Abstract
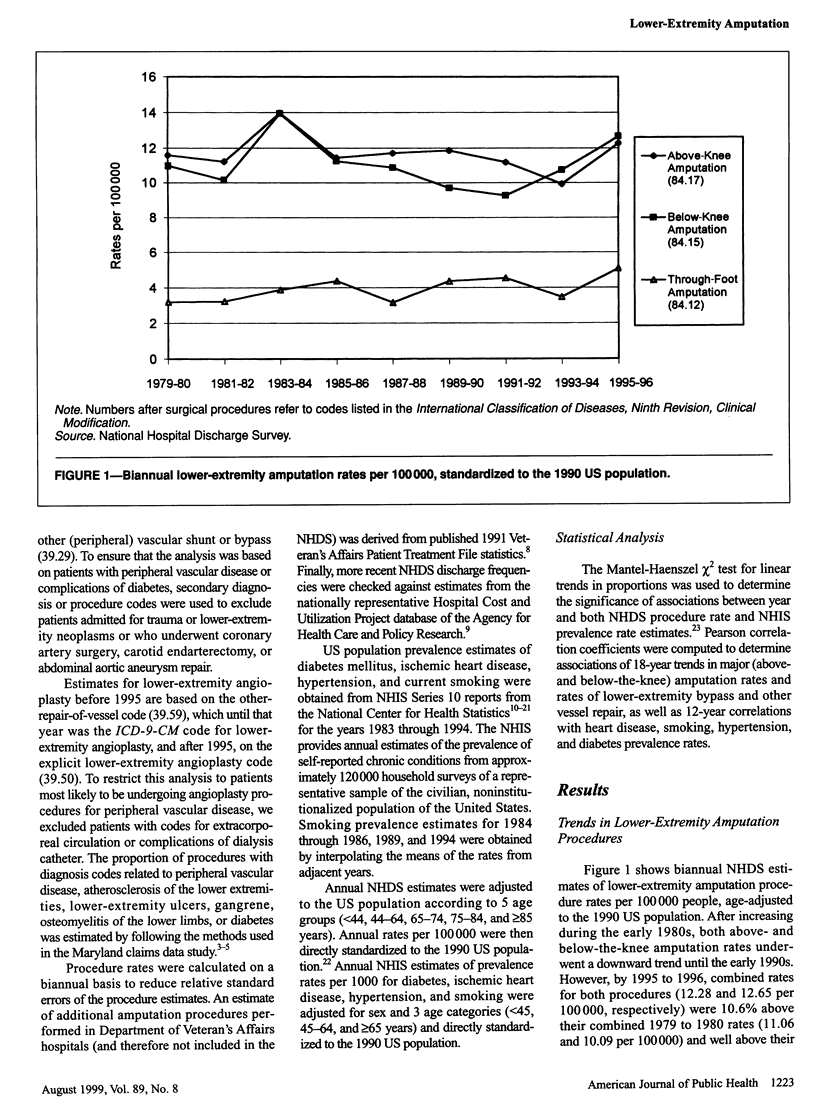
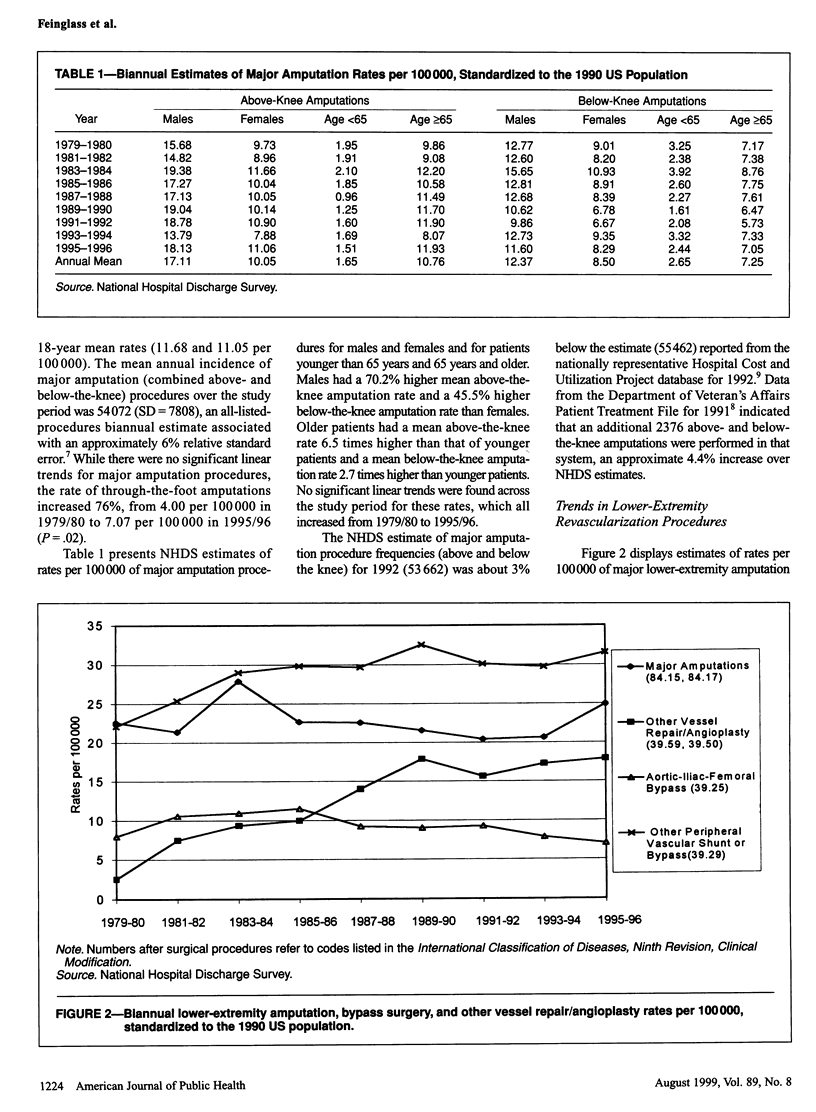
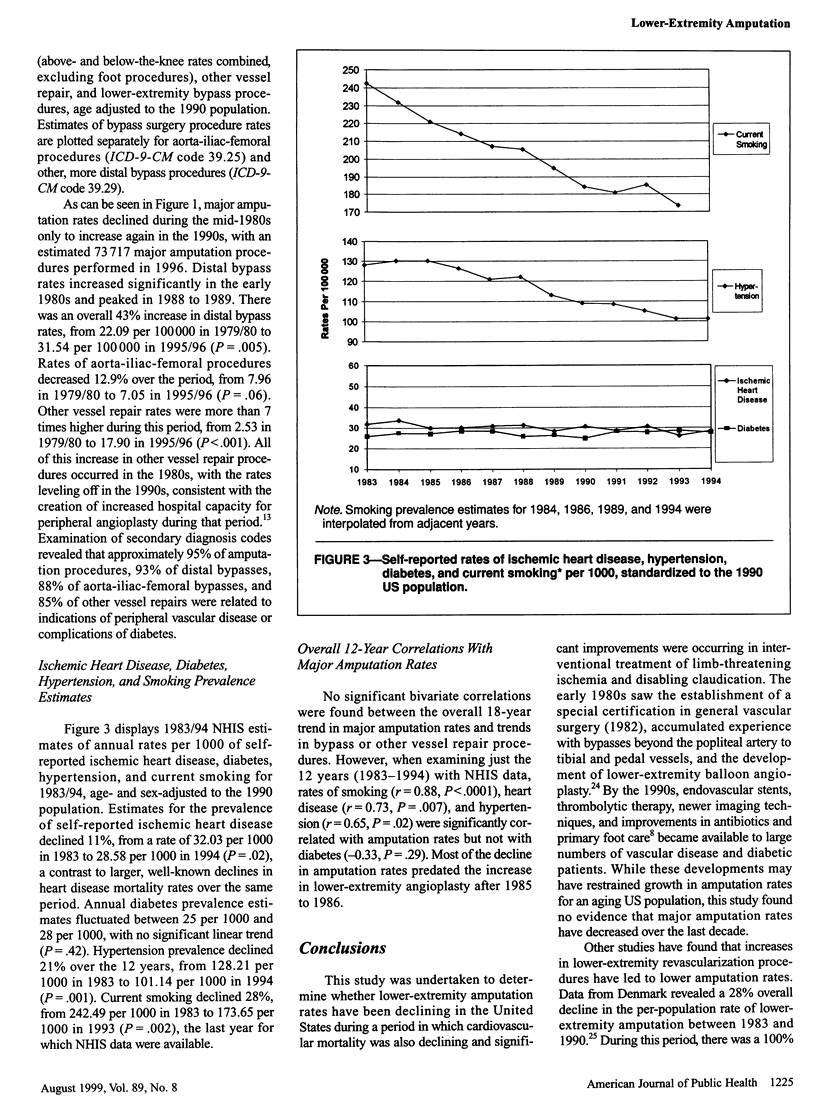
OBJECTIVES: This report describes trends in the rates of lower-extremity amputation and revascularization procedures and vascular disease risk factors. METHODS: We analyzed trends in National Hospital Discharge Survey data for 1979 through 1996 and in National Health Interview Study data for 1983 through 1994. RESULTS: Despite a decline between 1983/84 and 1991/92, by 1995/96 the rate of major amputation had increased 10.6% since 1979/80. The earlier 12-year decline was positively correlated with reductions in the prevalence of smoking (r = 0.88, P < .0001), hypertension (r = 0.65, P = .02), and heart disease (r = 0.73, P = .007), but not diabetes (r = -0.33, P = .29). During the 1980s, amputation and angioplasty rates were inversely correlated (r = -0.75, P = .001), but the decline in amputation rates occurred before the increase in angioplasty. The major amputation rate, which has increased since 1993, was 24.95 per 100,000 people in 1996. CONCLUSIONS: Major amputation rates fell in the years following the diffusion of distal bypass surgery but before the widespread use of peripheral angioplasty. Because disease prevalence and primary amputation rates are unknown, it is difficult to estimate the contribution of recent improvements in vascular surgery to limb preservation.
Full text
PDF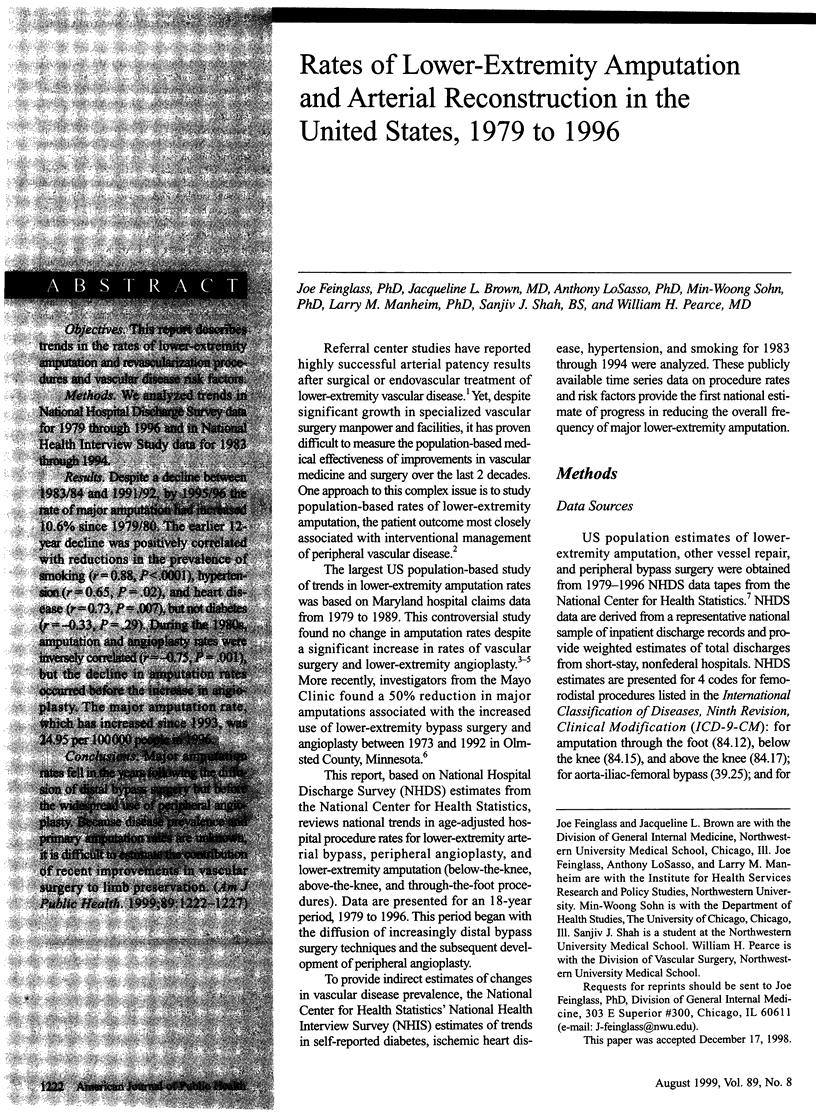

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Becker G. J., Ferguson J. G., Bakal C. W., Kinnison M. L., McLean G. K., Pentecost M. J., Perler B. A., van Breda A., Veith F. J. Angioplasty, bypass surgery, and amputation for lower extremity peripheral arterial disease in Maryland: a closer look. Radiology. 1993 Mar;186(3):635–638. doi: 10.1148/radiology.186.3.8430166. [DOI] [PubMed] [Google Scholar]
- Becker G. J., Ferguson J. G., Bakal C. W., Kinnison M. L., McLean G. K., Pentecost M. J., Perler B. A., van Breda A., Veith F. J. Angioplasty, bypass surgery, and amputation for lower extremity peripheral arterial disease in Maryland: a closer look. Radiology. 1993 Mar;186(3):635–638. doi: 10.1148/radiology.186.3.8430166. [DOI] [PubMed] [Google Scholar]
- De Frang R. D., Taylor L. M., Jr, Porter J. M. Basic data related to amputations. Ann Vasc Surg. 1991 Mar;5(2):202–207. doi: 10.1007/BF02016758. [DOI] [PubMed] [Google Scholar]
- Ebskov L. B., Schroeder T. V., Holstein P. E. Epidemiology of leg amputation: the influence of vascular surgery. Br J Surg. 1994 Nov;81(11):1600–1603. doi: 10.1002/bjs.1800811111. [DOI] [PubMed] [Google Scholar]
- Hallett J. W., Jr, Byrne J., Gayari M. M., Ilstrup D. M., Jacobsen S. J., Gray D. T. Impact of arterial surgery and balloon angioplasty on amputation: a population-based study of 1155 procedures between 1973 and 1992. J Vasc Surg. 1997 Jan;25(1):29–38. doi: 10.1016/s0741-5214(97)70318-5. [DOI] [PubMed] [Google Scholar]
- Hunink M. G., Goldman L., Tosteson A. N., Mittleman M. A., Goldman P. A., Williams L. W., Tsevat J., Weinstein M. C. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. JAMA. 1997 Feb 19;277(7):535–542. [PubMed] [Google Scholar]
- Hunink M. G., Wong J. B., Donaldson M. C., Meyerovitz M. F., Harrington D. P. Patency results of percutaneous and surgical revascularization for femoropopliteal arterial disease. Med Decis Making. 1994 Jan-Mar;14(1):71–81. doi: 10.1177/0272989X9401400109. [DOI] [PubMed] [Google Scholar]
- Isner J. M., Rosenfield K. Redefining the treatment of peripheral artery disease. Role of percutaneous revascularization. Circulation. 1993 Oct;88(4 Pt 1):1534–1557. doi: 10.1161/01.cir.88.4.1534. [DOI] [PubMed] [Google Scholar]
- Leibson C. L., O'Brien P. C., Atkinson E., Palumbo P. J., Melton L. J., 3rd Relative contributions of incidence and survival to increasing prevalence of adult-onset diabetes mellitus: a population-based study. Am J Epidemiol. 1997 Jul 1;146(1):12–22. doi: 10.1093/oxfordjournals.aje.a009187. [DOI] [PubMed] [Google Scholar]
- MANTEL N., HAENSZEL W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959 Apr;22(4):719–748. [PubMed] [Google Scholar]
- Murabito J. M., D'Agostino R. B., Silbershatz H., Wilson W. F. Intermittent claudication. A risk profile from The Framingham Heart Study. Circulation. 1997 Jul 1;96(1):44–49. doi: 10.1161/01.cir.96.1.44. [DOI] [PubMed] [Google Scholar]
- Pell J. P., Whyman M. R., Fowkes F. G., Gillespie I., Ruckley C. V. Trends in vascular surgery since the introduction of percutaneous transluminal angioplasty. Br J Surg. 1994 Jun;81(6):832–835. doi: 10.1002/bjs.1800810613. [DOI] [PubMed] [Google Scholar]
- Stanley J. C., Barnes R. W., Ernst C. B., Hertzer N. R., Mannick J. A., Moore W. S. Vascular surgery in the United States: workforce issues. Report of the Society for Vascular Surgery and the International Society for Cardiovascular Surgery, North American Chapter, Committee on Workforce Issues. J Vasc Surg. 1996 Jan;23(1):172–181. doi: 10.1016/s0741-5214(05)80050-3. [DOI] [PubMed] [Google Scholar]
- Tunis S. R., Bass E. B., Klag M. J., Steinberg E. P. Variation in utilization of procedures for treatment of peripheral arterial disease. A look at patient characteristics. Arch Intern Med. 1993 Apr 26;153(8):991–998. [PubMed] [Google Scholar]
- Tunis S. R., Bass E. B., Steinberg E. P. The use of angioplasty, bypass surgery, and amputation in the management of peripheral vascular disease. N Engl J Med. 1991 Aug 22;325(8):556–562. doi: 10.1056/NEJM199108223250806. [DOI] [PubMed] [Google Scholar]
- Weaver F. M., Burdi M. D., Pinzur M. S. Outpatient foot care: correlation to amputation level. Foot Ankle Int. 1994 Sep;15(9):498–501. doi: 10.1177/107110079401500908. [DOI] [PubMed] [Google Scholar]


