Abstract
Background
SLC/CCL21, normally expressed in high endothelial venules and in T cell zones of spleen and lymph nodes, strongly attracts T cells and dendritic cells (DC). We have previously shown that SLC/CCL21-mediated anti-tumor responses are accompanied by significant induction of IFNγ and the CXC chemokines, monokine induced by IFNγ (MIG/CXCL9) and IFNγ-inducible protein-10 (IP-10/CXCL10).
Results
We assessed the importance of IFNγ, IP-10/CXCL10 and MIG/CXCL9 in SLC/CCL21 therapy. In vivo depletion of IP-10/CXCL10, MIG/CXCL9 or IFNγ significantly reduced the anti-tumor efficacy of SLC/CCL21. Assessment of cytokine production at the tumor site showed an interdependence of IFNγ, MIG/CXCL9 and IP-10/CXCL10; neutralization of any one of these cytokines caused a concomitant decrease in all three cytokines. Similarly, neutralization of any one of these cytokines led to a decrease in the frequency of CXCR3+ve T cells and CD11c+ve DC at the tumor site.
Conclusion
These findings indicate that the full potency of SLC/CCL21-mediated anti-tumor responses require in part the induction of IFNγ, MIG/CXCL9 and IP-10/CXCL10.
Background
SLC/CCL21, normally expressed in high endothelial venules and in T cell zones of spleen and lymph nodes, strongly attracts T cells and dendritic cells (DC) [1-8]. SLC/CCL21 recruits both naïve lymphocytes and antigen stimulated DC into T cell zones of secondary lymphoid organs, co-localizing these early immune response constituents that culminate in cognate T cell activation [1]. The capacity to facilitate the co-localization of both DC and T cells forms a strong rationale for the use of SLC/CCL21 in cancer therapy. In previous studies we have shown that the SLC/CCL21-mediated anti-tumor responses are accompanied by the enhanced elaboration of IFNγ, IP-10/CXCL10, MIG/CXCL9, GM-CSF and IL-12, but decreased PGE2, VEGF, IL-10, and TGF-β at the tumor site [9,10]. In addition, there was a marked increase in CD4+ and CD8+ cells secreting IFNγ and GM-CSF as well as DC expressing CD11c infiltrating the tumors. MIG/CXCL 9 and IP-10/CXCL10 are glutamine-leucine-arginine (ELR)-negative CXC chemokines that are potent chemoattractants for activated T cells [11-13]. These chemokines also have in common the ability to signal through a G protein-coupled receptor, CXCR3, expressed on activated T lymphocytes. IP-10/CXCL10, MIG/CXCL9 and IFNγ are known to have potent anti-tumor activities in vivo [14-17]. Both MIG/CXCL9 and IP-10/CXCL10 are important for the anti-tumor activity mediated by IFNγ inducing cytokines such as IL-12 [16,18,19]. Based on these findings we hypothesized that augmentation in IFNγ, MIG/CXCL9, and IP-10/CXCL10 would play an important role in the SLC/CCL21-mediated anti-tumor response. Here we show that the cytokines IFNγ, IP-10/CXCL10 and MIG/CXCL9 serve as effector molecules in SLC/CCL21-mediated anti-tumor responses.
Results and Discussion
Host antigen presenting cells (APC) are critical for the cross-presentation of tumor antigens [20]. However tumors have the capacity to limit APC maturation, function and infiltration of the tumor site [21-24]. Thus molecules that attract host APC and T cells could serve as potent agents for cancer immunotherapy. A potentially effective pathway to restore Ag presentation is the establishment of a chemotactic gradient that favors localization of both activated DC and Type 1 cytokine producing lymphocytes at the tumor site. SLC/CCL21, a CC chemokine expressed in high endothelial venules and in T cell zones of spleen and lymph nodes, strongly attracts naive T cells and DCs [1-8]. Because DCs are potent APCs that function as principal activators of T cells, the capacity to facilitate the co-localization of both DC and T cells may reverse tumor-mediated immune suppression and orchestrate effective cell-mediated immune responses [9,10,25-27]. In addition to its immunotherapeutic potential, SLC/CCL21 has been found to have potent angiostatic effects [28], thus adding further support for its use in cancer therapy. Based on these dual capacities, we as well as others have begun pre-clinical evaluation of SLC/CCL21 in several tumor models [9,10,25-27].
Utilizing two transplantable murine lung cancer models, we have previously shown that the anti-tumor efficacy of SLC/CCL21 is T cell-dependent [9]. In both models recombinant SLC/CCL21 administered intratumorally led to complete tumor eradication in 40 % of the treated mice. Studies performed in CD4 and CD8 knockout mice also revealed a requirement for both CD4 and CD8 lymphocytes subsets for SLC/CCL21 mediated tumor regression. Consistent with these findings we found that SLC therapy did not alter tumor growth in SCID mice. In immune competent mice, intratumoral injection of SLC/CCL21 led to a significant increase in CD4 and CD8 T lymphocytes as well as DC infiltrating the tumor and the draining lymph nodes. The cellular infiltrates were accompanied by an enhanced elaboration of IL-12, IFNγ, IP-10/CXCL10 and MIG/CXCL9 at the tumor site [9].
SLC/CCL21 is documented to have direct anti-angiogenic effects [28,29]; the tumor reductions observed in this model could have been due to participation by T cells secreting IFNγ leading to inhibition of angiogenesis via MIG/CXCL9 and IP-10/CXCL10, as well as T cell-dependent immunity [16]. IFNγ mediates a range of biological effects that facilitate anticancer immunity. MIG/CXCL9 and IP-10/CXCL10 are potent angiostatic factors that are induced by IFNγ [14,16,17]. Both MIG/CXCL9 and IP-10/CXCL10 are chemotactic for stimulated CXCR3-expressing activated T lymphocytes that could further amplify IFNγ at the tumor site [30]. Hence we postulated that in addition to IFNγ, IP-10/CXCL10 and MIG/CXCL9 would also be important contributors to the tumor reduction in the context of SLC/CCL21 therapy.
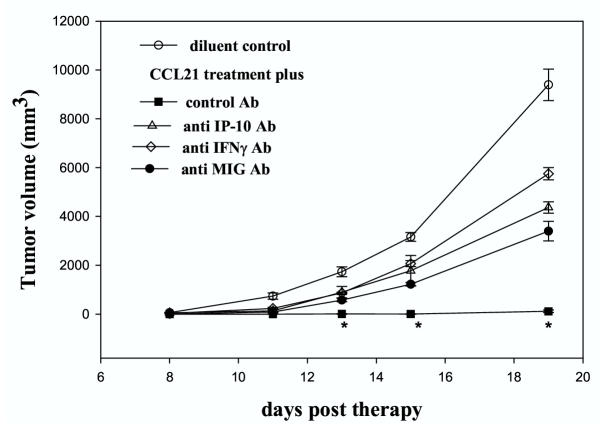
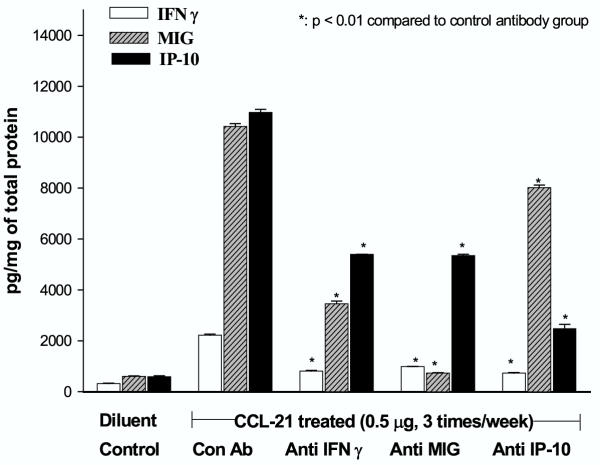
To determine the importance of MIG/CXCL9, IP-10/CXCL10 and IFNγ in the SLC/CCL21 mediated antitumor response, these cytokines were depleted in SLC/CCL21-treated mice. Anti-IP-10/CXCL10, MIG/CXCL9 and IFNγ antibodies each partially but yet significantly inhibited the anti-tumor efficacy of SLC/CCL21 (Figure 1 * p < 0.01 compared to the control antibody group). Neutralization of IFNγ caused a significant decrease in both MIG/CXCL9 and IP-10/CXCL10 indicating that these chemokines are largely IFNγ dependent. Thus, an increase in IFNγ at the tumor site of SLC/CCL21-treated mice could explain the relative increases in IP-10/CXCL10 and MIG/CXCL9. The converse was also observed; IFNγ production at the tumor site was found to be MIG/CXCL9- and IP-10/CXCL10-dependent as indicated by the fact that neutralization of these cytokines caused a significant decrease in IFNγ(Figure 2). Neutralization of any one of these cytokines caused a concomitant decrease in all three cytokines, thus indicating that IFNγ, MIG/CXCL9 and IP-10/CXCL10 are interdependent in the SLC/CCL21-mediated anti-tumor responses. Based on these findings, we speculated that the decrease of IP-10/CXCL10 and MIG/CXCL9 led to a decrease in IFNγ by limiting the influx of T cells producing IFNγ at the tumor site. Because MIG/CXCL9 and IP-10/CXCL10 are chemotactic for stimulated CXCR3 expressing activated T lymphocytes, we determined if neutralizing these chemokines in vivo in the SLC/CCL21-treated mice would decrease the frequency of CXCR3 expressing T cells at the tumor sites. Compared to SLC/CCL21-treated mice receiving control antibody, flow cytometric evaluation of single-cell suspensions of non-necrotic tumors from SLC/CCL21-treated mice receiving neutralizing antibodies to MIG/CXCL9, IP-10/CXCL10 and IFNγ showed 10, 12 and 31 % decreases, respectively, in the gated CD3 CXCR3+ve T cell populations (Table 1). The fact that neutralization of IFNγ was the most efficient at decreasing the total number of CXCR3-activated T cells may be due to the decrease in the IFNγ-dependent CXCR3 ligands MIG/CXCL9 and IP-10/CXCL10. Individually, neutralizing MIG/CXCL9 and/or IP-10/CXCL10 only led to a partial decrease in the total number of CXCR3-activated T cells. Because MIG/CXCL9 and IP-10/CXCL10 share the same receptor (CXCR3), one possible explanation of a partial decrease in CXCR3-activated T cells is that neutralization of one ligand may overexpose the receptor to the other ligand. Furthermore, because murine SLC/CCL21 binds CXCR3 receptor, SLC/CCL21 may be recruiting CXCR3+ve T cells directly. An alternative explanation is that residual cytokines such as IFN-inducible T cell α chemoattractant (ITAC/CXCL11) present after in vivo neutralization of IFNγ, MIG, IP-10 may have remaining activity and attract CXCR3+ve T cells. Our results imply that all 3 cytokines, IFNγ, MIG and IP-10 play interrelated roles in the recruitment of CXCR3-activated T cells in SLC/CCL21-mediated anti-tumor responses. While the number of CD4 and CD8 cells remained unaltered, compared to SLC/CCL21-treated mice receiving control antibody, mice administered neutralizing antibodies to MIG/CXCL9, IP-10/CXCL10 and IFNγ showed respective decreases of 38, 28 and 16% in the number of CD11c+ DEC205+ DC infiltrating the tumor (Table 1). At present it is not clear why there is a decrease in DC following neutralization of MIG/CXCL9, IP-10/CXCL10 and IFNγ. A plausible explanation is that these cytokines may be involved in complex interactions with other molecules that are chemotactic for DC. Further studies are required to delineate the mechanisms responsible for MIG/CXCL9, IP-10/CXCL10 and IFNγ mediated localization of DC at the tumor site.
Figure 1.
10 5 3 LL tumors were implanted in C57Bl/6 mice. 5 days following tumor implantation, mice were treated intratumorally with recombinant murine SLC/CCL21 (0.5 μg) 3X/week. One day before SLC/CCL21 administration, mice were given the respective cytokine antibody by i.p. injection. The antibodies were administered three times per week. Antibodies to: IP-10/CXCL10, MIG/CXCL9 and IFNγ significantly inhibited the antitumor efficacy of SLC/CCL21 (*p < 0.01 compared to the control antibody treated group). n = 8 mice group
Figure 2.
SLC/CCL21-treated mice had a significant induction in IFNγ, MIG/CXCL9 and IP-10/CXCL10 at the tumor site compared to diluent treated control tumor bearing mice (p < 0.001). Assessment of cytokine production at the tumor site of SLC/CCL21 treated mice receiving anti-IFNγ, anti MIG/CXCL9 and anti IP-10/CXCL10 showed an interdependence of IFNγ, MIG/CXCL9 and IP-10/CXCL10: neutralization of any one of these cytokines in vivo caused a concomitant decrease in all three cytokines (*p < 0.01 compared to the control antibody treated group). Results are expressed as pg/mg of total protein. Total protein was determined by the Bradford assay. n= 8 mice per group
Table 1.
Neutralization of IP-10, MIG and IFNγ reduces the frequency of CD3+CXCR3+ T lymphocytes and CD11C+ DEC205+ DC at the tumor site of SLC/CCL21-treated mice
| + Anti IP-10 | + Anti MIG | + Anti IFNγ | + anti Control Ab | Diluent Control | ||||||
| % | MCF | % | MCF | % | MCF | % | MCF | % | MCF | |
| CD4 | 13 | 44 | 14 | 47 | 13 | 40 | *13 | 42 | *6 | 48 |
| CD8 | 35 | 57 | 34 | 55 | 32 | 50 | *33 | 52 | *26 | 52 |
| CD3CXCR3 | **28 | 58 | **27 | 57 | **23 | 55 | * 34 | 59 | *12 | 58 |
| CD11C+DEC 205+ | **10 | 111 | **9 | 110 | **11 | 101 | *14 | 105 | *4 | 100 |
Single cell suspensions of non-necrotic tumor nodules from SLC/CCL21 treated mice receiving neutralizing antibodies to P-10/CXCL10, MIG/CXCL9, IFNγ, control Ab and diluent treated tumor bearing mice were prepared. Cell surface staining for T cell markers CD4, CD8, CD3, and the chemokine receptor CXCR3 as well as DC markers CD11C and DEC205 were evaluated by flow cytometry. Cells were identified as lymphocytes or DC by gating on the forward and side scatter profiles; 10,000 gated events were collected and analyzed using Cell Quest software. Within the gated T lymphocyte population, intratumoral injection of SLC/CCL21 led to an increase in the frequency of CD4+, CD8+, CD3+CXCR3+ events compared to the diluent control (*p < 0.001). Within the gated DC population, intratumoral injection of SLC/CCL21 led to an increase in the frequency of CD11C+DEC205+ events compared to the diluent control (*p < 0.001). Compared to SLC/CCL21-treated mice receiving control antibody, mice receiving neutralizing antibodies to IP-10/CXCL10, MIG/CXCL9, and IFNγ showed decrease in the gated CD3+CXCR3+ T cell as well as CD11C+DEC205 + DC events (**p < 0.01) (n = 8 mice per group). MCF is mean channel fluorescence intensity. CD3+CXCR3+ MCF is for CXCR3. CD11C+DEC205+, MCF is for DEC205.
Conclusions
Our results suggest that the anti-tumor properties of SLC/CCL21 may be due to its chemotactic capacity in co-localization of DC and T cells as well as in part to the induction of key cytokines such as IFNγ, IP-10/CXCL10 and MIG/CXCL9.
Materials and Methods
Reagents
Abs to murine IFNγ, recombinant IFNγ were obtained from PharMingen (San Diego, CA). Abs to murine MIG/CXCL9, IP-10/CXCL10 and recombinant cytokine standards was purchased from R&D (Minneapolis, MN). Recombinant SLC/CCL21 was obtained from PeproTech. (Rocky Hill, NJ). Polyclonal goat anti-murine MIG/CXCL9 and anti-murine IP-10/CXCL10 specific anti-serum were produced and characterized as previously described [31]. Anti-mouse IFNγ monoclonal (R4-462, American Type Culture Collection, Rockville, Maryland, MD) neutralizing antibody was purified by affinity chromatography from SCID mice ascites, which was generated 3–4 weeks after intraperitoneal injection of 106 R4-462 hybridoma cells per mouse [32]. For flow cytometry, labeled antibodies (FITC, PE, PerCP) against the T cell surface markers to CD3, CD4, CD8 and against the DC markers, CD11c and DEC 205 and the appropriate controls were purchased from PharMingen. FITC labeled anti-rabbit IgG was purchased from PharMingen. Rabbit anti-mouse CXCR3 antibody was purchased from Zymed Laboratories Inc. (So. San Francisco, CA). Murine serum albumin (Sigma, St. Louis, MO) was utilized as control injections for SLC/CCL21.
Cell culture and tumorigenesis model
A weakly immunogenic lung cancer, Lewis lung carcinoma (3LL, H-2b) obtained from ATCC (CRL-1642, LLC) was utilized for assessment of cytokines important for SLC/CCL21 – mediated anti-tumor responses in vivo. The cells were routinely cultured as monolayers in 25 cm3 tissue culture flasks containing RPMI 1640 medium (Irvine Scientific, Santa Anna, CA) supplemented with 10% fetal bovine serum (FBS) (Gemini Bioproducts, Calabasas, CA), penicillin (100 U/ml), streptomycin (0.1 mg/ml), 2 mM glutamine (JRH Biosciences, Lenexa, KS) and maintained at 37°C in a humidified atmosphere containing 5% CO2 in air. The cell lines were mycoplasma free and cells were utilized up to the tenth passage before thawing frozen stock cells from liquid N2.
For tumorigenesis experiments, 105 3LL tumor cells were inoculated by s.c. injection in the right supra scapular area of C57Bl/6 mice and tumor volumes were monitored three times each week. Five day established tumors were treated with intratumoral injection of 0.5 μg of recombinant murine SLC/CCL21 (Pepro Tech, Rocky Hill, NJ) or murine serum albumin (utilized as an irrelevant protein for control injections) were administered three times per week for two weeks as previously described [9]. 24 h prior to SLC/CCL21 treatment, and then three times a week, mice were injected i.p. with 1 ml/dose of anti-IP-10/CXCL10, or anti-MIG/CXCL9, or 100 μg/dose of purified monoclonal anti-IFNγ or appropriate control antibodies (goat IgG and rat IgG) at equivalent doses for the duration of the experiment. In response to these antibodies, there was a significant reduction of the respective cytokines in vivo (Figure 2). Tumor volume was calculated as previously described [9].
Cytokine ELISA
MIG/CXCL9, IP-10/CXCL10 and IFNγ were quantified using a modification of a double ligand method as previously described [33].
Flow Cytometry
Flow cytometric analyses for T cell and DC markers were performed on a FACScan flow cytometer (Becton Dickinson, San Jose, CA) in the University of California, Los Angeles, Jonsson Cancer Center Flow Cytometry Core Facility. Cells were identified as lymphocytes or DC by gating based on forward and side scatter profiles. CD11c+ve DCs were defined as the bright populations within tumor nodules. 10,000-gated events were collected and analyzed using Cell Quest software (Becton Dickinson). For staining, two or three fluorochromes (PE, FITC, PerCP) (PharMingen) were used to gate on the CD3, CD4 and CD8 T lymphocyte population or CD11c +ve DC in single cell suspensions from tumor nodule. For CXCR3 expression, T cells were doubly stained for CD3 and CXCR3 cell surface markers.
Statistical Analysis
Groups of 8 mice were used. Statistical analyses of the data in figures 1, 2 and in table 1 were performed using the paired Student t test.
Author's contributions
Author 1 SS and Author 2 SCY coordinated and carried out all the experiments. Authors SH, LXZ, MH, RKB and MDB contributed to the discussion of the article. Author JFL together with SS performed the statistical analyses. Authors RMS and SMD together with SS conceived of the study, participated in its design and drafted the manuscript.
All authors read and approved the final manuscript
Acknowledgments
Acknowledgements
We thank Kimberly Atianzar for excellent technical assistance in conducting the ELISA measurements. National Institutes of Health Grant R01 CA78654, CA85686, P50 CA90388, Medical Research Funds from the Department of Veterans Affairs, The Research Enhancement Award Program in Cancer Gene Medicine and the Tobacco-Related Disease Research Program of the University of California supported this work.
Contributor Information
Sherven Sharma, Email: sharmasp@ucla.edu.
Seok-Chul Yang, Email: yangsc@ucla.edu.
Sven Hillinger, Email: hillings@ucla.edu.
Li X Zhu, Email: LZhu@mednet.ucla.edu.
Min Huang, Email: minhuang@ucla.edu.
Raj K Batra, Email: rbatra@ucla.edu.
Jeff F Lin, Email: j-lin5@northwestern.edu.
Marie D Burdick, Email: MBurdick@mednet.ucla.edu.
Robert M Strieter, Email: RStrieter@mednet.ucla.edu.
Steven M Dubinett, Email: SDubinett@mednet.ucla.edu.
References
- Cyster J G. Chemokines and the Homing of Dendritic Cells to the T Cell Areas of Lymphoid Organs. J Exp Med. 1999;189:447–450. doi: 10.1084/jem.189.3.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogata M, Zhang Y, Wang Y, Itakura M, Zhang Y, Harada A, Hashimoto S, Matsushima K. Chemotactic Response Toward Chemokines and Its Regulation by Transforming Growth Factor-beta1 of Murine Bone Marrow Hematopoietic Progenitor Cell-Derived Different Subset of Dendritic Cells. Blood. 1999;93:3225–3232. [PubMed] [Google Scholar]
- Chan VW, Kothakota S, Rohan MC, Panganiban-Lustan L, Gardner JP, Wachowicz MS, Winter JA, Williams LT. Secondary lymphoid-tissue chemokine (SLC) is chemotactic for mature dendritic cells. Blood. 1999;93:3610–6. [PubMed] [Google Scholar]
- Hedrick JA, Zlotnik A. Identification and characterization of a novel beta chemokine containing six conserved cysteines. J Immunol. 1997;159:1589–93. [PubMed] [Google Scholar]
- Hromas R, Kim CH, Klemsz M, Krathwohl M, Fife K, Cooper S, Schnizlein-Bick C, Broxmeyer HE. Isolation and characterization of Exodus-2, a novel C-C chemokine with a unique 37-amino acid carboxyl-terminal extension. J Immunol. 1997;159:2554–8. [PubMed] [Google Scholar]
- Nagira M, Imai T, Yoshida R, Takagi S, Iwasaki M, Baba M, Tabira Y, Akagi J, Nomiyama H, Yoshie O. A lymphocyte-specific CC chemokine, secondary lymphoid tissue chemokine (SLC), is a highly efficient chemoattractant for B cells and activated T cells. Eur J Immunol. 1998;28:1516–23. doi: 10.1002/(SICI)1521-4141(199805)28:05<1516::AID-IMMU1516>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Tanabe S, Lu Z, Luo Y, Quackenbush EJ, Berman MA, Collins-Racie LA, Mi S, Reilly C, Lo D, Jacobs KA, Dorf ME. Identification of a new mouse beta-chemokine, thymus-derived chemotactic agent 4, with activity on T lymphocytes and mesangial cells. J Immunol. 1997;159:5671–9. [PubMed] [Google Scholar]
- Willimann K, Legler DF, Loetscher M, Roos RS, Delgado MB, Clark-Lewis I, Baggiolini M, Moser B. The chemokine SLC is expressed in T cell areas of lymph nodes and mucosal lymphoid tissues and attracts activated T cells via CCR7. Eur J Immunol. 1998;28:2025–34. doi: 10.1002/(SICI)1521-4141(199806)28:06<2025::AID-IMMU2025>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Sharma S, Stolina M, Luo J, Strieter RM, Burdick M, Zhu LX, Batra RK, Dubinett SM. Secondary lymphoid tissue chemokine mediates T cell-dependent antitumor responses in vivo. J Immunol. 2000;164:4558–63. doi: 10.4049/jimmunol.164.9.4558. [DOI] [PubMed] [Google Scholar]
- Sharma S, Stolina M, Zhu L, Lin Y, Batra R, Huang M, Strieter R, Dubinett S. Secondary Lymphoid Organ Chemokine Reduces Pulmonary Tumor Burden in Spontaneous Murine Bronchoalveolar Cell Carcinoma. Cancer Research. 2001;61:6406–6412. [PubMed] [Google Scholar]
- Taub DD, Lloyd AR, Conlon K, Wang JM, Ortaldo JR, Harada A, Matsushima K, Kelvin DJ, Oppenheim JJ. Recombinant human interferon-inducible protein 10 is a chemoattractant for human monocytes and T lymphocytes and promotes T cell adhesion to endothelial cells. J Exp Med. 1993;177:1809–14. doi: 10.1084/jem.177.6.1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao F, Rabin RL, Yannelli JR, Koniaris LG, Vanguri P, Farber JM. Human Mig chemokine: biochemical and functional characterization. J Exp Med. 1995;182:1301–14. doi: 10.1084/jem.182.5.1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loetscher M, Gerber B, Loetscher P, Jones SA, Piali L, Clark-Lewis I, Baggiolini M, Moser B. Chemokine receptor specific for IP10 and mig: structure, function, and expression in activated T-lymphocytes [see comments] J Exp Med. 1996;184:963–9. doi: 10.1084/jem.184.3.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strieter RM, Kunkel SL, Arenberg DA, Burdick MD, Polverini PJ. Interferon gamma-inducible protein 10 (IP-10), a member of the C-X-C chemokine family, is an inhibitor of angiogenesis. Biochem Biophys Res Commun. 1995;210:51–7. doi: 10.1006/bbrc.1995.1626. [DOI] [PubMed] [Google Scholar]
- Addison C, Arenberg D, Morris S, Xue Y, Burdick M, Mulligan M, Iannettoni M, Strieter R. The CXC chemokine, monokine induced by interferon gamma, inhibits non-small cell lung carcinoma tumor growth and metastasis. Hum Gene Ther. 2000;11:247–61. doi: 10.1089/10430340050015996. [DOI] [PubMed] [Google Scholar]
- Tannenbaum CS, Tubbs R, Armstrong D, Finke JH, Bukowski RM, Hamilton TA. The CXC chemokines IP-10 and Mig are necessary for IL-12-mediated regression of the mouse RENCA tumor. J Immunol. 1998;161:927–32. [PubMed] [Google Scholar]
- Arenberg DA, Kunkel SL, Polverini PJ, Morris SB, Burdick MD, Glass MC, Taub DT, Iannettoni MD, Whyte RI, Strieter RM. Interferon-gamma-inducible protein 10 (IP-10) is an angiostatic factor that inhibits human non-small cell lung cancer (NSCLC) tumorigenesis and spontaneous metastases. J Exp Med. 1996;184:981–92. doi: 10.1084/jem.184.3.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanegane C, Sgadari C, Kanegane H, Feldstein tJ, Yao L, Gupta G, Farber JM, Liao F, Liu L, Tosato G. Contribution of the CXC chemokines IP-10 and Mig to theantitumor effects of IL-12. J Leukocyte Biol. 1998;64:384. doi: 10.1002/jlb.64.3.384. [DOI] [PubMed] [Google Scholar]
- Pertl U, Luster AD, Varki NM, Homann D, Gaedicke G, Reisfeld RA, Lode HN. IFN-gamma-inducible protein-10 is essential for the generation of a protective tumor-specific CD8 T cell response induced by single-chain IL-12 gene therapy. J Immunol. 2001;166:6944–51. doi: 10.4049/jimmunol.166.11.6944. [DOI] [PubMed] [Google Scholar]
- Huang AYC, Golumbek P, Ahmadzadeh M, Jaffee E, Pardoll D, Levitsky H. Role of bone marrow-derived cells in presenting MHC class I-restricted tumor antigens. Science. 1994;264:961–965. doi: 10.1126/science.7513904. [DOI] [PubMed] [Google Scholar]
- Gabrilovich DI, Chen HL, Girgis KR, Cunningham HT, Meny GM, Nadaf S, Kavanaugh D, Carbone DP. Production of vascular endothelial growth factor by human tumors inhibits the functional maturation of dendritic cells. Nat Med. 1996;2:1096–103. doi: 10.1038/nm1096-1096. [DOI] [PubMed] [Google Scholar]
- Qin Z, Noffz G, Mohaupt M, Blankenstein T. Interleukin-10 prevents dendritic cell accumulation and vaccination with granulocyte-macrophage colony-stimulating factor gene-modified tumor cells. J Immunol. 1997;159:770–776. [PubMed] [Google Scholar]
- Gabrilovich DI, Corak J, Ciernik IF, Kavanaugh D, Carbone DP. Decreased antigen presentation by dendritic cells in patients with breast cancer. Clin Cancer Res. 1997;3:483–90. [PubMed] [Google Scholar]
- Gabrilovich D, Ishida T, Oyama T, Ran S, Kravtsov V, Nadaf S, Carbone DP. Vascular endothelial growth factor inhibits the development of dendritic cells and dramatically affects the differentiation of multiple hematopoietic lineages in vivo. Blood. 1998;92:4150–66. [PubMed] [Google Scholar]
- Arenberg DA, Zlotnick A, Strom SRB, Burdick MD, Strieter RM. The murine CC chemokine, 6Ckine, inhibits tumor growth and angiogenesis in a human lung cancer SCID mouse model. Cancer Immunology Immunotherapy. 2000;49:587–592. doi: 10.1007/s002620000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicari AP, Yahia SA, Chemin K, Mueller A, Zlotnik A, Caux C. Antitumor effects of the Mouse Chemokine 6Ckine/SLC through angiostatic and Immunological mechanisms. J Immunol. 2000;165:1992–2000. doi: 10.4049/jimmunol.165.4.1992. [DOI] [PubMed] [Google Scholar]
- Kirk CJ, Hartigan-O'Connor D, Nickoloff BJ, Chamberlain JS, Giedlin M, Aukerman L, Mule JJ. T cell-dependent antitumor immunity mediated by secondary lymphoid tissue chemokine: augmentation of dendritic cell-based immunotherapy. Cancer Res. 2001;61:2062–70. [PubMed] [Google Scholar]
- Soto H, Wang W, Strieter RM, Copeland NG, Gilbert DJ, Jenkins NA, Hedrick J, Zlotnik A. The CC chemokine 6Ckine binds the CXC chemokine receptor CXCR3. Proc Natl Acad Sci U S A. 1998;95:8205–10. doi: 10.1073/pnas.95.14.8205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arenberg D, Zlotnick A, Strom S, Burdick M, Strieter R. Inhibition of lung cancer growth by the novel chemokine 6C-kine. Am J Resp Crit Care Med. 1999;159:A746. [Google Scholar]
- Farber JM. Mig and IP-10: CXC chemokines that target lymphocytes. J Leukoc Biol. 1997;61:246–57. [PubMed] [Google Scholar]
- Belperio JA, Keane MP, Burdick MD, Lynch JP, 3rd, Xue YY, Li K, Ross DJ, Strieter RM. Critical role for CXCR3 chemokine biology in the pathogenesis of bronchiolitis obliterans syndrome. J Immunol. 2002;169:1037–49. doi: 10.4049/jimmunol.169.2.1037. [DOI] [PubMed] [Google Scholar]
- Spitalny GL, Havell EA. Monoclonal antibody to murine gamma interferon inhibits lymphokine-induced antiviral and macrophage tumoricidal activities. J Exp Med. 1984;159:1560–5. doi: 10.1084/jem.159.5.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Standiford TJ, Kunkel SL, Basha MA, Chensue SW, III JPL, Toews GB, Westwick J, Strieter RM. Interleukin-8 gene expression by a pulmonary epithelial cell line: A model for cytokine networks in the lung. J Clin Invest. 1953;86:1945–1990. doi: 10.1172/JCI114928. [DOI] [PMC free article] [PubMed] [Google Scholar]