Figure 1.
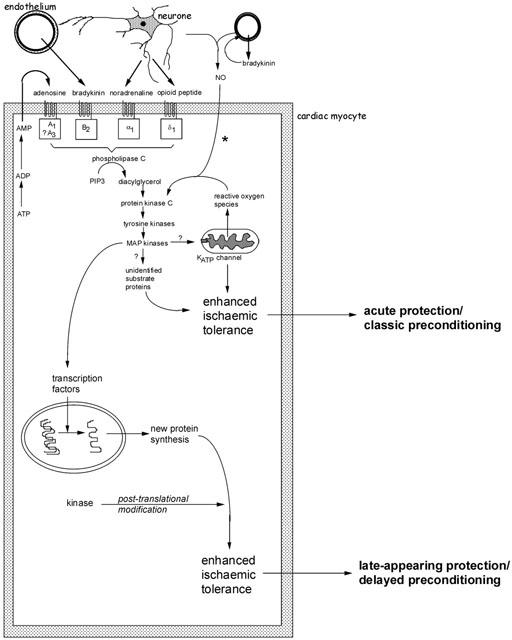
Schematic representation of the major identified pathways of early and delayed forms of preconditioning. Several autocrine/paracrine mediators released during the period of preconditioning ischaemia act on G-protein coupled receptors and are known to participate in the infarct-limiting effect of ischaemic preconditioning. These include adenosine released during ischaemia as a result of ATP breakdown, bradykinin released from vascular endothelium and mediators of neural origin (noradrenaline and opioid peptides). Reactive oxygen species, especially superoxide anion generated as a result of mitochondrial uncoupling, may also act as upstream mediators. A complex signal cascade is activated which involves activation of protein kinase C isoenzymes, tyrosine kinases and mitogen-activated protein kinases. The phosphorylation cascade is thought to result in activation of the ATP-sensitive potassium (KATP) channel on the mitochondrial inner membrane. At present it remains unknown how opening of this channel confers protection during ischaemia. The participation of other ‘cytoprotective' proteins has been proposed, including proteins that suppress or modulate apoptosis and proteins associated with cytoskeletal integrity (αB-crystallin and 27 kDa heat shock protein). *The participation of endogenous NO (of endothelial or neural origin) in initiating the classical preconditioning mechanism may be model specific. Early protection against cell death and infarction is not NO-dependent whereas preconditioning against arrhythmias does involve NO generation. For delayed preconditioning, evidence for the involvement of NO (possibly as a signalling intermediate downstream of bradykinin) is more persuasive and consistent. The distinguishing feature of delayed preconditioning is the co-ordinated regulation of a gene transcription programme as a result of upstream kinase signalling. The delayed phase of protection is dependent on de novo synthesis of inducible proteins. Those thought to be particularly important in the acquisition of delayed tolerance to ischaemia include iNOS, cyclo-oxygenase-2 and intracellular antioxidant enzymes such as manganese – superoxide dismutase. For more detailed discussion see Baxter & Ferdinandy (2001).
