 12.Rath GL, Jarratt LG, Leonardson G. Rates of domestic violence against adult women by men partners. J Am Board Fam Pract. 1989;2:227–33. [PubMed] [Google Scholar]
- 13.Gin NE, Rucker L, Frayne S, Cygan R, Hubbel FA. Prevalence of domestic violence among patients in three ambulatory care internal medicine clinics. J Gen Intern Med. 1991;6:317–22. doi: 10.1007/BF02597429. [DOI] [PubMed] [Google Scholar]
- 14.McCauley J, Kern DE, Kolodner K, et al. The “battering syndrome”: prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann Intern Med. 1995;123:737–46. doi: 10.7326/0003-4819-123-10-199511150-00001. [DOI] [PubMed] [Google Scholar]
- 15.Wagner PJ, Mongan P, Hamrick D, Hendrick LK. Experience of abuse in primary care patients: racial and rural differences. Arch Fam Med. 1995;4:956–62. doi: 10.1001/archfami.4.11.956. [DOI] [PubMed] [Google Scholar]
- 16.Campbell JC, Lewandowski LA. Mental and physical health effects of intimate partner violence on women and children. Psychiatr Clin No Am. 1997;20:353–74. doi: 10.1016/s0193-953x(05)70317-8. [DOI] [PubMed] [Google Scholar]
- 17.Resnick HS, Acierno R, Kilpatrick DG. Health impact of interpersonal violence 2: medical and mental health outcomes. Behav Med. 1997;23:65–78. doi: 10.1080/08964289709596730. [DOI] [PubMed] [Google Scholar]
- 18.Scholle SH, Rost KM, Golding JM. Physical abuse among depressed women. J Gen Intern Med. 1998;13:607–13. doi: 10.1046/j.1525-1497.1998.00183.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stark E, Flitcraft A. Killing the beast within: woman battering and female suicidality. Int J Health Serv. 1995;25:43–64. doi: 10.2190/H6V6-YP3K-QWK1-MK5D. [DOI] [PubMed] [Google Scholar]
- 20.McCauley J, Kern DE, Kolodner K, Derogatis LR, Bass EB. Relation of low-severity violence to women's health. J Gen Intern Med. 1998;13:687–91. doi: 10.1046/j.1525-1497.1998.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stark E, Flitcraft AH. Woman battering. In: Wallace RB, editor. Maxcy-Rosenau-Last Public Health and Preventive Medicine. 14th ed. Stanford, Conn: Appleton & Lange; 1998. pp. 1231–8. In: [Google Scholar]
- 22.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression: two questions are as good as many. J Gen Intern Med. 1997;12:439–45. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183–205. [Google Scholar]
- 24.McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy: severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267:3176–8. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- 25.Soeken K, Parker B, McFarlane J, Lominak MC. The Abuse Assessment Screen: a clinical instrument to measure frequency, severity and perpetrator of abuse against women. In: Campbell J, editor. Empowering Survivors of Abuse: Health Care for Battered Women and Their Children. Newbury Park, Calif: Sage Publications; 1998. In: [Google Scholar]
- 26.Brislin RW. Back-translation for cross-cultural research. J Cross-Cultural Psych. 1970;1:185–216. [Google Scholar]
- 27.Bureau of the Census, Economics and Statistics Administration. Race and Hispanic Origin: 1990 Census Data. Washington, DC: U.S. Department of Commerce; 1991. [Google Scholar]
- 28.U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. 2nd ed. Alexandria, Va: International Medical Publications Incorporated; 1996. pp. 555–65. [Google Scholar]