Abstract
Background
Patients presenting in the emergency room with flank pain suggestive of acute ureteric colic may have alternative underlying conditions mimicking ureteric stones. An early diagnosis and appropriate treatment for other causes of flank pain is important. The majority of centers around the world are increasingly using un-enhanced helical CT (UHCT) for evaluation of ureteric colic. This study was conducted to determine the incidence and spectrum of significant incidental diagnoses established or suggested on UHCT performed for suspected renal/ureteric colic.
Methods
Urologist and radiologist reviewed 233 consecutive UHCT, performed for suspected renal/ureteral colic along with assessment of the medical records. Radiological diagnoses of clinical entities not suspected otherwise were analyzed. All other relevant radiological, biochemical and serological investigations and per-operative findings were also noted.
Results
Ureteral calculi were identified in 148 examinations (64%), findings of recent passage of calculi in 10 (4%) and no calculus in 75 examinations (32%). Overall the incidental findings (additional or alternative diagnosis) were found in 28 (12%) CT scans. Twenty (71%) of these diagnoses were confirmed by per-operative findings, biopsy, and other radiological and biochemical investigations or on clinical follow up.
Conclusion
A wide spectrum of significant incidental diagnoses can be identified on UHCT performed for suspected renal/ureteral colic. In the present series of 233 consecutive CT examinations, the incidence of incidental diagnosis was 12%.
Keywords: Non-contrast enhanced Spiral Computed Tomography, flank pain, incidental diagnosis
Background
The application of UHCT for the diagnosis of acute ureteric colic has positively influenced the practice of urology and uro-radiology. The technology allows the rapid and accurate determination of the presence of stone in the urinary tract. Since the pioneering study on the role of UHCT in the evaluation of ureteric colic by Smith et al [1] in 1995, a number of studies have shown the superiority of non-contrast enhanced CT over IVU and Ultrasonography [2-5]. Its sensitivity and specificity is reported to be more than 95% and 96 % respectively [1-6]. An important disadvantage is a higher radiation dose to the patient [7]. Denton [8] noted a difference of 2.5 mSv versus 4.7 mSv in the radiation dose to the patient between IVU and UHCT performed for renal colic.
Advantages of UHCT includes rapid scan time, avoidance of contrast related hazards, cost effectiveness, high accuracy, and its ability to suggest an alternative diagnosis for flank pain. This last characteristic of UHCT is valuable in diagnosing many significant diseases earlier in their course, which may be helpful in decreasing the associated morbidity. In this study, we are presenting our initial experience of diagnosing alternative or additional diseases on UHCT performed for the evaluation of acute flank pain.
Methods
The radiologist's reports on CT, CT films and medical records of 233 consecutive patients, performed between July 2000 and August 2001 at a University Hospital for suspected renal/ureteral colic were reviewed. The UHCT were obtained on a Cti/pro single slice helical CT scanner (General Electrical medical systems, Milwaukee, WI). The exposure factors setting were KVp 130 and mAS 200–250. All scans were obtained from the upper border of T12 vertebral body to the lower border of symphysis pubis using 5 mm collimation, without the use of oral or intravenous contrast material. Patients were placed in supine position with full urinary bladder at the time of the UHCT. Additional prone films were taken whenever the radiologist needed a better description of suspected distal ureteric calculi. Radiological diagnoses of clinical entities otherwise suspected were analyzed. All relevant radiological, biochemical, serological investigations as well as per-operative findings were also analyzed.
Results
From July 19, 2000 to August 15, 2001, 233 patients had UHCT for the evaluation of acute flank pain. Ureteral calculi were identified in 148 examinations (64%), findings of recent passage of calculi in 10 (4%) and no calculus in 75 (32%) scans. Thirty-two of the conservatively managed patients were lost to follow up and therefore were not included. In the remaining 201 patients, sensitivity and specificity of UHCT in diagnosing calculi was 99% and 98% respectively while +ve and -ve predictive value was 99% and 98% respectively. Twenty-eight patients (12%) had alternative or additional diseases (other than renal, ureteric or bladder stone disease) diagnosed on UHCT.
Table 1 describes in detail the alternative or additional diagnoses.
Table 1.
Alternative diagnoses to ureteric colic made by UHCT.
| Alternative or additional diagnosis | n = 28 | Confirmation of diagnosis | Modality used for confirmation |
| Inflammatory conditions | |||
| Cholelithiasis | 3 | 3 | Ultrasound |
| Pyelonephritis | 2 | 2 | Clinical picture/ microbiology |
| Appendicitis | 3 | 1 | Per-opearative findings/ pathology |
| Pancreatitis | 1 | 1 | Biochemical |
| Cholecystitis | 1 | 1 | Per-operative findings/ pathology |
| Mesenteric lymphadenitis | 1 | - | Clinical follow up |
| Spleenic abscess | 1 | 1 | Ultrasound |
| Tumors/Mass | |||
| Adenaxal mass | 4 | 2 | Ultrasound |
| Ovarian cyst | 2 | 1 | Ultrasound |
| Renal mass | 2 | 1 | Ultrasound |
| Incidentaloma | 1 | 1 | Ultrasound |
| Pelvic mass | 1 | 1 | Ultrasound |
| Vertebral metastasis | 1 | 1 | Histopathology |
| Pancreatic head cyst* | 1 | - | - |
| Other Urological disease | |||
| Uretero-pelvic junction obstruction | 2 | 2 | Reterograde urography/ diuretic renography |
| Ureteric stricture | 1 | 1 | Retrograde urography |
| Bladder outlet obstruction | 1 | 1 | Urodynamics |
*Patient lost to follow up
In 71 % of these cases, diagnosis was confirmed by the surgical procedure, biopsy and biochemical evaluation (in case of pancreatitis) as shown in Table 1.
Discussion
A wide variety of significant or potentially significant diagnoses can be identified on UHCT performed for suspected ureteral/renal colic [9-13]. Apart from its high sensitivity and specificity for diagnosing stone disease, the characteristic of UHCT, which discriminates it from other modalities, is its ability to pick up other unsuspected significant clinical entities. Early diagnosis of diseases such as appendicitis, cholecystitis, pancreatitis, diverticulitis and leaking aortic aneurysm that require urgent and prompt treatment could affect the associated morbidity and mortality associated with such diseases. In a large series of 1000 UHCT for suspected renal/ureteric colic, Katz[13] reported 101 patients (10%) with alternative or incidental diagnosis.
Table 2 shows some of the major series published to date on this subject.
Table 2.
Incidence of other conditions in previously published series
| Incidental Diseases | |||||
| Genitourinary (excluding renal, vesical and ureteric calculi) | Current series 28/233(12 %) | Fielding [9] 11/100 (10 %) | Marcella [10] 60/412 (14.5 %) | Andersson [12] 65/417 (15.9 %) | Katz [13] 101/1000 (10%) |
| Adenaxal masses | 4 | 4 | 11 | 13 | 23 |
| Ovarian cyst | 2 | - | 8 | - | - |
| Pyelonephritis | 2 | - | - | 7 | 9 |
| Bladder outlet obstruction | 1 | - | - | 3 | 4 |
| PUJ obstruction | 2 | - | - | 1 | 3 |
| Complicated renal cyst | - | - | - | - | 2 |
| Renal/perinephric hemorrhage | - | - | - | - | 2 |
| UVJ obstruction | - | - | - | - | 4 |
| Renal cell carcinoma/mass | 2 | - | 13 | 1 | 4 |
| Ureteric obstruction due to Lymph nodes | - | - | - | - | 1 |
| A-V malformation | - | - | - | - | 1 |
| Renal artery aneurysm | - | - | 1 | 1 | |
| Polycystic kidney disease | - | - | - | - | 1 |
| Duplicated ureter | - | - | - | 1 | 2 |
| Urachal mass | - | - | - | - | 1 |
| Ureteral stricture | 1 | - | 5 | - | - |
| Uterine leiomyma | - | - | - | 1 | - |
| Obstruction by TCC/cervical CA | - | - | - | 2 | - |
| Perinephric hematoma | - | - | - | 1 | - |
| Megaureter | - | - | - | 1 | - |
| Emphysematous cystitis | - | - | - | 1 | - |
| Large stone in neo-bladder | - | - | - | 1 | - |
| Xanthogranulomatous. Pyelonephritis | - | - | - | 1 | -- |
| Hematoma in bladder | - | - | - | 1 | -- |
| Lymphocele in transplanted kidney | - | - | - | 1 | -- |
| Non genitourinary tract diseases | |||||
| Colonic Pathology | - | - | - | - | 6 |
| Colonic Cancer | - | 1 | 4 | - | 2 |
| Appendicitis | 3 | - | 6 | 7 | 5 |
| Pelvic mass/lymphadenopathy | 1 | - | - | - | 6 |
| Small bowel disease | - | - | - | - | 4 |
| Porcelain gallbladder | - | - | - | - | 2 |
| Cholelithiasis | 3 | 2 | 7 | - | - |
| Cholecystitis | 1 | - | - | 1 | 3 |
| Choledocholithiasis | - | - | - | 4 | - |
| Pancreatitis | 1 | - | - | 2 | 3 |
| Hepatomegaly | - | - | - | - | 1 |
| Peri-umbilical Hernia | - | - | - | 1 | 1 |
| Liposarcoma | - | - | - | 1 | 1 |
| Cervical mass | - | - | - | 1 | |
| Vaginal mass | - | - | - | - | 1 |
| Small bowel intussusceptions | - | - | - | - | 1 |
| CLL/Lymphoma | - | - | - | 1 | 1 |
| Crohn's disease | - | - | - | 2 | 1 |
| Psoa's hemorrhage | - | - | - | - | 1 |
| Rectus sheath hematoma | - | - | - | - | 1 |
| Sacroilitis | - | - | - | - | 1 |
| Bronchopneumonia | - | 1 | - | - | - |
| Diverticulitis | - | 3 | 4 | 5 | - |
| Leaking aortic aneurysm | - | - | 1 | 1 | - |
| Aortic dissection | - | - | - | - | 1 |
| Mesenteric lymphadenitis | 1 | - | - | - | - |
| Spleenic infarct | - | - | 1 | - | - |
| Spleenic abscess | 1 | - | - | - | - |
| Ruptured spleen | - | - | - | 1 | - |
| Vertebral metastasis | 1 | - | - | 1 | - |
| Adrenal adenoma | 1 | - | - | - | - |
| Pancreatic head cystic mass | 1 | - | - | - | - |
| Liver haemangioma | - | - | - | 1 | - |
Among the major series published on the subject [9-13], the incidence of unsuspected clinical entities was 10–15%. The disease pattern is remarkably similar in most series (Table 2). In one report from Albert Einstein Medical Center, Philadelphia, Marcella et al [8] noted an unusually high incidence of incidentally discovered renal cell cancer. There is low incidence of diverticulitis in South Asia and we have found no case of diverticulitis in our series by comparison to other series. It is important that in the absence of ureterolithiasis, particular care should be taken to rule out alternative diagnosis for flank pain.
In our series, early diagnosis of pancreatitis, cholecystitis, mesenteric lymphadenitis, pyelonephritis and appendicitis, initiated early treatment. The alternative diagnosis of eight tumors in our series and similar trends in other series is interesting. It suggests that UHCT may change the prognosis in many cases that would otherwise be diagnosed late.
Conclusion
A wide variety of significant alternative or additional diagnoses can be reliably identified on UHCT performed for suspected renal/ureteric colic. In the present series, such diseases were diagnosed in 12% of cases. Unlike most series from the West we did not note any case of diverticulitis.
Competing interests
None declared.
Authors' contribution
NAA collected data and participated in manuscript writing
MHA conceived the idea, helped in the analysis of data and participated in writing the manuscript.
JR conceived the idea, helped in the analysis of data and participated in writing the manuscript.
All authors read and approved the final manuscript.
Figure 1.
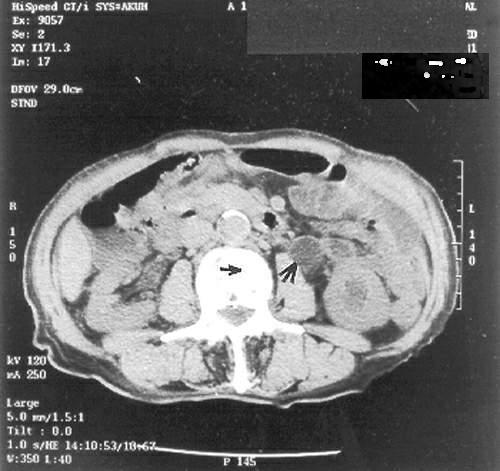
A 70 year gentleman presented with a three month localized left flank pain. It was mild to moderate in intensity. UHCT showed (Fig. 1) gross hydronephrosis and hydroureter with 1 cm mid-ureteric calculus (Rt. Arrow). Incidentally, hyper-dense bony deposits were detected in the L3 vertebral body (Lt. arrow). Later, a raised PSA and histopathology of prostate biopsy confirmed adenocarcinoma.
Figure 2.
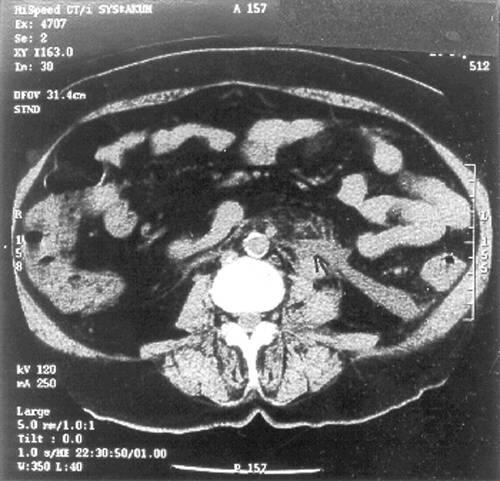
A 40-year old lady presented to the emergency room with a 12-hour history of severe left flank pain radiating downwards and backwards. She was tender in the left flank and hypochondrium. Her urine examination showed microscopic hematuria. An initial diagnosis of left ureteric colic was made. However, UHCT showed an inflamed pancreatic tail (Arrow). A raised amylase and lipase confirmed the diagnosis of acute pancreatitis.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Nazim A Ahmad, Email: nazim.ahmed@aku.edu.
M Hammad Ather, Email: hammad.ather@aku.edu.
Jeffrey Rees, Email: jeffrey.rees@aku.edu.
References
- Smith RC, Rosenfield AT, Choe KA, et al. Acute flank pain: Comparison of non-contrast enhanced computerized tomography and intravenous pyelography. Radiology. 1995;194:789–94. doi: 10.1148/radiology.194.3.7862980. [DOI] [PubMed] [Google Scholar]
- Spencer BA, Bush JA, Rao PM, Dretler SP, Rhea JT, Novelline RA. Unenhanced helical CT for clinically suspected acutely symptomatic ureteral calculi: Experience with 339 examinations. Presented at American Roentgen Ray Society 98th Annual Meeting. San Francisco. 1998.
- Yilmeaz S, Sindel T, Arsalan G, et al. Comparison of spiral CT, US and IVU in detection of ureteral calculi. Eur Radiol. 1998;8:212–217. doi: 10.1007/s003300050364. [DOI] [PubMed] [Google Scholar]
- Niall O, Russell J, MacGregor , et al. A comparison of noncontrast computerized tomography with excretory urography in the assessment of acute flank pain. J Urol. 1999;161:534–7. doi: 10.1097/00005392-199902000-00047. [DOI] [PubMed] [Google Scholar]
- Homer JA, Davies-Payne DL, P Peddinti BS. Randomized prospective comparison of non-contrast enhanced helical computed tomography and intravenous urography in the diagnosis of acute ureteric colic. Australas Radiol. 2001;45:285–90. doi: 10.1046/j.1440-1673.2001.00922.x. [DOI] [PubMed] [Google Scholar]
- Spencer BA, Dretler PS. Helical CT and ureteric colic. Urol Clin North Amer. 2000;27:231–41. doi: 10.1016/s0094-0143(05)70253-6. [DOI] [PubMed] [Google Scholar]
- Schulz RJ, Gignac C. Applications of tissue air ratios for patient dosage in diagnostic radiology. Radiology. 1976;120:687. doi: 10.1148/120.3.687. [DOI] [PubMed] [Google Scholar]
- Denton ER, Mackenzie A, Greenwell T, Popert R, Rankin SC. Unenhanced helical CT for renal colic- is the radiation dose justifiable. Clin Radiol. 1999;54:444–7. doi: 10.1016/s0009-9260(99)90829-2. [DOI] [PubMed] [Google Scholar]
- Fielding JR, Steel G, Fox LA, et al. Spiral computerized tomography in the evaluation of acute flank pain: A replacement for excretory urography. J Urol. 1997;157:2071–2073. doi: 10.1097/00005392-199706000-00009. [DOI] [PubMed] [Google Scholar]
- Marcella MN, Harkaway RC, Susan L, et al. Helical CT Scanning: The primary imaging modality for acute flank pain: Am. J Emerg Med. 2000;18:649–52. doi: 10.1053/ajem.2000.16292. [DOI] [PubMed] [Google Scholar]
- Dalrymple NC, Verga M, Kevin R, et al. The value of unenhanced helical CT in the management of acute flank. Pain J Urol. 1998;159:735–40. [PubMed] [Google Scholar]
- Anderson KR, Smith RC. CT for the evaluation of flank pain. J Endourol. 2001;15:25–29. doi: 10.1089/08927790150500917. [DOI] [PubMed] [Google Scholar]
- Katz DS, Scheer M, Jefrey H, et al. Alternative or additional diagnosis on unenhanced helical computed tomography for suspected renal colic: Experience with 1000 consecutive examinations. Urology. 2000;56:53–57. doi: 10.1016/S0090-4295(00)00584-7. [DOI] [PubMed] [Google Scholar]


