Abstract
OBJECTIVE
Both physicians and patients view advance directives as important, yet discussions occur infrequently. We assessed differences and correlations between physicians’ and their patients’ desires for end-of-life care for themselves.
MEASUREMENTS AND MAIN RESULTS
Study physicians (n = 78) were residents and faculty practicing in an inner-city, academic primary care general internal medicine practice. Patients (n = 831) received primary care from these physicians and were either at least 75 or between 50 and 74 years of age, with selected morbid conditions. Physicians and patients completed identical questionnaires that included an assessment of their preferences for six specific treatments if they were terminally ill. There were significant differences between physicians' and patients' preferences for all six treatments (p < .0001), with physicians wanting less treatment than their patients for five of them. Patients desiring more care (p < .01) were more often male (odds ratio [OR] 1.7), African-American (OR 1.6), and older (OR 1.02 per year). There were no such correlates with physicians' preferences. A treatment preference score was calculated from respondents' desires to receive or refuse the six treatments. Physicians' scores were highly correlated with those of their enrolled primary care patients (r = .51, p < .0001).
CONCLUSIONS
Although patients and physicians as groups differ substantially in their preferences for end-of-life care, there was significant correlation between individual academic physicians' preferences and those of their primary care patients. Reasons for this correlation are unknown.
Keywords: end-of-life care, advance directives, patient preferences, physician preferences
In 1990, Congress passed the Patient Self-Determination Act, which became effective in December 1991. The Act requires hospitals to inform all admitted patients of their rights to state what types of care they desire should they become critically ill and unable to participate in medical decision making.1–3 Unfortunately, the Act focuses on patients sufficiently ill to require hospitalization, which does not foster discussions between physicians and their patients about advance care planning.4 Despite both doctors’ and patients’ beliefs that such discussions are important,5–7 they occur infrequently.7–9 There is a growing opinion that such discussions are best held between patients and their personal physicians in the ambulatory care setting.10–12
Despite the burgeoning literature concerning advance directives,13 little is known about physicians’ own desires for end-of-life care.14–17 To shed some light on this subject, we surveyed faculty and resident physicians practicing in an inner-city academic general internal medicine practice and conducted detailed interviews with more than 800 of their primary care patients. Physicians and their patients were asked the same questions about their preferences for end-of-life treatments.18–19 We then compared and contrasted physicians’ preferences for end-of-life care with the preferences for their primary care patients. We hypothesized that physicians and patients, in general, would have very different preferences for treatment when faced with a terminal illness, and that physicians would want less aggressive treatment than patients. Because of the documented lack of discussion between physicians and their patients about end-of-life care,7–9 we anticipated that there would be no association between physicians’ own preferences for end-of-life care and those of their patients.
METHODS
Study Site and Physician Subjects
Indiana University’s Institutional Review Board gave its approval to conduct this study in the General Medicine Practice (GMP) of the Regenstrief Health Center, a multispecialty academic ambulatory care center affiliated with an urban teaching hospital in Indianapolis.20 All GMP physicians, both faculty and residents, deliver primary care to stable panels of patients for the duration of their appointments in the Department of Medicine. Although residents have independent decision-making authority, they briefly present most patients to their attending faculty after each visit.
As part of a larger study assessing the impact of advance directives on health care, all GMP attending general internist faculty and residents (predominantly categorical internal medicine residents and residents in a combined medicine-pediatrics residency) were asked to complete a self-administered questionnaire assessing their knowledge, attitudes, and beliefs concerning advance directives and end-of-life care. We excluded from analysis those physicians who first entered the GMP as first-year residents (interns) during the study because of their lack of clinical experience and time to establish a rapport with their assigned primary care patients. Eligible physicians were asked to provide personal demographic information, answer questions about their degree of religiosity, and respond to questions, first published by Danis et al.,18,19 about their own preferences for six selected aspects of medical care if they developed “a condition where my doctors believe that there is little hope that I will recover from my illness and that my death is likely no matter what is done.” The six aspects of care were hospitalization, intensive care, cardiac resuscitation, surgery, mechanical ventilation, and medically provided nutrition and hydration. Respondents had to select one of three responses to each treatment option: “Yes, I would want it,” “No, I would not want it,” or “I don’t know.” (The survey instrument is available from the authors on request.) We chose to focus on this terminal illness scenario to simplify the process of establishing advance directives. Local experience with a more comprehensive advance directive form (with four scenarios and multiple responses per aspect of care discussed) was discouraging; most patients could not (or would not) complete it.
In the last two months of an academic year, when all current residents and faculty had practiced in the GMP for a minimum of 10 months, the questionnaire was distributed by research assistants to each physician at the beginning of a GMP practice session. The physicians were asked to complete the questionnaire then or before the end of that session, if possible. Nonrespondents received additional questionnaires up to a maximum of four, the fourth being hand-delivered by one of the study investigators.
Patient Subjects
For this study, we targeted patients who were at risk of morbid events and were thus the highest-priority candidates for discussing end-of-life care. Eligible patients were either very old (75 years of age or older) or were between 50 and 74 years of age and suffering from one or more of the following morbid conditions: congestive heart failure, ischemic heart disease, cancer other than cutaneous basal cell carcinoma, chronic lung disease, stroke or transient ischemic attacks, chronic renal insufficiency, or chronic liver disease.
Using diagnoses, test results, and appointment data stored in the Regenstrief Medical Record System,21 we generated daily lists of eligible patients with scheduled GMP appointments. Before visiting their physicians, eligible patients were approached in the GMP waiting room by a research assistant who invited them to participate in a study of advance directives. After accompanying assenting patients to a private interviewing area and obtaining patient consent, trained interviewers administered the Pfeiffer Short Portable Mental Status Questionnaire.22 Using standard scoring, we excluded patients who failed this cognitive function screen because their responses on the various questionnaires would be unreliable. We were unable to recruit patients from a small number of GMP sessions because these patients were being recruited for another study with similar eligibility criteria. We also excluded GMP patients who could not speak English, had hearing impairments, lived in nursing homes, or were prisoners.
Methods for administering the questionnaires for this study have been previously described.23 Briefly, consenting eligible patients were interviewed before and immediately after they had seen their primary care physicians on the day of enrollment. (In no cases were patients interviewed on the day that their physicians received their study questionnaire.) To help the patients respond, the interviewers used large-print cue cards showing the response options. Using a questionnaire identical (including the accompanying text) to that described above for physicians, interviewers asked patients about their preferences for medical treatments if they were terminally ill. All interviews and responses to patient questions were strictly scripted. Patients were also asked questions concerning their health status, social support, attitudes and beliefs regarding advance directives, and religiosity. Finally, during their postvisit interviews, patients were asked whether they had discussed advance directives with their physicians that day. From patients’ electronic medical records, we extracted clinical data, including the number of previous visits during which each patient had been treated by his or her current primary care physician.
Statistical Analyses
For each physician and patient, we calculated a treatment preference score using Dani’s methods18: each “yes” answer was scored as +1, each “no” was scored as −1, and each “don’t know” answer was scored as 0. The treatment preference score was the sum of all six items; therefore the maximum possible score was +6 for subjects wanting all six treatments if they were terminally ill, while the minimum score would be −6 for respondents not wanting any of the six treatments. Both patients and physicians were separated into three groups based on their treatment preference scores as suggested by Danis18,19: least aggressive (treatment preference score −6 to −2 inclusive), moderately aggressive (treatment preference score −1 to +1), and most aggressive (treatment preference score +2 to +6).
We used Student’s t tests and corrected χ2 tests to assess bivariate relations among continuous and categorical data, respectively. Using polychotomous logistic regression separately for physicians and patients, we also determined which of the factors listed above were independently associated with preferences for aggressive end-of-life treatments. Polychotomous logistic regression is used when the dependent variable has a natural ordering. The procedure fits a parallel line regression model to the data that is based on the cumulative distribution probabilities of the dependent variable.24
We assessed the relations between physicians’ treatment preference scores and the treatment preference scores of their patients in two ways. First, with the physician as the unit of analysis, we used Pearson correlation to compare the actual treatment preference score for each physician with the mean treatment preference score for all of his or her enrolled patients. Second, with the mean of each physician’s enrolled patients’ treatment preference scores as the dependent variable, we used multiple liner regression to assess the effects of physicians’ characteristics, including their treatment preference score category as suggested by Danis,18 age, gender, status (a categorical variable indicating resident or faculty), and the number of previous primary care encounters with each enrolled patient (categorized as 0, 1–5, or ≥ 6).
RESULTS
There were 158 physicians practicing in the GMP at the time of this study; 137 (87%) returned completed questionnaires. Fifty-nine (43%) of these physicians and their surveys were excluded from this analysis because the physicians either were new first-year residents in the later months of the study or were practicing in GMP sessions from which no patients were recruited. Of the 78 physicians retained for this analysis, 54 were residents and 24 were full-time faculty general internists.
Over the 9-month enrollment period, 1,409 potentially eligible patients kept scheduled appointments with their primary care physicians. Of these, 161 (12%) were not eligible: 83 failed the Pfeiffer mental status examination, 24 lived in a nursing home, 22 were deaf or otherwise noncommunicative, 13 were prisoners, 8 did not speak English, and 11 had some other reason for exclusion. Of the remaining 1,248 truly eligible patients, 156 (12%) refused to participate, 41 (3%) were missed by the research assistants, and 1,051 (85%) were enrolled in the study and completed the enrollment questionnaires. The 78 physicians in this analysis were primary care physicians for 831 (79%) of these patients. The remaining 220 patients (21%) were excluded from analysis because their primary care physicians began their first year of residency during the study.
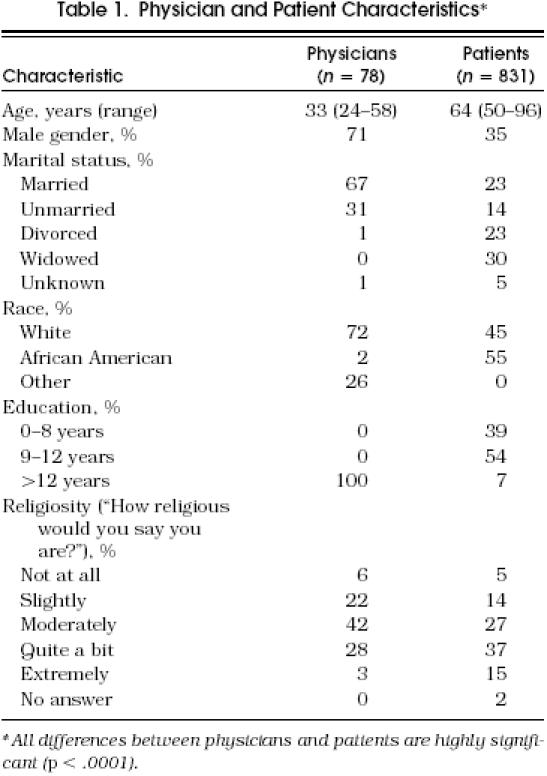
Table 1 shows descriptive data for the 78 physicians and their 831 enrolled patients. The mean number of patients per physician was 11 (range 1–26). As expected, physicians were much younger than their patients and were predominantly men while the majority of enrolled patients were women. The majority of physicians were married whereas the majority of patients were either divorced or widowed. Only 2% of the physicians were African-American compared with more than half the patients. (Because of the small number of African-American physicians, physician race was not included in any analyses). Patients tended to consider themselves more religious than did the physicians. All of the differences between physicians and their enrolled patients were statistically significant (p < .01).
Table 1.
Physician and Patient Characteristics*
The mean number of previous visits of enrolled patients to their primary care physicians was 4.2 ± 6.0 (SD) (range 0–37). Enrolled patients had a mean of less than 1 previous primary care visit to 16 study physicians (21%), a mean of 1 to 5 previous visits to 45 physicians (58%), and more than 5 visits to the remaining 17 physicians (21%). Only 2.6% of the patients reported having discussed advance directives with their physicians on the day they were enrolled in this study, and fewer than 5% stated that they had ever discussed advance care issues with their current primary care physician.
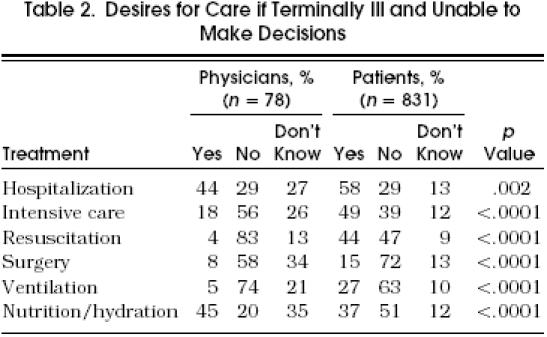
As groups, physicians and patients had substantial differences in their preferences for end-of-life treatment (Table 2). Patients desired five of the six treatment options more often than the physicians, the exception being artificial nutrition or hydration, which physicians more often desired if terminally ill. Also, for five of the six treatment options, physicians answered “don’t know” more than twice as often as patients.
Table 2.
Desires for Care if Terminally III and Unable to Make Decisions
Using a polychotomous logistic regression procedure, we found no significant association between physicians’ age, status (resident or faculty), religiosity, or gender and their treatment preference scores. However patients’ treatment preference scores were higher among African Americans (odds ratio [OR] 1.6; 95% confidence interval [CI] 1.1, 2.2; p = .008), males (OR 1.7; 95% CI 1.2, 2.3; p = .002) and older patients (OR per year = 1.02; 95% CI 1.01, 1.03; p < .0001). Religiosity was not a significant correlate of patients’ preferences for end-of-life care.
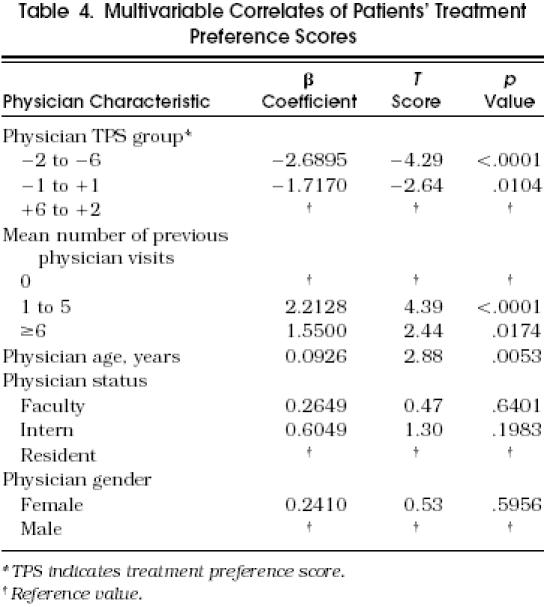
There was a significant positive correlation between physicians’ treatment preference scores and the mean scores of their enrolled patients (r = .51, p < .0001). As shown in Table 3, the mean treatment preference score for enrolled patients of the 8 physicians (10%) in the most aggressive group was 0.760 compared with −0.746 for patients of the 24 physicians (31%) in the moderately aggressive group and −1.567 for patients of the 46 physicians (59%) in the least aggressive group. Using multivariable linear regression to control for other physician characteristics, we found that the primary care physicians’ treatment preference score category remained the strongest correlate with the mean score of their enrolled patients, followed by the number of previous visits to the physician and the physician’s age (Table 4 Physicians’ gender and resident or faculty status had no significant independent association with their enrolled patients’ mean treatment preference scores.
Table 3.
Correlation Between Physician and Patient Treatment Preference Scores
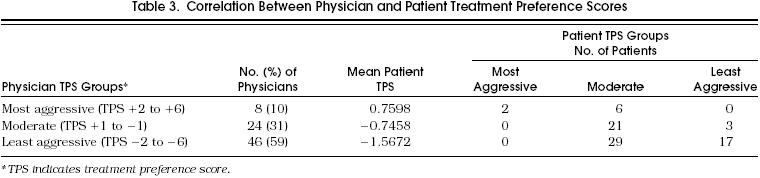
Table 4.
Multivariable Correlates of Patients' Treatment Preference Scores
DISCUSSION
As we expected, there were clear differences in preferences for end-of-life care between inner-city patients and the academic primary care physicians (general internists and internal medicine residents) who care for them. This is to be expected because of the dramatically different demographic and socioeconomic characteristics between the two. Two thirds of the physicians were residents in training, while patients eligible for this study had to be at least 50 years old. The racial mix between the two groups was dramatically different as well, with physicians being overwhelmingly white (with a substantial proportion being of Asian and Middle Eastern descent) whereas patients were slightly more than half African-American, the rest being white. There were also obvious socioeconomic differences.
Contrary to our hypothesis and despite the significant differences in preferences for end-of-life care among physicians and patients as groups, there was a substantial positive correlation between the preferences of individual physicians and those of their patients (Table 3). There are two potential explanations for this unanticipated result. First, patients might select their primary care physicians for some characteristic that is correlated with treatment preferences at the end of life. However, GMP patients seldom have the opportunity to choose their primary care providers. Most patients are “inherited” by incoming physicians who replace physicians that have just left the practice. Completely new GMP patients either are assigned to available GMP appointments on a rotating basis or are given appointments with physicians who recently cared for them in the hospital and to whom they were again assigned on a rotating basis.
Alternatively, physicians might have directly influenced their patients’ end-of-life treatment preferences. Because fewer than 5% of the patients enrolled in this study had ever discussed advance directives with their current physicians, a more subtle interaction between doctor and patient is most likely responsible for this correlation. Because the clinical encounter is under the physician’s control, it is likely that the physicians are affecting patients’ preferences and not vice versa. For example, during clinical encounters, physicians may be assuming more aggressive or passive postures toward diagnosis and treatment. Some physicians may be generally optimistic about treatments and their outcomes while others may be more skeptical or pessimistic. Such attitudes on the part of the physicians may affect the hope or skepticism with which their patients view therapeutic options.
We could find only one previous study in which physicians’ preferences for end-of-life care were directly compared to their patients’ preferences for such care.16 In this study, which focused on four aspects of care (resuscitation, ventilation, artificial nutrition or hydration, and hospitalization), there was a negative correlation between physicians’ preferences for their own end-of-life care and the preferences of their patients. The meaning of these results is unclear, however, because only one correlation was statistically significant among 12 comparisons made on data from only 16 physicians and 22 patients.
We also found that patients with no previous visits to their primary care physicians had significantly lower treatment preference scores (Table 4). Greater familiarity with their doctors may lead patients to trust their physicians to know when to discontinue aggressive therapy if it is futile. Such patients may also trust their physicians to aggressively treat their discomfort. Perhaps physicians and patients who have “invested” more in their relationship are more willing to work together to prolong life, regardless of the risk of bad outcomes. Schneiderman et al. provide tantalizing data that may bear on this point.16 They found that physicians could not predict their outpatients’ preferences for life-sustaining care. However, physicians’ estimates of patients’ preferences were significantly correlated with the physicians’ own preferences for such care. Perhaps, as the doctor-patient relationship matures, physicians do more than project their personal desires on their patients; they may actually modify their patients’ preferences to be more in line with their own.
It is interesting, and perhaps a bit disconcerting, to discover that physicians’ own preferences for end-of-life care may influence their patients’ preferences even in the absence of formal discussions. Studies have shown that neither their physicians nor family members can accurately predict what types of care patients would want at the end of their lives.16,–30 The fact that the physicians and patients we studied, as groups, did not agree on types of end-of-life care they would like for themselves calls for explicit discussions of advance care issues. Physicians should play an important role in shared decision making about such complicated issues as end-of-life care without unduly impressing their own opinions on their patients. Specifically, physicians can: provide accurate, objective information about patients’ diagnoses and prognoses; listen carefully and discuss openly patients’ fears and concerns; and solicit, discuss, and record their values and preferences for terminal care.
This study has several limitations. It only involved academic physicians practicing in one inner-city site. Therefore, the results may not be applicable to other clinical venues. However, doctor-patient communication is likely to be most constrained between elderly, poor, inner-city minority patients and young physicians from very different socioeconomic backgrounds.31,32 This study, the first of its kind comparing opinions of physicians and their own primary care physicians, has broad implications and should be repeated in different clinical venues, especially community practices in which formal doctor-patient relationships are likely to be stronger and more long-lived.
The survey medium itself may have confounded the results: physicians completed a written questionnaire, but patients were interviewed. Although the mode of data collection might have affected the results, it should bias them toward there being less correlation between physicians and patients. Regardless, we had little choice about how we interviewed patients and physicians. Our pilot studies demonstrated that the sick and elderly patients to whom this study was targeted could not reliably complete written questionnaires on their own. Conversely, the physicians were too busy to arrange formal interviews. They often completed the 15- to 20-minute questionnaire between patient visits. These problems are likely to exist in other clinical sites and would be difficult to overcome.
Nevertheless, our data show that, despite patients generally wanting more of the targeted treatments than physicians, patients’ treatment preferences for terminal care were significantly related to those of their primary care physicians. This relation remained after controlling for their differences in age, gender, race, and religiosity. High-quality formal discussions need to occur,33 in which primary care physicians help their patients better understand the issues surrounding end-of-life decision making. The goal is to establish patient preferences that reflect their own values and desires rather than those of their physicians.
Acknowledgments
The authors thank the physicians, nurses, and patients in the General Medicine Practice of the Regenstrief Health Center for their patience and support of this study.
REFERENCES
- 1.White ML, Fletcher JC. The Patient Self-Determination Act: on balance, more help than hindrance. JAMA. 1991;266:410–2. doi: 10.1001/jama.1991.03470030110035. [DOI] [PubMed] [Google Scholar]
- 2.Wolf SM, Boyle P, Callahan D, et al. Sources of concern about the Patient Self-Determination Act. N Engl J Med. 1991;325:1666–71. doi: 10.1056/nejm199112053252334. [DOI] [PubMed] [Google Scholar]
- 3.La Puma J, Orentlichter D, Moss RJ. Advance directives on admission: clinical implications of the Patient Self-Determination Act of 1990. JAMA. 1991;266:402–5. doi: 10.1001/jama.266.3.402. [DOI] [PubMed] [Google Scholar]
- 4.Johnson RF, Jr, Baranowski-Birkmeier T, O’Donnel JB. Advance directives in the medical intensive care unit of a community teaching hospital. Chest. 1995;107:752–6. doi: 10.1378/chest.107.3.752. [DOI] [PubMed] [Google Scholar]
- 5.Lo B, McLeod GA, Saika G. Patients attitudes to discussing life-sustaining treatment. Arch Intern Med. 1986;146:1613–5. [PubMed] [Google Scholar]
- 6.Davidson KW, Hackler C, Caradine DR, McCord RS. Physicians’ attitudes on advance directives. JAMA. 1989;262:2415–9. [PubMed] [Google Scholar]
- 7.Emmanuel LL, Barry MJ, Stoeckle JD, Ettelson LM, Emmanuel EJ. Advance directives for medical care: a case for greater use. N Engl J Med. 1991;324:889–96. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 8.Gamble ER, McDonald PJ, Lichstein PR. Knowledge, attitudes, and behavior of elderly persons regarding living wills. Arch Intern Med. 1991;151:277–80. [PubMed] [Google Scholar]
- 9.Stelter KL, Elliott BA, Bruno CA. Living will completion in older adults. Arch Intern Med. 1992;152:954–9. [PubMed] [Google Scholar]
- 10.Wenger NS, Oye RK, Bellamy PE. Prior capacity of patients lacking decision making ability early in hospitalization: implications for advance directive administration. J Gen Intern Med. 1994;9:539–43. doi: 10.1007/BF02599276. [DOI] [PubMed] [Google Scholar]
- 11.Emmanuel LL. Does the DNR order need life-sustaining intervention? Time for comprehensive advance directives. Am J Med. 1989;86:87–90. doi: 10.1016/0002-9343(89)90234-9. [DOI] [PubMed] [Google Scholar]
- 12.Greco PJ, Schulman KA, Lavizzo-Mourey R, Hansen-Flaschen J. The Patient Self-Determination Act and the future of advance directives. Ann Intern Med. 1991;115:639–43. doi: 10.7326/0003-4819-115-8-639. [DOI] [PubMed] [Google Scholar]
- 13.Miles SH, Koepp R, Weber EP. Advance end-of-life treatment planning: a research review. Arch Intern Med. 1996;156:1062–8. [PubMed] [Google Scholar]
- 14.Hillier TA, Patterson JR, Hodges MO, Rosenberg MR. Physicians as patients: choices regarding their own resuscitation. Arch Intern Med. 1995;155:1289–93. doi: 10.1001/archinte.155.12.1289. [DOI] [PubMed] [Google Scholar]
- 15.Gillick MR, Hesse K, Mazzapica N. Medical technology at the end of life: what would physicians and nurses want for themselves. Arch Intern Med. 1993;153:2542–7. [PubMed] [Google Scholar]
- 16.Schneiderman LJ, Kaplan RM, Pearlman RA, Teetzel H. Do physicians’ own preferences for life-sustaining treatment influence their perceptions of patients’ preferences? J Clin Ethics. 1993;4:28–33. [PubMed] [Google Scholar]
- 17.Virmani J, Schneiderman LJ, Kaplan RM. Relationship of advance directives to physician-patient communication. Arch Intern Med. 1994;154:909–12. [PubMed] [Google Scholar]
- 18.Danis M, Southerland LI, Garrett JM, et al. A prospective study of advance directives for life-sustaining care. N Engl J Med. 1991;324:882–8. doi: 10.1056/NEJM199103283241304. [DOI] [PubMed] [Google Scholar]
- 19.Danis M, Garrett JM, Harris R, Patrick DL. Stability of choices about life-sustaining treatments. Ann Intern Med. 1994;120:567–73. doi: 10.7326/0003-4819-120-7-199404010-00006. [DOI] [PubMed] [Google Scholar]
- 20.Tierney WM, Miller ME, Hui SL, McDonald CJ. Practice randomization and clinical research: the Indiana experience. Med Care. 1991;29:JS57–64. [PubMed] [Google Scholar]
- 21.McDonald CJ, Tierney WM, Martin DK, Overhage JM. The Regenstrief Medical Record System: 20 years’ experience in hospital outpatient clinics and neighborhood health centers. MD Comput. 1992;9:206–17. [PubMed] [Google Scholar]
- 22.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 23.Dexter PR, Stump TE, Tierney WM, Wolinsky FD. The psychometric properties of the SF-36 health survey among older adults in the clinical setting. J Clin Geropsych. 1996;2:225–37. [Google Scholar]
- 24.Agresti A. New York, NY: John Wiley and Sons; 1992. Categorical Data Analysis; pp. 318–20. [Google Scholar]
- 25.Emmanuel EJ, Emmanuel LL. Proxy decision making for incompetent patients. JAMA. 1992;267:2067–71. [PubMed] [Google Scholar]
- 26.Seckler AB, Meier DE, Mulvihill M, Paris BE. Substituted judgment: how accurate are proxy predictions? Ann Intern Med. 1991;115:92–8. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]
- 27.Uhlmann RF, Pearlman RA, Cain KC. Physicians’ and spouses’ predictions of elderly patients’ resuscitation preferences. J Gerontol. 1988;43(suppl):M115–21. doi: 10.1093/geronj/43.5.m115. [DOI] [PubMed] [Google Scholar]
- 28.Zweibel NR, Cassel CK. Treatment choices at the end of life: a comparison of decisions by older patients and their physicians-selected proxies. Gerontologist. 1989;29:615–21. doi: 10.1093/geront/29.5.615. [DOI] [PubMed] [Google Scholar]
- 29.Gerety MB, Chiodo LK, Kanten DN, Tuley MR, Cornell JE. Medical treatment preferences of nursing home residents: relationship to function and concordance with surrogate decision-makers. J Am Geriatr Soc. 1993;41:953–60. doi: 10.1111/j.1532-5415.1993.tb06761.x. [DOI] [PubMed] [Google Scholar]
- 30.Hare J, Pratt C, Nelson C. Agreement between patients and their self-selected surrogates on difficult medical decisions. Arch Intern Med. 1992;152:1049–54. [PubMed] [Google Scholar]
- 31.Dula A. The life and death of Miss Mildred: an elderly black woman. Clin Geriatr Med. 1994;10:419–31. [PubMed] [Google Scholar]
- 32.Ventres W, Nichter M, Reed R, Frankel R. Limitation of medical care: an ethonographic analysis. J Clin Ethics. 1993;4:134–44. [PubMed] [Google Scholar]
- 33.Tulsky FA, Chesney MA, Lo B. How do medical residents discuss resuscitation with patients? J Gen Intern Med. 1995;10:436–42. doi: 10.1007/BF02599915. [DOI] [PubMed] [Google Scholar]


