Abstract
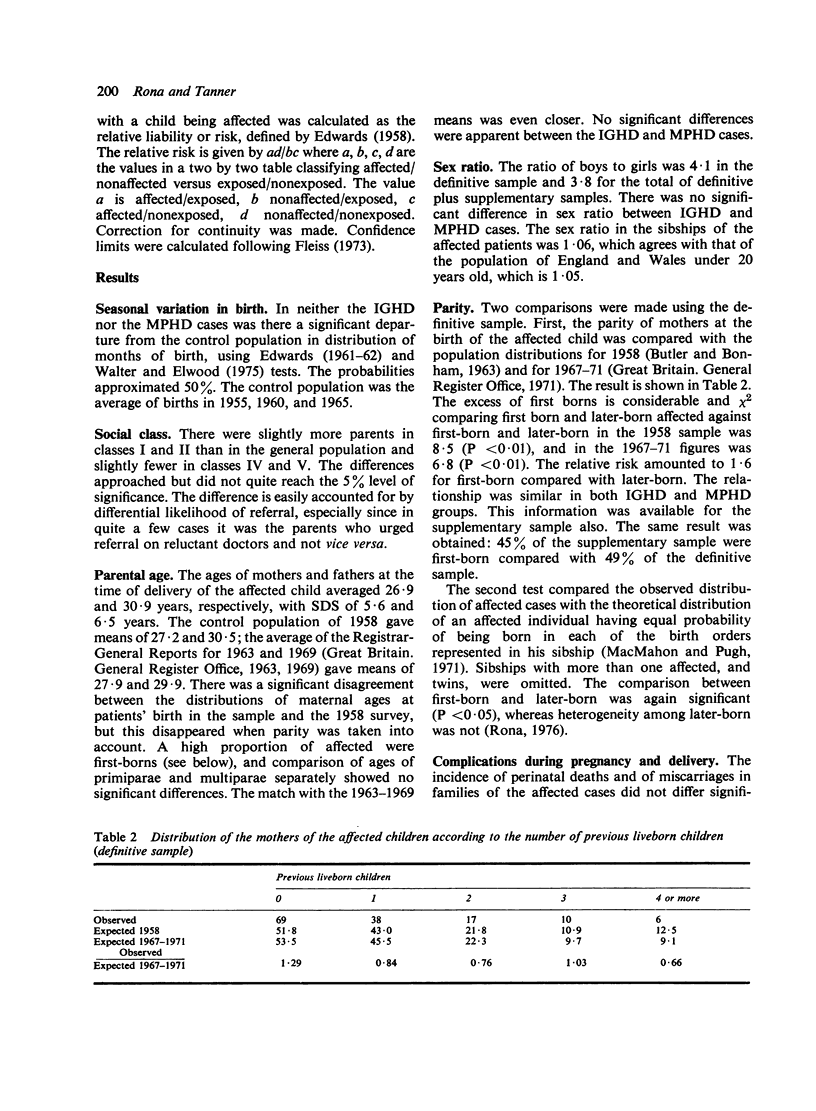
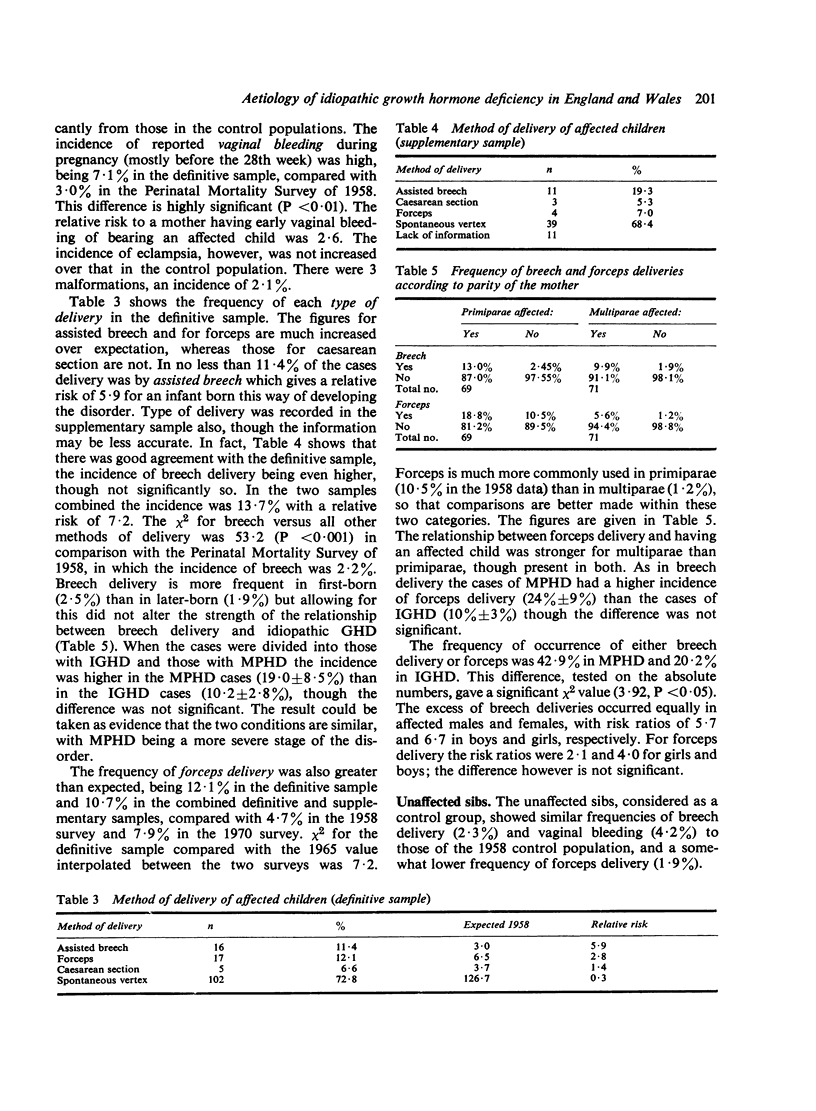
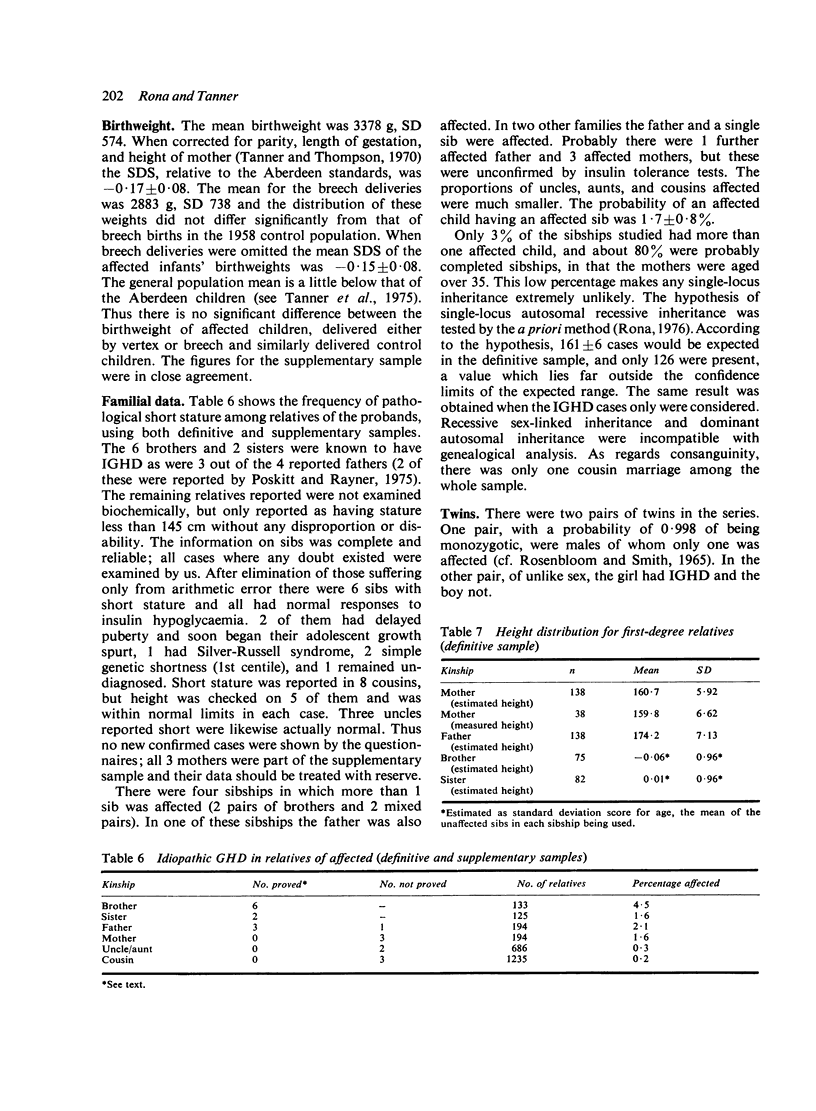
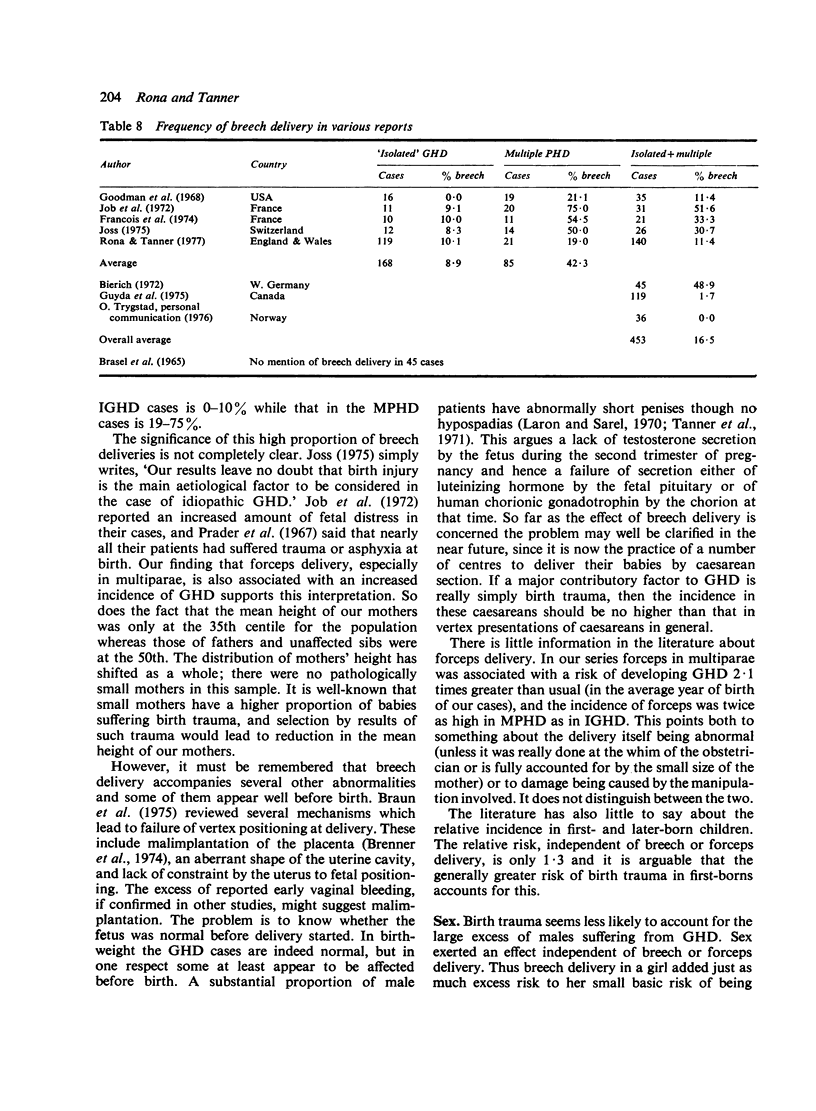
Information on height, sex, age, and condition of mothers' pregnancy and labour was obtained on all first- and second-degree relatives of 140 cases of idiopathic growth hormone deficiency (GHD). Less detailed information was available for 68 further cases, the two samples together constituting all cases from England and Wales treated under the Medical Research Council Clinical Trial of Human Growth Hormone up till 1974. Compared with the Perinatal Mortality survey of 1958, idiopathic GHD cases showed a significantly greater incidence of breech births (13-7%), of forceps deliveries especially in multiparae (5-6%), and of reported early vaginal bleeding (7-1%). The incidences of breech and forceps were both higher in cases with multiple pituitary hormone deficiency than in cases of 'isolated' GHD. The frequency of either breech or forceps was 43% in multiple and 20% in 'isolated' GHD. Heights of fathers and sibs of affected cases averaged the 50th centile; those of mothers the 35th centile. The ratio of boys to girls affected was 3-8. There were 4 families with more than one member affected; 4-5% of the brothers of probands were themselves affected, 2% of fathers and 1-5% of both sisters and mothers. In the world literature the sex ratio averages about 2-9 with little difference between series; the frequency of breech delivery averages 21% with large differences (2% to 50%) between series. A table of relative risks is given from which a screening procedure may be constructed; following 1% of selected births would give 10% of cases, and 20% of births 50% of cases. We propose a multifactorial aetiology for GHD which brings it into line with malformations such as anencephaly, cleft lip and palate, and pyloric stenosis. An underlying liability to the disease is postulated, continuously distributed in the population and depending on both polygenic and environmental factors among which sex and birth trauma are important. The disease becomes manifest when the liability value reaches a fixed threshold. On this assumption, heritability of idopathic GHD is approximately the same as that of coeliac disease, pyloric stenosis, and patent ductus.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BRASEL J. A., WRIGHT J. C., WILKINS L., BLIZZARD R. M. AN EVALUATION OF SEVENTY-FIVE PATIENTS WITH HYPOPITUITARISM BEGINNING IN CHILDHOOD. Am J Med. 1965 Apr;38:484–498. doi: 10.1016/0002-9343(65)90127-0. [DOI] [PubMed] [Google Scholar]
- Braun F. H., Jones K. L., Smith D. W. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419–421. doi: 10.1016/s0022-3476(75)80977-2. [DOI] [PubMed] [Google Scholar]
- Brenner W. E., Bruce R. D., Hendricks C. H. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700–712. doi: 10.1016/s0002-9378(16)33744-9. [DOI] [PubMed] [Google Scholar]
- Butenandt O., Knorr D. Familiärer Hypopituitarismus. Monatsschr Kinderheilkd. 1970 Aug;118(8):470–473. [PubMed] [Google Scholar]
- Carter C. O. Genetics of common single malformations. Br Med Bull. 1976 Jan;32(1):21–26. doi: 10.1093/oxfordjournals.bmb.a071318. [DOI] [PubMed] [Google Scholar]
- EDWARDS J. H. Congenital malformations of the central nervous system in Scotland. Br J Prev Soc Med. 1958 Jul;12(3):115–130. doi: 10.1136/jech.12.3.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EDWARDS J. H. The recognition and estimation of cyclic trends. Ann Hum Genet. 1961 May;25:83–87. doi: 10.1111/j.1469-1809.1961.tb01501.x. [DOI] [PubMed] [Google Scholar]
- Edwards J. H. Familial predisposition in man. Br Med Bull. 1969 Jan;25(1):58–64. doi: 10.1093/oxfordjournals.bmb.a070672. [DOI] [PubMed] [Google Scholar]
- François R., David L., Clerget-Gurnaud Traitement des nanismes hypophysaires. Pediatrie. 1974 Apr-May;29(3):305–318. [PubMed] [Google Scholar]
- Goodman H. G., Grumbach M. M., Kaplan S. L. Growth and growth hormone. II. A comparison of isolated growth-hormone deficiency and multiple pituitary-hormone deficiencies in 35 patients with idiopathic hypopituitary dwarfism. N Engl J Med. 1968 Jan 11;278(2):57–68. doi: 10.1056/NEJM196801112780201. [DOI] [PubMed] [Google Scholar]
- Guyda H., Friesen H., Bailey J. D., Leboeuf G., Beck J. C. Medical Research Council of Canada therapeutic trial of human growth hormone: first 5 years of therapy. Can Med Assoc J. 1975 Jun 7;112(11):1301–1309. [PMC free article] [PubMed] [Google Scholar]
- Hubble D. Growth hormone deficiencies in childhood. Can Med Assoc J. 1967 Nov 4;97(19):1144–1158. [PMC free article] [PubMed] [Google Scholar]
- Job J. C., Lejeune C., Canlorbe P., Rossier A. Le nanisme par insuffisance hypophysaire sporadique et idiopathique. Etude d'une série de 31 cas. Arch Fr Pediatr. 1972 Feb;29(2):117–133. [PubMed] [Google Scholar]
- Kumahara Y., Okada Y., Miyai K., Iwatsubo H. Typical cases of isolated growth hormone deficiency with autosomal recessive inheritance. Acta Endocrinol (Copenh) 1970 Apr;63(4):618–624. doi: 10.1530/acta.0.0630618. [DOI] [PubMed] [Google Scholar]
- Laron Z., Sarel R. Penis and testicular size in patients with growth hormone insufficency. Acta Endocrinol (Copenh) 1970 Apr;63(4):625–633. doi: 10.1530/acta.0.0630625. [DOI] [PubMed] [Google Scholar]
- McKusick V. A., Rimoin D. L. General Tom Thumb and other midgets. Sci Am. 1967 Jul;217(1):102–passim. doi: 10.1038/scientificamerican0767-102. [DOI] [PubMed] [Google Scholar]
- Moe P. J. Hypopituitary dwarfism. The importance of early therapy. Acta Paediatr Scand. 1968 Jul;57(4):300–304. doi: 10.1111/j.1651-2227.1968.tb07297.x. [DOI] [PubMed] [Google Scholar]
- Poskitt E. M., Rayner P. H. Isolated growth hormone deficiency. Two families with autosomal dominant inheritance. Arch Dis Child. 1974 Jan;49(1):55–59. doi: 10.1136/adc.49.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prader A., Zachmann M., Poley J. R., Illig R., Széky J. Long-term treatment with human growth hormone (Raben) in small doses. Evaluation of 18 hypopituitary patients. Helv Paediatr Acta. 1967 Oct;22(5):423–440. [PubMed] [Google Scholar]
- ROSENBLOOM A. L., SMITH D. W. IDIOPATHIC ANTERIOR HYPOPITUITARISM IN ONE OF IDENTICAL TWINS. J Pediatr. 1965 Jul;67:84–88. doi: 10.1016/s0022-3476(65)80307-9. [DOI] [PubMed] [Google Scholar]
- Rimoin D. L., Merimee T. J., Mc Kusick V. A. Growth-hormone deficiency in man: an isolated, recessively inherited defect. Science. 1966 Jun 17;152(3729):1635–1637. doi: 10.1126/science.152.3729.1635. [DOI] [PubMed] [Google Scholar]
- Sadeghi-Nejad A., Senior B. Autosomal dominant transmission of isolated growth hormone deficiency in iris-dental dysplasia (Rieger's syndrome). J Pediatr. 1974 Nov;85(5):644–648. doi: 10.1016/s0022-3476(74)80507-x. [DOI] [PubMed] [Google Scholar]
- Seip M., Van Der Hagen C. B., Trygstad O. Hereditary pituitary dwarfism with spontaneous puberty. Arch Dis Child. 1968 Feb;43(227):47–52. doi: 10.1136/adc.43.227.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikholislam B. M., Stempfel R. S., Jr Hereditary isolated somatotropin deficiency: effects of human growth hormone administration. Pediatrics. 1972 Mar;49(3):362–374. [PubMed] [Google Scholar]
- TRYGSTAD O., SEIP M. HEREDITARY PITUITARY DWARFISM TREATED WITH HUMAN GROWTH HORMONE. Acta Paediatr. 1964 Nov;53:527–532. doi: 10.1111/j.1651-2227.1964.tb07264.x. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Lejarraga H., Cameron N. The natural history of the Silver-Russell syndrome: a longitudinal study of thirty-nine cases. Pediatr Res. 1975 Aug;9(8):611–623. doi: 10.1203/00006450-197508000-00001. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Thomson A. M. Standards for birthweight as gestation periods from 32 to 42 weeks, allowing for maternal height and weight. Arch Dis Child. 1970 Aug;45(242):566–569. doi: 10.1136/adc.45.242.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H. A note on the bone age at which patients with true isolated growth hormone deficiency enter puberty. J Clin Endocrinol Metab. 1975 Oct;41(4):788–790. doi: 10.1210/jcem-41-4-788. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H., Hughes P. C., Vince F. P. Effect of human growth hormone treatment for 1 to 7 years on growth of 100 children, with growth hormone deficiency, low birthweight, inherited smallness, Turner's syndrome, and other complaints. Arch Dis Child. 1971 Dec;46(250):745–782. doi: 10.1136/adc.46.250.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H., Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. I. Arch Dis Child. 1966 Oct;41(219):454–471. doi: 10.1136/adc.41.219.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter S. D., Elwood J. M. A test for seasonality of events with a variable population at risk. Br J Prev Soc Med. 1975 Mar;29(1):18–21. doi: 10.1136/jech.29.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]


