Abstract
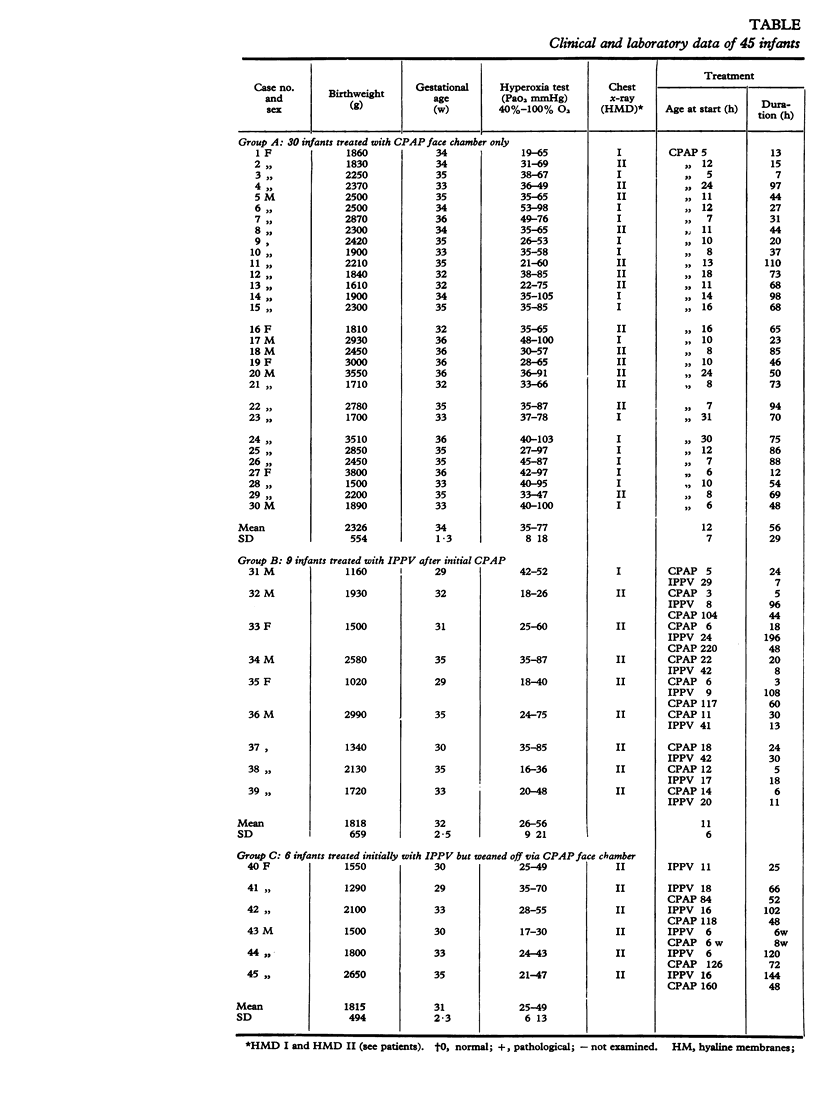
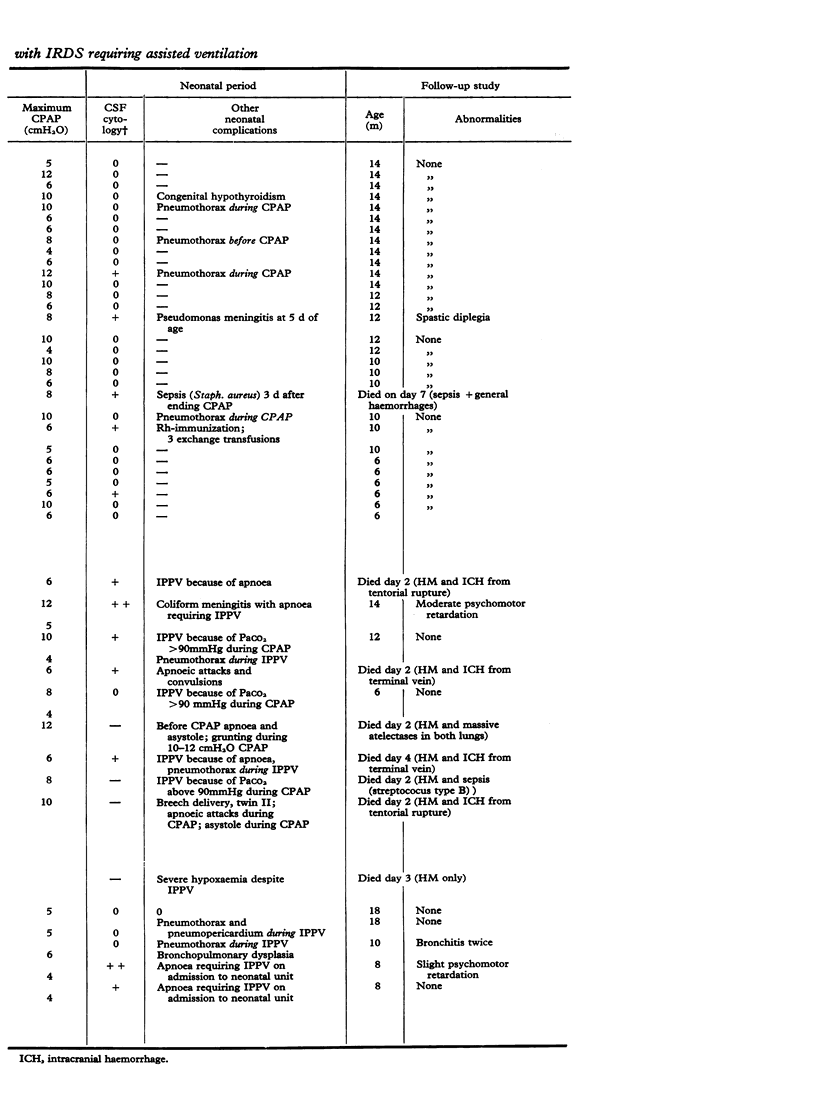
Continuous positive airways pressure treatment by a face chamber in idiopathic respiratory distress syndrome. During a 3-year period 45 infants with idiopathic respiratory distress syndrome (IRDS) requiring ventilatory support were treated in the neonatal unit. Continuous positive airways pressure (CPAP) via the face chamber was applied as initial therapy in 39 infants and during weaning from initial intermittent positive pressure ventilation (IPPV) treatment in 5 infants, whereas 1 infant received IPPV only. Among the 39 infants initially treated with CPAP 9 required IPPV as well. The overall survival rate was 37/45 or 82%. Incapacity to hyperoxygenate while breathing 100% oxygen was the indication for CPAP while occurrence of apnoeic attacks was the indication for IPPV. Pao2 during the hyperoxia test before ventilatory support was less than 50 mmHg in 10 infants and between 50 and 105 mmHg in 35 infants. Surviving infants were followed up with neurological and developmental control examinations as well as chest x-ray, and in several infants pulmonary function tests. 3/37 infants had moderate neurological sequelae and only 1/37 infants developed bronchopulmonary dysplasia. No deleterious effects of the face chamber were seen. As the face chamber is a noninvasive and easily applied technique for CPAP therapy without hazards, it is proposed that it should be used at a still earlier stage of IRDS in order to lesson the need for IPPV treatment and to increase the neurological and lung functional quality of survival.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ackerman B. D., Stein M. P., Sommer J. S., Schumacher M. Continuous positive airway pressure applied by means of a tight-fitting face-mask. J Pediatr. 1974 Sep;85(3):408–411. doi: 10.1016/s0022-3476(74)80131-9. [DOI] [PubMed] [Google Scholar]
- Ahlström H., Jonson B. Pulmonary mechanics in infants. Methodological aspects. Scand J Respir Dis. 1974;55(2):129–140. [PubMed] [Google Scholar]
- Ahlström H. Pulmonary mechanics in infants surviving severe neonatal respiratory insufficiency. Acta Paediatr Scand. 1975 Jan;64(1):69–80. doi: 10.1111/j.1651-2227.1975.tb04381.x. [DOI] [PubMed] [Google Scholar]
- Ahlstöm H., Jonson B., Svenningsen N. W. Continuous positive airway pressure with a face chamber in early treatment of idiopathic respiratory distress syndrome. Acta Paediatr Scand. 1973 Jul;62(4):433–436. doi: 10.1111/j.1651-2227.1973.tb08132.x. [DOI] [PubMed] [Google Scholar]
- Angell James J. E., Daly M. de B. Nasal reflexes. Proc R Soc Med. 1969 Dec 12;62(12):1287–1293. [PMC free article] [PubMed] [Google Scholar]
- Ballard R. A., Kraybill E. N., Hernandez J., Renfield M. L., Blankenship W. J. Idiopathic respiratory distress syndrome. Treatment with continuous negative-pressure ventilation. Am J Dis Child. 1973 May;125(5):676–681. doi: 10.1001/archpedi.1973.04160050030006. [DOI] [PubMed] [Google Scholar]
- Barrie H. Letter: Continuous positive airway pressure for respiratory-distress syndrome. Lancet. 1973 Oct 13;2(7833):851–851. doi: 10.1016/s0140-6736(73)90898-2. [DOI] [PubMed] [Google Scholar]
- Baum J. D., Roberton N. R. Distending pressure in infants with respiratory distress syndrome. Arch Dis Child. 1974 Oct;49(10):771–781. doi: 10.1136/adc.49.10.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caliumi-Pellegrini G., Agostino R., Orzalesi M., Nodari S., Marzetti G., Savignoni P. G., Bucci G. Twin nasal cannula for administration of continuous positive airway pressure to newborn infants. Arch Dis Child. 1974 Mar;49(3):228–230. doi: 10.1136/adc.49.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chernick V. Continuous distending pressure in hyaline membrane disease: of devices, disadvantages, and a daring study. Pediatrics. 1973 Jul;52(1):114–115. [PubMed] [Google Scholar]
- Chernick V. Hyaline-membrane disease: therapy with constant lung-distending pressure. N Engl J Med. 1973 Aug 9;289(6):302–304. doi: 10.1056/NEJM197308092890606. [DOI] [PubMed] [Google Scholar]
- Chernick V., Vidyasagar D. Continuous negative chest wall pressure in hyaline membrane disease: one year experience. Pediatrics. 1972 May;49(5):753–760. [PubMed] [Google Scholar]
- Cooke R. Practical problems associated with artificial ventilation in the newborn infant. Biol Neonate. 1970;16(1):60–73. doi: 10.1159/000240257. [DOI] [PubMed] [Google Scholar]
- Dinwiddie R., Mellor D. H., Donaldson H. C., Tunstall M. E., Russell G. Quality of survival after artificial ventilation of the newborn. Arch Dis Child. 1974 Sep;49(9):703–710. doi: 10.1136/adc.49.9.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn P. M. Respiratory distress syndrome. Continuous positive airway pressure (CPAP) using the Gregory box. Proc R Soc Med. 1974 Apr;67(4):245–247. [PMC free article] [PubMed] [Google Scholar]
- Fanaroff A. A., Cha C. C., Sosa R., Crumrine R. S., Klaus M. H. Controlled trial of continuous negative external pressure in the treatment of severe respiratory distress syndrome. J Pediatr. 1973 Jun;82(6):921–928. doi: 10.1016/s0022-3476(73)80418-4. [DOI] [PubMed] [Google Scholar]
- Gregory G. A., Kitterman J. A., Phibbs R. H., Tooley W. H., Hamilton W. K. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971 Jun 17;284(24):1333–1340. doi: 10.1056/NEJM197106172842401. [DOI] [PubMed] [Google Scholar]
- Jung A. L., Thomas G. K. Stricture of the nasal vestibule: a complication of nasotracheal intubation in newborn infants. J Pediatr. 1974 Sep;85(3):412–414. doi: 10.1016/s0022-3476(74)80132-0. [DOI] [PubMed] [Google Scholar]
- Kattwinkel J., Fleming D., Cha C. C., Fanaroff A. A., Klaus M. H. A device for administration of continuous positive airway pressure by the nasal route. Pediatrics. 1973 Jul;52(1):131–134. [PubMed] [Google Scholar]
- Omer M. I., Robson E., Neligan G. A. Can initial resuscitation of preterm babies reduce the death rate from hyaline membrane disease? Arch Dis Child. 1974 Mar;49(3):219–221. doi: 10.1136/adc.49.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prod'hom L. S., Choffat J. M., Frenck N., Mazoumi M., Relier J. P., Torrado A. Care of the seriously ill neonate with hyaline membrane disease and with sepsis (sclerema neonatorum). Pediatrics. 1974 Feb;53(2):170–181. [PubMed] [Google Scholar]
- Rasche R. F., Kuhns L. R. Histopathologic changes in airway mucosa of infants after endotracheal intubation. Pediatrics. 1972 Oct;50(4):632–637. [PubMed] [Google Scholar]
- Reynolds E. O., Taghizadeh A. Improved prognosis of infants mechanically ventilated for hyaline membrane disease. Arch Dis Child. 1974 Jul;49(7):505–515. doi: 10.1136/adc.49.7.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes P. G., Hall R. T. Continuous positive airway pressure delivered by face mask in infants with the idiopathic respiratory distress syndrome: a controlled study. Pediatrics. 1973 Jul;52(1):1–5. [PubMed] [Google Scholar]
- Salle B., Champin J. P., Desebbe C., Andre M. Le traitement des formes sévères de détresse respiratoire idiopathique du nouveau-né par l'utilisation d'une pression négative constante périthoracique. Arch Fr Pediatr. 1974 Jun-Jul;31(6):565–573. [PubMed] [Google Scholar]
- Svenningsen N. W., Blennow G. Continuous positive airway pressure and noise level. Lancet. 1973 Sep 15;2(7829):623–623. doi: 10.1016/s0140-6736(73)92460-4. [DOI] [PubMed] [Google Scholar]
- Vert P., Andre M., Sibout M. Continuous positive airway pressure and hydrocephalus. Lancet. 1973 Aug 11;2(7824):319–319. doi: 10.1016/s0140-6736(73)90816-7. [DOI] [PubMed] [Google Scholar]