Abstract
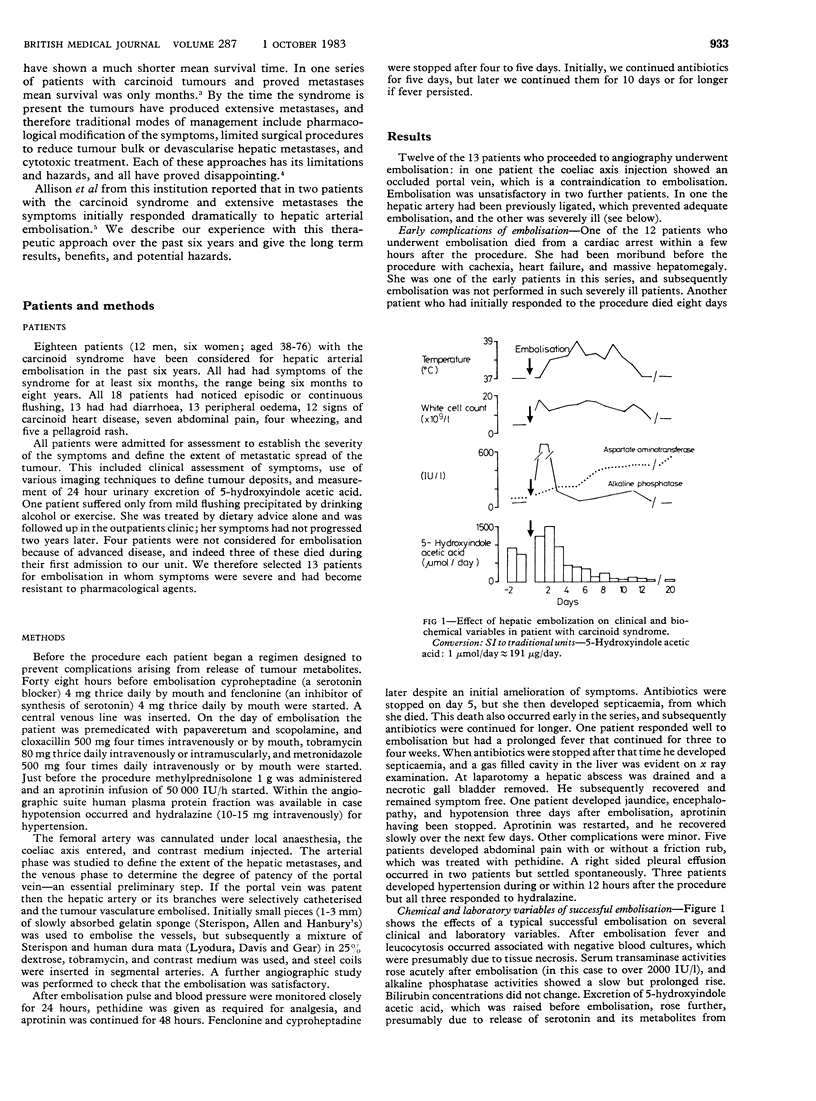
Eighteen patients with severe symptoms of the carcinoid syndrome were assessed for hepatic embolisation. Four were too ill, and one had mild symptoms; thus 13 received a periembolisation regimen of cyproheptadine, fenclonine, aprotinin, methylprednisolone, tobramycin, flucloxacillin, and metronidazole. Embolisation was not performed in one patient with an occluded portal vein and was unsatisfactory in two others, in one because she was moribund and in the other because the hepatic artery had been ligated. Dramatic improvement in symptoms occurred in the nine patients in whom embolisation was successfully carried out, with abolition of flushing, severe abdominal pain, and wheeze and reduction in diarrhoea from 10.5 (SD 7.6) to 1.6 (0.9) stools/day. Urinary excretion of 5-hydroxyindole acetic acid fell from 1048 (716) to 289 (184) mumol/24 h (200 (137) to 55 (35) mg/24 h). Complications included one death from septicaemia, a hepatic abscess requiring surgical drainage, abdominal pain in three patients, pleural effusion in two, and transient encephalopathy in one. Relief of symptoms lasted for one to 24 months, and second embolisation in two patients produced further remissions of four to six months. Five patients died, one to 40 months after embolisation, in four cases because of metastases or heart failure. Hepatic embolisation is the treatment of choice for symptoms of the carcinoid syndrome resistant to medical treatment.
Full text
PDF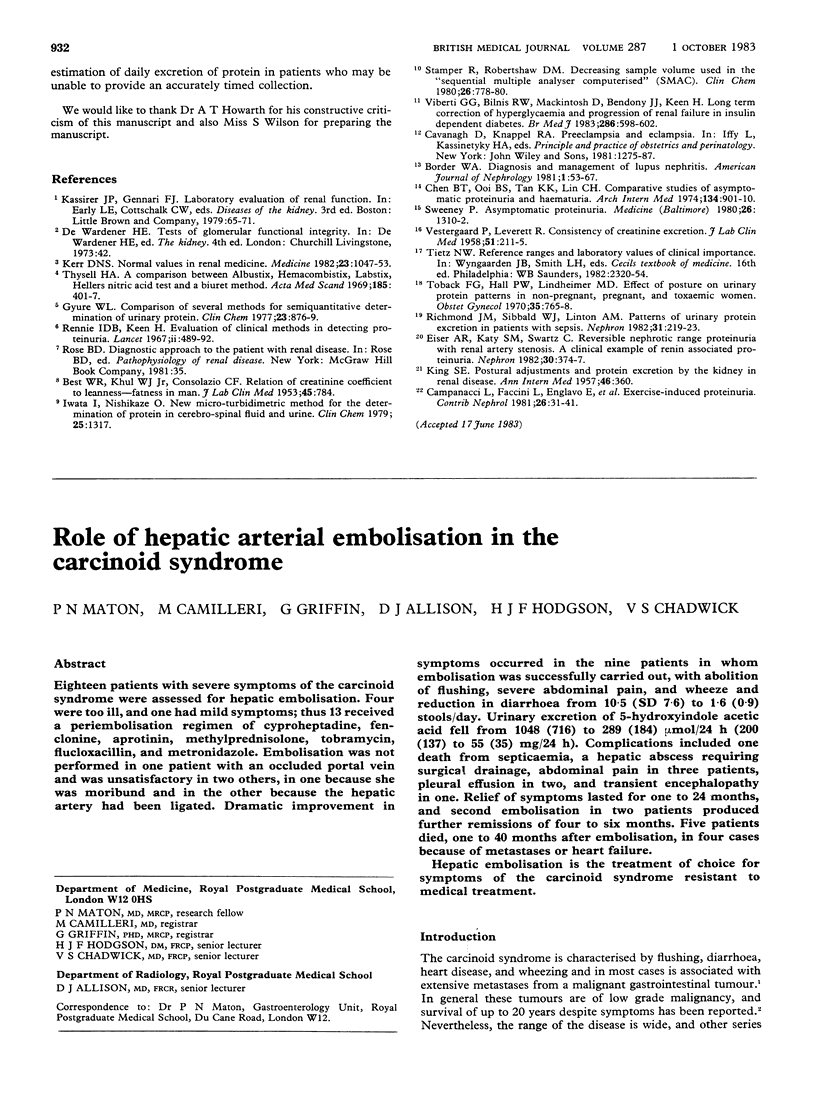
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allison D. J., Modlin I. M., Jenkins W. J. Treatment of carcinoid liver metastases by hepatic-artery embolisation. Lancet. 1977 Dec 24;2(8052-8053):1323–1325. doi: 10.1016/s0140-6736(77)90369-5. [DOI] [PubMed] [Google Scholar]
- Déry R. Theoretical and clinical considerations in anaesthesia for secreting carcinoid tumors. Can Anaesth Soc J. 1971 May;18(3):245–263. doi: 10.1007/BF03025460. [DOI] [PubMed] [Google Scholar]
- Godwin J. D., 2nd Carcinoid tumors. An analysis of 2,837 cases. Cancer. 1975 Aug;36(2):560–569. doi: 10.1002/1097-0142(197508)36:2<560::aid-cncr2820360235>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- MOERTEL C. G., SAUER W. G., DOCKERTY M. B., BAGGENSTOSS A. H. Life history of the carcinoid tumor of the small intestine. Cancer. 1961 Sep-Oct;14:901–912. doi: 10.1002/1097-0142(196109/10)14:5<901::aid-cncr2820140502>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Mays E. T., Wheeler C. S. Demonstration of collateral arterial flow after interruption of hepatic arteries in man. N Engl J Med. 1974 May 2;290(18):993–996. doi: 10.1056/NEJM197405022901804. [DOI] [PubMed] [Google Scholar]
- Melia W. M., Nunnerley H. B., Johnson P. J., Williams R. Use of arterial devascularization and cytotoxic drugs in 30 patients with the carcinoid syndrome. Br J Cancer. 1982 Sep;46(3):331–339. doi: 10.1038/bjc.1982.208. [DOI] [PMC free article] [PubMed] [Google Scholar]


