Abstract
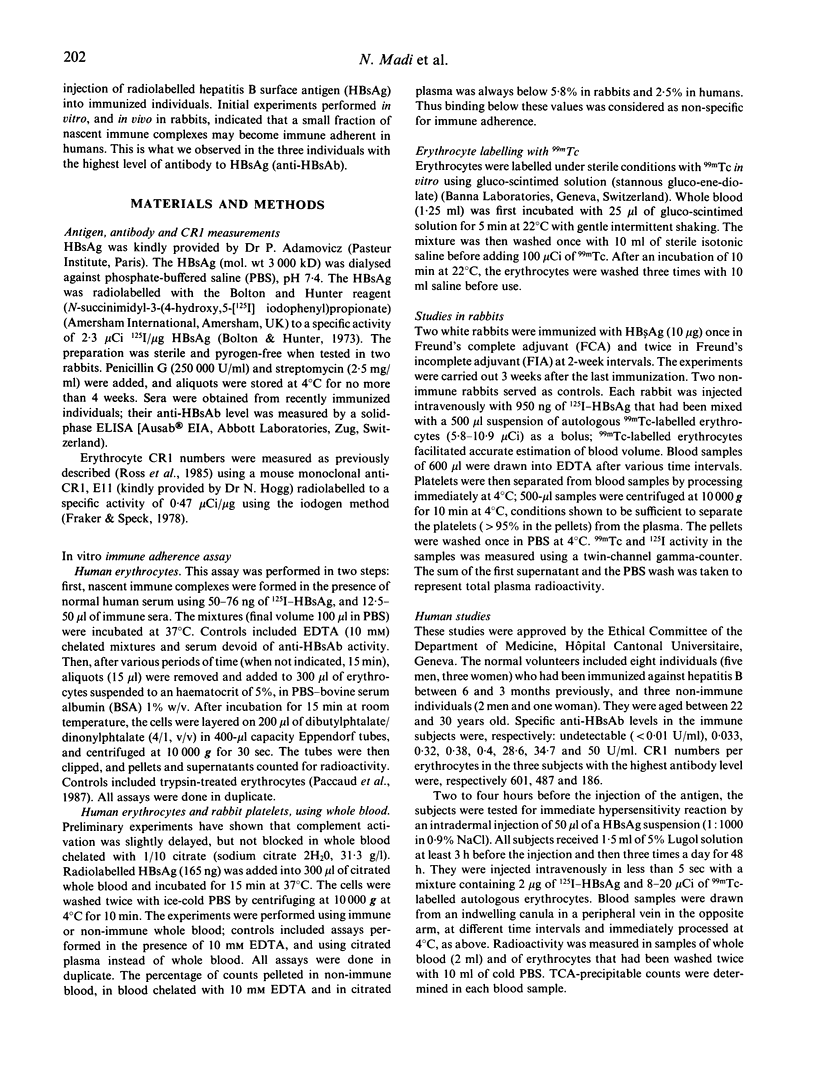
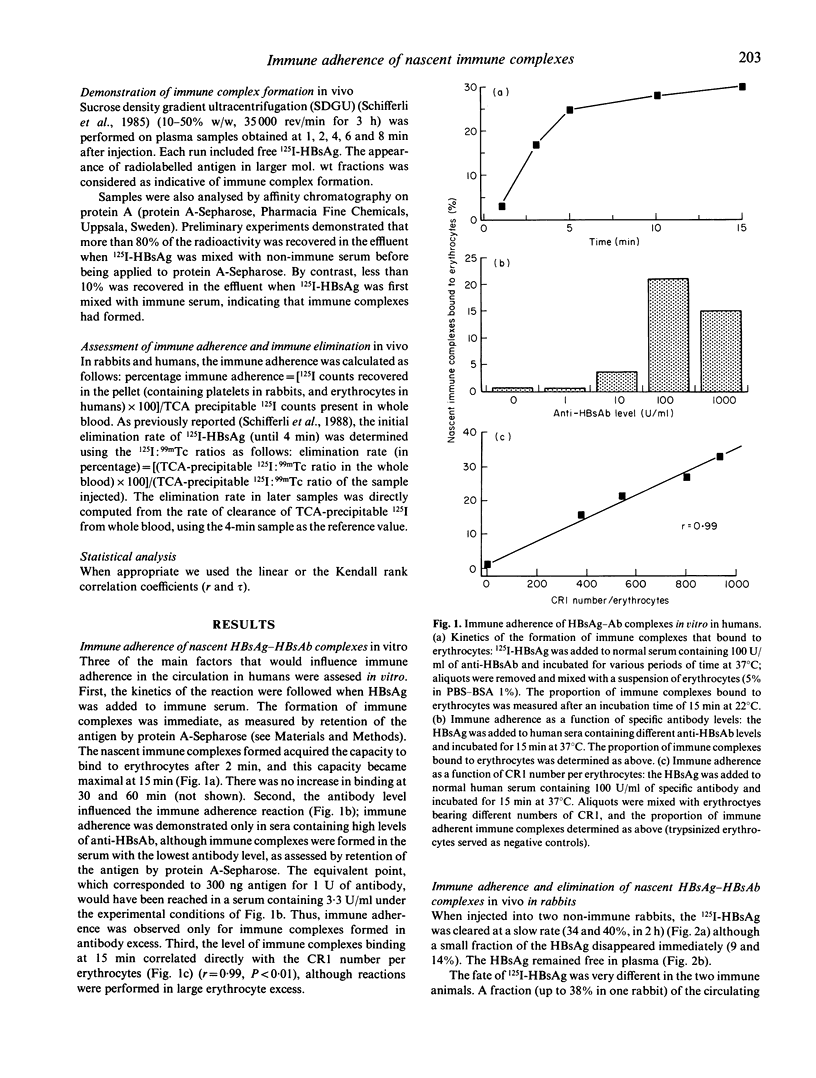
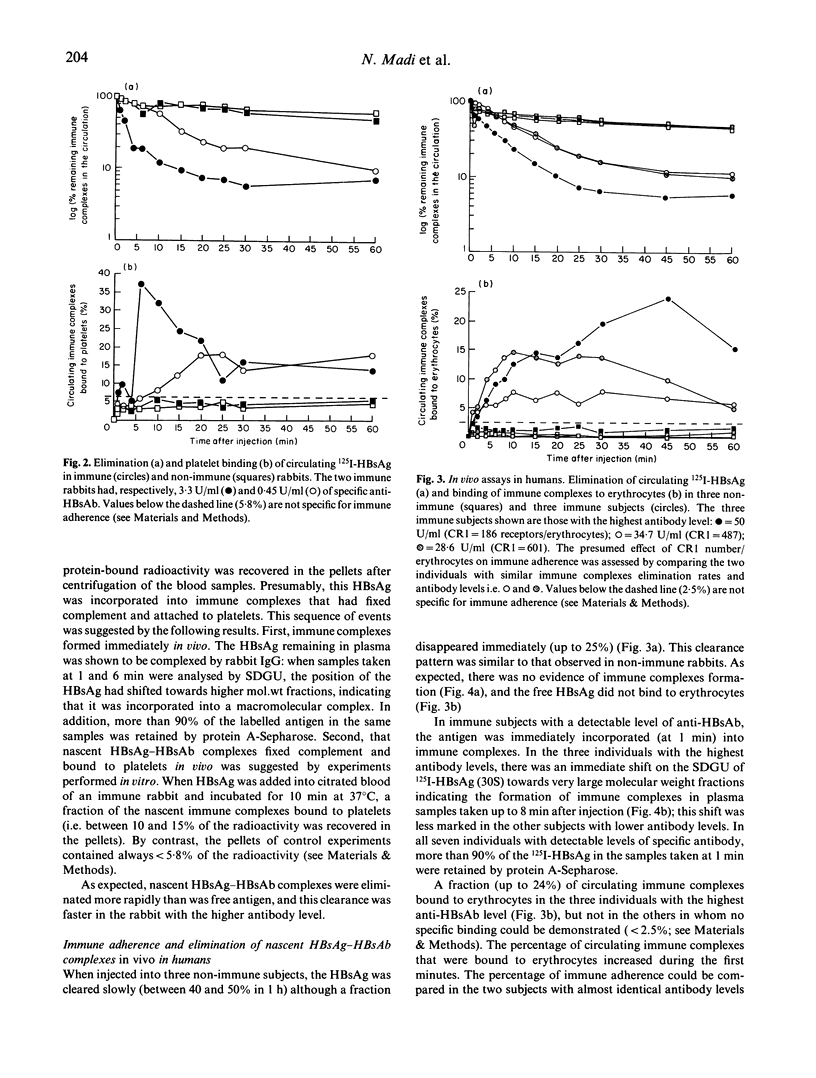
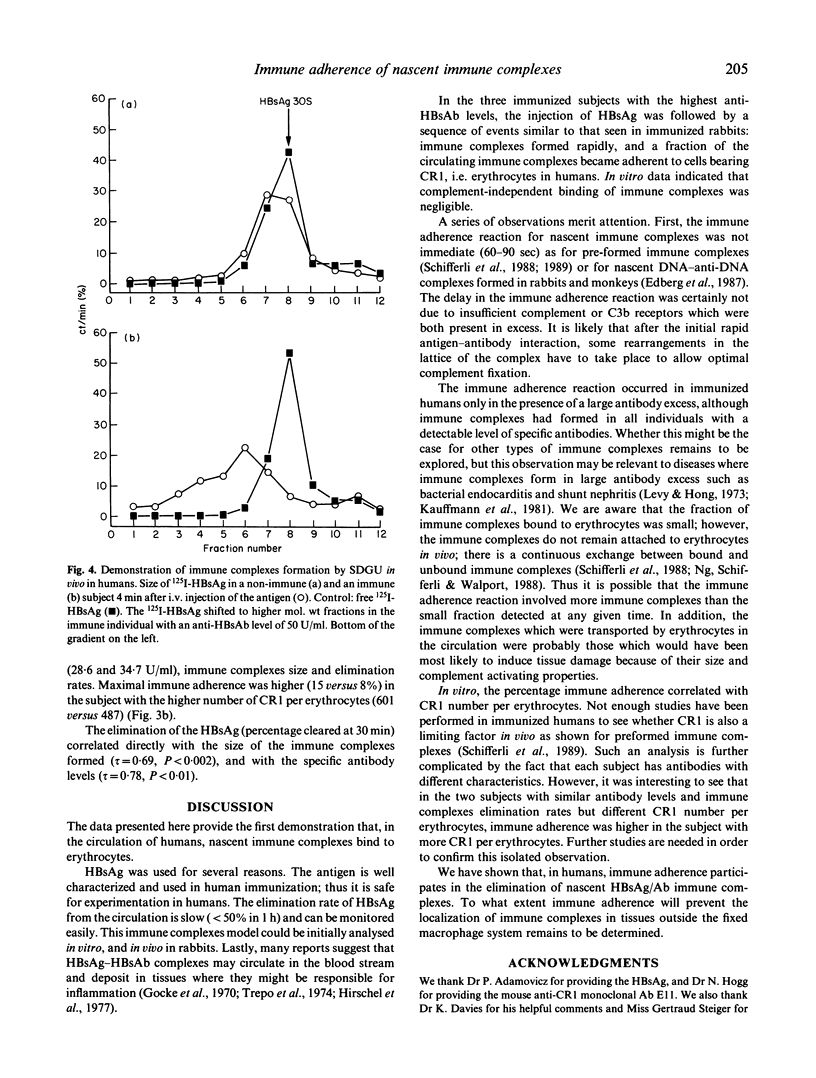
Upon i.v. injection into humans, pre-formed immune complexes bind complement and adhere to complement receptor type I (CR1, CD35) on erythrocytes (immune adherence). However, in most circumstances antigen and antibody react in the presence of complement; such nascent immune complexes may have properties different from pre-formed immune complexes. To define whether nascent immune complexes would also adhere to erythrocytes in vivo in humans, we studied immune complexes that formed upon i.v. injection of radiolabelled hepatitis B surface antigen (HBsAg) into immunized volunteers (eight subjects with anti-HBsAb levels ranging from undetectable to 50 U/ml.; and three control non-immune individuals). Immune complexes formed immediately in the subjects with detectable levels of specific antibody, and the clearance rate of these immune complexes correlated with the anti-HBsAb level (r = 0.78, P < 0.01). A fraction of the circulating immune complexes bound to erythrocytes in the three individuals with the highest antibody level (8-15% at 10 min). The effect of CR1 number per erythrocytes was analysed in two subjects with similar antibody levels and immune complexes clearance rates: immune adherence was higher in the subject with more CR1 per erythrocytes. The same immune complexes model studied in vitro provided similar results: a fraction of nascent immune complexes bound to human erythrocytes; this immune adherence was observed only when immune complexes formed in the presence of antibody excess, and correlated with CR1 number per erythrocytes (r = 0.99, P < 0.01). Finally, adherence of nascent HBsAg-antibody immune complexes to platelets was demonstrated in rabbits. Although immune adherence involves only a small fraction of nascent immune complexes at any given time, it may be essential for the safe disposal of large nascent immune complexes.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bolton A. E., Hunter W. M. The labelling of proteins to high specific radioactivities by conjugation to a 125I-containing acylating agent. Biochem J. 1973 Jul;133(3):529–539. doi: 10.1042/bj1330529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornacoff J. B., Hebert L. A., Smead W. L., VanAman M. E., Birmingham D. J., Waxman F. J. Primate erythrocyte-immune complex-clearing mechanism. J Clin Invest. 1983 Feb;71(2):236–247. doi: 10.1172/JCI110764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edberg J. C., Kujala G. A., Taylor R. P. Rapid immune adherence reactivity of nascent, soluble antibody/DNA immune complexes in the circulation. J Immunol. 1987 Aug 15;139(4):1240–1244. [PubMed] [Google Scholar]
- Fraker P. J., Speck J. C., Jr Protein and cell membrane iodinations with a sparingly soluble chloroamide, 1,3,4,6-tetrachloro-3a,6a-diphrenylglycoluril. Biochem Biophys Res Commun. 1978 Feb 28;80(4):849–857. doi: 10.1016/0006-291x(78)91322-0. [DOI] [PubMed] [Google Scholar]
- Gocke D. J., Hsu K., Morgan C., Bombardieri S., Lockshin M., Christian C. L. Association between polyarteritis and Australia antigen. Lancet. 1970 Dec 5;2(7684):1149–1153. doi: 10.1016/s0140-6736(70)90339-9. [DOI] [PubMed] [Google Scholar]
- Hirschel B. J., Benusiglio L. N., Favre H., Chatelanat F., Humair L., Zubler R. H., Cruchaud A. Glomerulonephritis associated with hepatitis B. report of a case and review of the literature. Clin Nephrol. 1977 Sep;8(3):404–409. [PubMed] [Google Scholar]
- Kauffmann R. H., Thompson J., Valentijn R. M., Daha M. R., Van Es L. A. The clinical implications and the pathogenetic significance of circulating immune complexes in infective endocarditis. Am J Med. 1981 Jul;71(1):17–25. doi: 10.1016/0002-9343(81)90253-9. [DOI] [PubMed] [Google Scholar]
- Levy R. L., Hong R. The immune nature of subacute bacterial endocarditis (SBE) nephritis. Am J Med. 1973 May;54(5):645–652. doi: 10.1016/0002-9343(73)90123-x. [DOI] [PubMed] [Google Scholar]
- Ng Y. C., Schifferli J. A., Walport M. J. Immune complexes and erythrocyte CR1 (complement receptor type 1): effect of CR1 numbers on binding and release reactions. Clin Exp Immunol. 1988 Mar;71(3):481–485. [PMC free article] [PubMed] [Google Scholar]
- Paccaud J. P., Steiger G., Sjöholm A. G., Spaeth P. J., Schifferli J. A. Tetanus toxoid-anti-tetanus toxoid complexes: a potential model to study the complement transport system for immune complex in humans. Clin Exp Immunol. 1987 Aug;69(2):468–476. [PMC free article] [PubMed] [Google Scholar]
- Ross G. D., Yount W. J., Walport M. J., Winfield J. B., Parker C. J., Fuller C. R., Taylor R. P., Myones B. L., Lachmann P. J. Disease-associated loss of erythrocyte complement receptors (CR1, C3b receptors) in patients with systemic lupus erythematosus and other diseases involving autoantibodies and/or complement activation. J Immunol. 1985 Sep;135(3):2005–2014. [PubMed] [Google Scholar]
- Schifferli J. A., Ng Y. C., Estreicher J., Walport M. J. The clearance of tetanus toxoid/anti-tetanus toxoid immune complexes from the circulation of humans. Complement- and erythrocyte complement receptor 1-dependent mechanisms. J Immunol. 1988 Feb 1;140(3):899–904. [PubMed] [Google Scholar]
- Schifferli J. A., Ng Y. C., Paccaud J. P., Walport M. J. The role of hypocomplementaemia and low erythrocyte complement receptor type 1 numbers in determining abnormal immune complex clearance in humans. Clin Exp Immunol. 1989 Mar;75(3):329–335. [PMC free article] [PubMed] [Google Scholar]
- Schifferli J. A., Peters D. K. Immune adherence and staphylococcus protein A binding of soluble immune complexes produced by complement activation. Clin Exp Immunol. 1983 Dec;54(3):827–833. [PMC free article] [PubMed] [Google Scholar]
- Schifferli J. A., Steiger G., Hauptmann G., Spaeth P. J., Sjöholm A. G. Formation of soluble immune complexes by complement in sera of patients with various hypocomplementemic states. Difference between inhibition of immune precipitation and solubilization. J Clin Invest. 1985 Dec;76(6):2127–2133. doi: 10.1172/JCI112217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trepo C. G., Zucherman A. J., Bird R. C., Prince A. M. The role of circulating hepatitis B antigen/antibody immune complexes in the pathogenesis of vascular and hepatic manifestations in polyarteritis nodosa. J Clin Pathol. 1974 Nov;27(11):863–868. doi: 10.1136/jcp.27.11.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga L., Thiry E., Füst G. BSA-anti-BSA immune complexes formed in the presence of human complement do not bind to autologous red blood cells. Immunology. 1988 Jul;64(3):381–384. [PMC free article] [PubMed] [Google Scholar]
- Waxman F. J., Hebert L. A., Cornacoff J. B., VanAman M. E., Smead W. L., Kraut E. H., Birmingham D. J., Taguiam J. M. Complement depletion accelerates the clearance of immune complexes from the circulation of primates. J Clin Invest. 1984 Oct;74(4):1329–1340. doi: 10.1172/JCI111543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waxman F. J., Hebert L. A., Cosio F. G., Smead W. L., VanAman M. E., Taguiam J. M., Birmingham D. J. Differential binding of immunoglobulin A and immunoglobulin G1 immune complexes to primate erythrocytes in vivo. Immunoglobulin A immune complexes bind less well to erythrocytes and are preferentially deposited in glomeruli. J Clin Invest. 1986 Jan;77(1):82–89. doi: 10.1172/JCI112306. [DOI] [PMC free article] [PubMed] [Google Scholar]


