Abstract
Several studies have shown that in the arterial wall hepatocyte growth factor/scatter factor (HGF/SF) is expressed by smooth muscle cells (SMCs) but acts on endothelial cells, not SMCs. Other studies, however, have indicated that SMCs can respond to HGF/SF. We have reinvestigated expression and activity of HGF/SF and its receptor MET in arterial SMC and endothelial cell cultures and in whole arteries after superficial or deep injury or atherogenesis. High-density cultures of SMCs produced HGF/SF but did not express MET, whereas SMCs, at the leading edge of injured cultures, expressed both ligand and receptor and showed a dramatic motility and growth response to HGF/SF. In line with these results, HGF/SF and MET expression was undetectable in the media of uninjured carotid arteries but was induced after deep arterial injury in areas of SMC migration in the neointima. Strong MET expression was also observed in the SMCs of the atherosclerotic lesions of homozygous apoE−/− mice, whereas HGF/SF was expressed by macrophage-derived foam cells. These results demonstrate that MET is induced in migrating and proliferating SMCs and that HGF/SF and MET are key mediators of the SMC response in atherogenesis.
The migration of vascular smooth muscle cells (SMCs) from the media layer to the intima and intimal proliferation is a key feature of the pathogenesis of atherosclerosis. This cellular response is accompanied by a striking removal from the cells’ contractile phenotype as intimal SMCs actively synthesize matrix components and become lipid-filled.1–5
Several lines of evidence imply a critical role for platelet-derived growth factor (PDGF) in SMC migration and in the development of the SMC-rich atherosclerotic lesions. Administration of PDGF after injury causes increased intimal thickening,6 and neutralizing of the PDGF antibodies7 or inhibitors of the PDGF receptor kinase8 reduce intimal thickening. Similarly, antibodies to basic fibroblast growth factor delay the progression of rat carotid lesions after catheter injuries.9 This firmly establishes a role for PDGF and fibroblast growth factor in atherogenesis, but it is often assumed that additional molecules are involved.
Hepatocyte growth factor/scatter factor (HGF/SF) is a high-molecular weight polypeptide growth factor initially discovered for its activity as a mitogen for liver cells10–12 and as a motility factor for epithelial cells.13,14 The factor induces growth and/or motility in target cells through a tyrosine kinase receptor encoded by the MET proto-oncogene.15,16 HGF/SF and its homologue HGF1/macrophage-stimulating protein17,18 define a distinct family of high-molecular weight growth factors whose members share the domain structure and the mechanism of activation of the blood proteinase precursor plasminogen.19 Similar to plasminogen, HGF/SF is produced as an inactive single-chain protein (pro-HGF/SF) that is subsequently converted into a two-chain, biologically active heterodimer. This conversion is catalyzed by urokinase- and tissue-type20,21 plasminogen activators and by another serine proteinase closely related to factor XII.22 Thus, vertebrate organisms have evolved a single enzymatic pathway that controls clotting and fibrinolysis and the cell response to plasminogen-related growth factors.
There is now conclusive evidence from gene targeting experiments in mice for essential roles of HGF/SF and MET in the development of the placenta, liver, and myogenic precursor cells.23–25 Further, recent genetic experiments26,27 and a wealth of physiological data support critical roles for HGF/SF and MET in the regeneration of liver,26–29 kidney,30 lung,31 and myocardial tissue.32
Several lines of evidence have implicated HGF/SF and MET in the vascular system, suggesting important roles but also leading to divergent conclusions. Early studies by Rosen and colleagues33 established that SMC cultures produce HGF/SF and that endothelial cells (ECs) respond to the factor.34 Subsequent studies revealed a major angiogenic activity for HGF/SF35–40 although failing to detect MET expression39 and/or a response to HGF/SF in SMCs.41,42 These studies led to the view that, in the arterial wall, SMC-derived HGF/SF acts as a paracrine effector of ECs. Other studies, however, have shown that ECs can also produce HGF/SF,43 that SMCs can respond to HGF/SF,44–47 and that intimal SMCs express HGF/SF and MET in rabbit carotid arteries after a balloon injury.48
Why do different studies report such a variable response of SMCs to HGF/SF? We have readdressed this problem by hypothesizing that the response of SMCs to HGF/SF may depend on the phenotypic state of these cells, ie, quiescent versus migratory. We show that, while confluent cultures of SMCs exhibit little or no MET expression, in agreement with earlier reports, sparse or injured cultures express the receptor and show a marked growth and motility response to HGF/SF. We next demonstrate that a transition from a MET− to a MET+ phenotype also occurs in SMCs in vivo during the recovery from experimental balloon injuries and during migration of SMCs from the media to the neointima. Lastly, we demonstrate that MET is highly expressed in SMCs surrounding the atherosclerotic lesions of apoE−/− mice while the ligand is also expressed in the center of the lesion by monocyte-derived foam cells. Together the in vitro and in vivo data establish that HGF/SF and MET are involved in multiple key pathways leading to arterial remodeling and atherogenesis. They also provide a rational framework for the seemingly conflicting data previously reported.
Materials and Methods
Mouse and Human HGF/SF
A full-length cDNA encoding mouse HGF/SF was cloned from a ras-transformed 3T3 fibroblast line (D4) and subcloned into the expression vector pA71. Mouse HGF/SF was purified from culture supernatants using a combination of heparin-Sepharose affinity and Mono S chromatography.14 The human recombinant HGF/SF used in this study was a kind gift from R. Schwall (Genentech, San Francisco, CA).
Antibodies
A neutralizing polyclonal anti-mouse HGF/SF antibody (1W66) was raised in sheep using a recombinant mouse HGF/SF protein, and antibodies were purified by ion exchange chromatography. The biological activity of 1W66 was confirmed by its inhibitory effect on HGF/SF-induced dispersion of MDCK colonies. Anti-mouse-MET polyclonal antibody was purchased from Santa Cruz Biotechnology (sc-162; Santa Cruz, CA).
Western Blots
For Western blots of conditioned media, rat SMCs (rSMCs) were grown to confluence in Dulbecco’s modified Eagle’s medium (DMEM)/5% fetal calf serum (FCS), washed twice in warm phosphate-buffered saline (PBS), and incubated for 3 days in 50 ml of serum-free DMEM. The conditioned medium was collected, added to phenylmethyl sulfonyl fluoride and N-methylmaleimide (1 mmol/L each), and centrifuged at 1500 × g for 10 minutes at 4°C. It was then filtered and stored at −20°C. Samples were partially purified by heparin-Sepharose chromatography before sodium dodecyl sulfate-polyacrylamide gel electrophoresis. For arterial extracts, rats were culled by suffocation in a rising concentration of carbon dioxide and perfused via the abdominal aorta with ice-cold Krebs buffer supplemented with 1 mmol/L phenylmethyl sulfonyl fluoride and 1 mmol/L N-methyl maleimide. Carotid arteries were dissected free of connective tissue, checked to be free of all blood, and snap-frozen in liquid nitrogen. Arteries were ground under liquid nitrogen using a mortar and pestle, suspended in 100 ml of gel loading buffer, and centrifuged at 13,000 rpm in a microfuge for 5 minutes to pellet and remove cell fragments.
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis was performed on 12.5% gels at 200 V. Gels were washed in transfer buffer (20% methanol, 192 mmol/L glycine, 25 mmol/L Tris, and 0.1 g/L sodium dodecyl sulfate) for 5 minutes, and proteins were transferred onto nitrocellulose membranes at 500 mA for 1 hour in a cooled blotting tank. Membranes were washed in Tris-buffered saline for 5 minutes and incubated in 50 g/L nonfat dried milk in Tris-buffered saline overnight at 4°C. Blots were next incubated with 1W66 prepared in 25 g/L nonfat dried milk in 1 g/L Tween 20 in Tris-buffered saline for 1 hour at room temperature, washed 3 × 10 minutes, and incubated with anti-sheep IgG horseradish peroxidase-conjugated secondary antibody for 1 hour at room temperature before addition of chemiluminescent horseradish peroxidase substrate (ECL substrate, RPN-2106; Amersham, Buckinghamshire, UK) for 1 minute and exposure to film.
Cell Assays
Primary cultures of rSMCs were prepared by outgrowth from aortic explants, based on the method of McMurray and colleagues.49 Passaged cells were maintained in cultured media with 10% FCS and characterized by hills and valley morphology and α-smooth muscle actin immunofluorescence and used between passages 3 to 14. Primary cultures of human SMCs were a kind gift from D. Proudfoot (Department of Medicine, University of Cambridge, Cambridge, UK); they were prepared from medial explants of nondiseased sections of aorta using the same procedure used for rSMCs and used within passage 12. Primary cultures of rat ECs were a kind gift from H. Lauder (Department of Pharmacology, University of Cambridge); they were prepared by outgrowth from aortic rings and used within passage 10. All cultures were tested for and found to be free of mycoplasma.
For scrape injury of SMC or EC cultures, cells were plated at 12,000 cells per well and 8000 cells per well, respectively, onto 96-well plates in 10% FCS in DMEM and grown to confluence. Cultures were then washed in PBS and incubated with 200 ml per well of 0.05% FCS in DMEM for another 48 hours to induce quiescence. A section of cells (30 to 50% of the total cell area) was then scraped from each well using a plastic scraper adapted from the plunger of an Eppendorf AG (Hamburg, FRG) multidispenser pipette tip. The cells were washed twice in PBS at 37°C and incubated in test media diluted in 1 mg/ml bovine serum albumin in DMEM for 24 hours. Cell numbers were measured at the end of the assay using a hemocytometer.
SMC directed migration was measured in a Boyden chamber using the method of Bornfeldt and colleagues50 with PDGF as a positive control. Polyvinylpyrrolidone-free filters of 8-μm pore size (10474; Poretics, Livermore, CA) were coated with fibronectin (for rSMCs) or collagen (for human SMCs) to promote cell adhesion. Cells were harvested with trypsin and ethylenediamine tetraacetic acid, washed with 1 mg/ml bovine serum albumin in DMEM, counted using a hemocytometer, and resuspended at a concentration of 120,000 cells/ml in 1 mg/ml bovine serum albumin in DMEM. The bottom wells of the Boyden chamber were filled with 0.5 to 500 ng/ml HGF/SF, 10 nmol/L PDGF, or DMEM/1 mg/ml bovine serum albumin as a negative control. The chamber was assembled with a filter and cells were added to the top wells. Chambers were incubated at 37°C for 6 hours, before migrated cells were visualized using a DiffQuick staining system (Gamidor Ltd., Abingdon Oxfordshire, UK) and counted under the microscope.
Immunofluorescence and Immunohistochemistry
Subconfluent cells plated on fibronectin-coated glass slides were fixed in ice-cold acetone for 5 minutes, air-dried, and washed in PBS before blocking nonspecific binding for 15 minutes in Protein Block (X0909; DAKO, Carpinteria, CA). Cells were incubated in 50 μg/ml 1W66 or × μg/ml anti-MET antibody for 1 hour at 37°C, washed in PBS, and incubated for another hour at 37°C in anti-sheep or anti-rabbit fluorescein isothiocyanate-conjugated secondary antibody, respectively. Cells were counterstained with propidium iodide and aqueous-mounted before examination with appropriate filters using a fluorescence microscope. Specificity of staining with the 1W66 antibody was confirmed by assessing its reactivity with cell lines known to express (or fail to express). For immunofluorescence of tissue sections, arteries were snap-frozen, mounted in OCT, and 10-mm sections were cut using a cryostat. Sections were fixed in acetone at −20°C for 10 minutes, air-dried, and processed as above.
In Vivo Injury Models
For balloon injury, 300-g rats were anesthetized and a 2-cm longitudinal midline incision was made through the skin. The left external carotid artery was located using blunt dissection and ligated distally, while proximally the artery was held with an untied ligature. A small hole was made in the vessel and a 2-French Fogarty balloon catheter inserted into the vessel and down to the aortic arch. Balloon injury of the common carotid artery was performed by three passes of the partially inflated balloon before the proximal ligature on the external carotid artery was ligated and the skin wound sutured.
For defined filament injury, rats were anesthetized and the external carotid artery located as described for balloon injury; however, in this case a 0.25-mm filament with a curved end, and housed retracted in a section of PE10 tubing, was inserted into the vessel. Once the end of the injury device had reached the aortic arch, the curved end of the filament was pushed out and the device pulled out of the vessel, with the aim of causing a single track of endothelial denudation approximately one third of the width of the opened out vessel, along the length of the common carotid artery. The external carotid artery was then tied off. The rat was then placed on its stomach and an area of the shoulder blades was shaved and swabbed before a 2-cm skin incision was made. Blunt dissection was used to create a skin pocket large enough to insert a 2-ml osmotic minipump filled with 3 mg/ml of human HGF/SF (hHGF/SF) in 20 mmol/L Tris-HCl and 0.5 mol/L NaCl, pH 7.6, buffer or buffer alone. The dosing schedule for hHGF/SF was determined in pilot studies. The tubing from the minipump was passed under the skin and cannulated into the right jugular vein and all skin wounds were sutured. Seventeen hours before termination, rats were dosed with a bromodeoxyuridine (BrdU) tablet. Rats were killed by suffocation in a rising concentration of carbon dioxide, perfused with Krebs buffer via the abdominal aorta, and the carotid arteries gently removed by dissection. Arteries were opened longitudinally, and pinned luminal side up for en face immunohistochemical staining for BrdU expression with diaminobenzidine substrate.
ApoE−/− Mice
The ApoE−/− mice were a kind gift of C. Long (Pfizer Central Research, Sandwich, UK) via Charles River Laboratories (Wilmington, MA). The mice were rederived onto a 129ola × C57BL/6 × BALB/c background and genotyped by Charles River. Mice were weaned at the age of 4 weeks, fed a normal chow diet for 1 week before being given a high-fat diet as described by Nakashima and colleagues.51 For histology and histochemistry, arteries that had been perfusion-fixed (40 g/L phosphate-buffered paraformaldehyde) were cut transversely into three to four pieces, fixed overnight, washed in saline, and paraffin-embedded. Sections (5 μm) were cut and mounted onto Vectabond (SP1800; Vector, Burlingame, CA). For HGF/SF and MET immunohistochemistry, paraffin-embedded sections were stained with primary antibodies as described above followed by biotinylated secondary antibodies and avidin-biotin reagent (SC-2018; Santa Cruz Biotechnology) before diaminobenzidine substrate. In addition to staining for HGF/SF and MET, sections were also stained for α-smooth muscle actin and for the macrophage marker CD68.
Results
Expression of HGF/SF and MET in SMCs and ECs
Early passage cultures of rat aortic ECs, SMCs, and adventitial fibroblasts were studied initially for expression of HGF/SF by immunofluorescence, Western blot, and biological activity on MDCK colonies, and for MET by immunofluorescence. Adventitial fibroblasts expressed HGF/SF and did not respond to the factor. The behavior of these cells, therefore, appeared to be typical of fibroblast isolates from other tissues13 and was not investigated further.
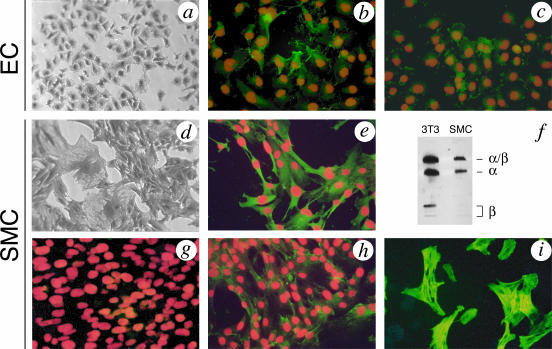
Figure 1, a and d, shows the appearance of typical EC and SMC cultures from rat aorta. A number of ECs expressed HGF/SF, as shown by green fluorescence with the 1W66 anti-mouse HGF/SF polyclonal antibody (Figure 1b) and secretion of MDCK colony-dispersing activity (data not shown). Expression was not homogenous throughout the cell population, with some cells showing more intense fluorescence than others (Figure 1b). As expected, ECs expressed the MET receptor (Figure 1c). SMCs showed strong expression of HGF/SF (Figure 1e), and the SMC-derived factor was indistinguishable from the factor originally isolated from a 3T3 line in terms of activity on MDCK cells (data not shown) and protein (Figure 1f). In agreement with a previous report,39 confluent cultures of SMCs did not express the MET receptor (Figure 1g). However, if such cultures were wounded (see below), the migrating cells at the wound edge showed strong MET expression (Figure 1h). These cells stained for α-smooth muscle actin (Figure 1i), indicating that they were bona fide SMCs that acquired MET expression in the transition from a stationary to a migrating phenotype.
Figure 1.
Expression of HGF/SF and MET in ECs and SMCs. Phase contrast image (a) and expression of HGF/SF (b) or MET (c) by immunofluorescence in subconfluent cultures of rat ECs. Phase contrast image (d) and expression of HGF/SF in SMCs by immunofluorescence (e) or Western blot (f). Both ECs (b) and SMCs (e) express HGF/SF but expression in ECs is weaker and not homogenous; in contrast, SMCs show strong and homogeneous expression of HGF/SF. f: The HGF/SF protein secreted by SMC cultures is indistinguishable from the protein isolated from a 3T3 line.14 g and h: Expression of MET in SMCs. Confluent cultures of SMCs do not express MET (g) but SMCs migrating at the edge of a scrape injury (as shown in Figure 2) show clear, positive staining for MET (h). i: MET-expressing cells from SMC cultures are positive for α-smooth muscle actin. Immunofluorescence of HGF/SF or MET is demonstrated by green fluorescence with nuclear counterstain in red.
HGF/SF Causes Migration and Growth of SMCs
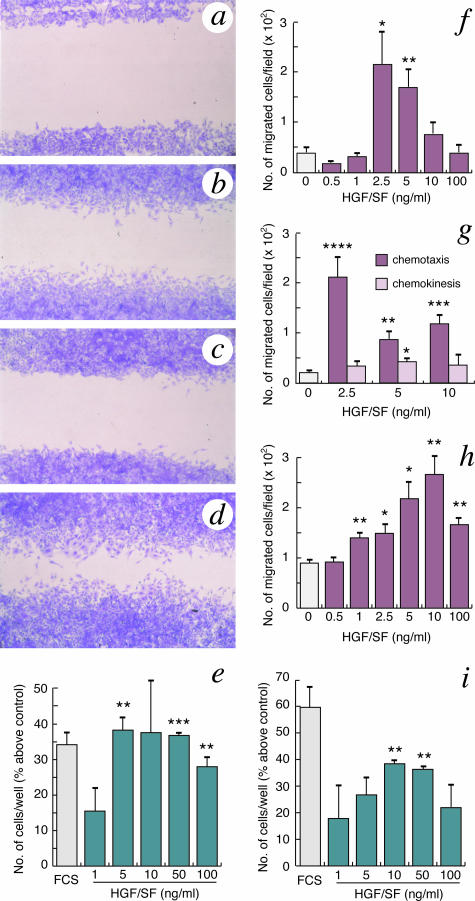
To clarify the functional role, if any, of MET expression in SMCs, a series of experiments was performed in which the response of these cells to HGF/SF was assessed in terms of wound recovery (Figure 2, a–d), growth (Figure 2e), and motility stimulation on individual cells (Figure 2, f–h). Figure 2a shows a control culture in basal medium 24 hours after wounding. The culture shows little regrowth in the free area compared to parallel cultures in 5% FCS (Figure 2b). HGF/SF alone induced regrowth at a level comparable with that of 5% FCS (Figure 2c) and considerably enhanced the regrowth caused by 5% FCS (Figure 2d). HGF/SF also increased SMC growth (cell number) in scrape-injured cultures to the same level achieved by 10% FCS (Figure 2e). This effect on SMC proliferation after injury was more potent than the one induced on scrape-injured EC cultures (Figure 2i). A direct effect of HGF/SF on SMC motility was next assessed in Boyden chamber assays. HGF/SF induced a dramatic motility response (Figure 2f) that resulted primarily from stimulation of directional (chemotactic) rather than random (chemokinetic) cell movement (Figure 2g). Human SMCs also exhibited a strong motility response to HGF/SF demonstrating that the effect of HGF/SF on SMCs translates across species (Figure 2h). Thus, the MET expression observed in scrape-injured cultures (Figure 1h) induces a strong migratory (Figure 2, c, d, and f–h) and growth (Figure 2d) response to HGF/SF in SMCs, raising the possibility of a much broader role of HGF/SF in arterial repair than previously postulated. This hypothesis was tested next through a series of expression and functional studies in vivo.
Figure 2.
HGF/SF induces cell migration and proliferation in SMCs. Regrowth of SMCs in response to HGF/SF was assessed 24 hours after scrape injury in the presence of 0.05% FCS (a), 5% FCS (b), 0.05% FCS + 2.5 ng/ml HGF/SF (c), or 5% FCS + 2.5 ng/ml HGF/SF (d). Both FCS and HGF/SF induce SMC migration and their activity is additive (compare d with b and c). e: HGF/SF induces proliferation of SMCs 24 hours after scrape injury. Data are shown for cultures in 10% FCS or 0.05% FCS + 1−100 ng/ml mHGF/SF. The effect of HGF/SF on SMC proliferation is comparable with that on ECs (i). HGF/SF induces migration of rat (f and g) and human (h) SMCs in Boyden chamber assays. The strong migratory response of rat SMCs to HGF/SF is due predominantly to chemotactic rather than chemokinetic activity (g). The experiments shown in e–i are the mean ± SEM from four wells. Statistical significance was represented at P < 0.05 (*), P < 0.01 (**), P < 0.001 (***), and P < 0.0001 (****).
HGF/SF and MET in Arterial Repair in Vivo
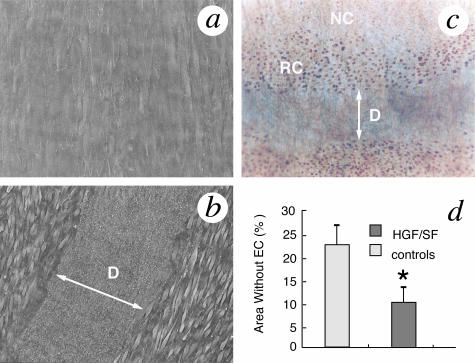
Figure 3 shows that HGF/SF promotes re-endothelialization after a defined filament injury in the rat carotid artery. Figure 3, a and b, show electron micrographs of the en face surface of uninjured (Figure 3a) and injured (Figure 3b) rat carotid arteries. The injury results in endothelial denudation and platelet adhesion and aggregation but no damage to the underlying internal elastic lamina and media layer. Forty-eight hours after injury, the ECs surrounding the denuded area migrated and proliferated (as shown by brown nuclear staining resulting from the incorporation of BrdU into DNA replicating cells (Figure 3c). Nonreplicating ECs farther away from the lesion only showed background staining (Figure 3c). Infusion of recombinant HGF/SF after injury induced a strong growth and migratory response in the ECs that resulted in a marked decrease in the area denuded of endothelium (Figure 3d).
Figure 3.
HGF/SF promotes re-endothelialization in the rat carotid artery after superficial, scrape injury in vivo. Electron micrographs of the en face surface of uninjured (a) and injured (b) rat carotid arteries. The scrape injury causes denudation (D) and platelet adhesion and aggregation but no damage to the underlying internal elastic lamina and media layers. c: Replicating cells (RCs) in the endothelium adjacent to the scrape injury are visualized by BrdU incorporation into DNA and shown as brown coloration under the light microscope. Nonreplicating (NR) ECs further away from the injury only show background staining. d: The en face area of the artery without ECs (labeled with NC), is compared in control and HGF/SF-treated rats 48 hours after injury and expressed as a percentage of the total en face area of each artery. Data are mean ± SEM from seven rats per group. Statistical significance is represented at P < 0.05 (*).
The involvement of HGF/SF in the repair of deeper arterial injuries that cause damage to the media layer and migration and proliferation of SMCs was investigated next. For this, balloon injuries were produced and the expression of HGF/SF and MET in the artery was studied throughout the arterial repair reaction. Expression of HGF/SF in vivo in uninjured carotid arteries was confined to lumen-lining cells (ECs) and to certain areas of the adventitia (A) but was barely detectable in the media of uninjured arteries (Figure 4a). Fourteen days after a deep arterial injury, a thick neointima develops containing a large number of SMCs migrated from the media and undergoing mitosis and extensive synthesis of the extracellular matrix.3,4 The SMCs of the neointima showed dramatic expression of both HGF/SF (Figure 4c) and MET (Figure 4d), and a time course of HGF/SF protein indicated striking changes, namely initial conversion of pro-HGF/SF (αβ) to two chains HGF/SF (α) followed by neo synthesis (days 2, 4, and 7 after injury) and further activation (Figure 4e). Expression of MET was also markedly up-regulated after injury (Figure 4, d and f). These findings, together with the SMC response to HGF/SF in culture (Figure 2), imply a critical role for HGF/SF and MET in SMC migration and arterial remodeling after deep mechanical injury.
Figure 4.
Expression of HGF/SF and MET in rat carotid arteries after deep (balloon) injury. Expression is demonstrated by green fluorescence for HGF/SF and red fluorescence for MET. HGF/SF immunofluorescence is detected only in lumen-lining cells and in certain areas of the adventitia (A) in uninjured arteries (a) whereas 14 days after injury striking expression of HGF/SF is observed in the newly developed intima and also in SMCs of the underlying media (c). MET immunofluorescence is undetectable in uninjured arteries (b), but very strong in the cells of the neointima 14 days after injury (d). Time course of expression of HGF/SF (e) and MET (f) in rat carotid arteries with no injury or 1, 2, 4, 7, and 14 days after injury. Injury first causes conversion of pro-HGF/SF (αβ) to active, two-chain HGF/SF (α chain is shown) followed by new synthesis of pro-HGF/SF and the subsequent activation. The Western blots are representative of three separate balloon injury experiments.
HGF/SF and MET in Atherogenesis
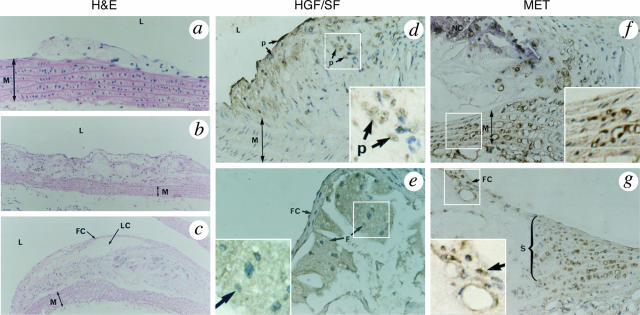
Endothelial damage and migration of SMCs from the media to the neointima are features of both arterial remodeling after mechanical injury and atherogenesis. Atherosclerotic lesions, however, are characterized by additional processes, such as lipid deposition, and the presence of a third and critical cell type, namely the monocyte-derived macrophage.2 We analyzed the expression of HGF/SF and MET during atherogenesis in the apoE−/− mouse, a model of atherogenesis that closely resembles the development and progression of human lesions.38 Figure 5, a, b, and c, show typical early, intermediate, and advanced lesions in such mice and, noticeably, the presence of a typical fibrous cap and lipid core in the advanced lesion similar to those of human lesions (Figure 5c). Expression of HGF/SF in the arterial lesions of apoE−/− mice occurred in lumen-lining cells and in foam cells within the lesions (Figure 5, d and e). These foam cells expressed CD68 and lacked expression of α-smooth muscle actin (data not shown); they were therefore HGF/SF-expressing macrophage-derived foam cells. In contrast, MET expression was strong in SMCs surrounding and entering the lesions, namely in the underlying media (Figure 5f), the shoulder region and the fibrous cap (Figure 5g). In summary, in the arterial lesions of apoE−/− mice, HGF/SF is expressed predominantly in macrophage-derived foam cells in the central area of the lesions whereas MET is expressed in SMCs at the periphery of and underneath the lesion.
Figure 5.
Expression of HGF/SF and MET in atherosclerotic lesions of apoE−/− mice. a–c: Lesion development is shown in H&E staining of transverse sections of the aortic arch. a: A small lesion protruding in the lumen (L) and without involvement of the media (M) layer. b: A more complex lesion resulting in extensive intimal thickening, lipid deposition, and stenosis. c: An advanced lesion with a typical fibrous cap (FC), lipid core (LC), and a severely compromised lumen. Extensive lipid deposition is seen in the underlying media as well. d and e: Strong, positive (p) expression of HGF/SF in cells bordering the lumen (d) and in monocyte-derived foam cells (F) of advanced lesions (e). f and g: Expression of MET in the media (f) and in SMC-rich, shoulder (S) regions of advanced lesions (g). Insets show higher magnification views of the areas delimited by squares.
Discussion
This study presents data that define new, major roles for HGF/SF and MET in vascular physiology and pathology and explain previous inconsistencies in the literature on the SMC response to HGF/SF. The experiments confirm that SMCs in culture produce HGF/SF (Figure 1, e and f), and that ECs express the MET receptor (Figure 1c) and respond to HGF/SF (Figure 2i), in line with earlier reports.34,39–42 The study thus supports a paracrine role for SMC-derived HGF/SF on vascular ECs in normal, adult arteries but also suggests novel roles for HGF/SF and MET in SMC-dependent arterial remodeling and atherogenesis after injury.
Injury Induces MET Expression in SMCs in Vitro and in Vivo
Although SMCs in culture express HGF/SF (Figure 1, e and f), expression by SMCs in vivo in uninjured arteries is barely detectable (Figure 3a). Thus the HGF/SF gene is one of several genes that become transcriptionally activated in SMCs during the phenotypic transition that occurs in culture.39 In vitro expression of HGF/SF in SMCs is not influenced by cell density or injury and appears constitutive. Expression of MET in SMCs, like HGF/SF, is undetectable in vivo in uninjured arteries (Figure 3b). However, in vitro, MET expression is remarkably regulated, being negligible in confluent cultures (Figure 1g), low in sparse cultures (data not shown), and high after scrape injury in cells at the leading edge of the wound (Figure 1h). Further, these MET-positive SMCs show a potent response to HGF/SF (Figure 2, c–h).
The pattern of expression of HGF/SF and MET during arterial remodeling after deep balloon injury confirmed that injury causes a dramatic increase in HGF/SF in vivo (Figure 4, c and e) and that the SMCs that migrated from the media to the neointima express MET (Figure 4d). Thus, HGF/SF appears to be critically involved in the SMC’s response to injury. The signals responsible for activation of the MET gene in SMCs after injury remain to be established, but the fact that the transition from a MET− to a MET+ phenotype can be achieved in vitro in scrape-injured cultures suggests ways in which such signal(s) may be examined, for example by microarray experiments.
HGF/SF and MET in Atherogenesis
There is now broad agreement that atherosclerosis constitutes an inflammatory response of the arterial wall to chronic injury. This “response to injury” hypothesis, first proposed in the 19th century by Rudolf Virchow,52 has been strongly advocated and extended by Russell Ross1–4 throughout the last 3 decades and is now widely accepted.5 Endothelial injury is thought to be a key, and possibly initiating feature, of early lesion development.53 Whereas small areas of an endothelial injury may be repaired without disease progression,54 chronic damage to the endothelium leads to platelet adhesion and aggregation and to macrophage recruitment. This, in turn, elicits SMC migration to the intima and the development of advanced lesions.
Platelets were one of several original sources of HGF/SF,55 along with macrophages in several tissues.56,57 Interestingly, HGF/SF expression by liver macrophages is essential for a full regenerative response of hepatocytes after injury.58 We propose that a similar course of events occurs in the arterial wall where HGF/SF is expressed in macrophage-derived foam cells in atherosclerotic lesions of apoE−/− mice (Figure 5, d and e) and MET is expressed in neighboring SMCs (Figure 5, f and g). Expression of HGF/SF has also been reported in macrophages in human arterial lesions.59,60 Thus, macrophage-derived HGF/SF may act as a key chemoattractant and mitogen for SMCs in atherogenesis and platelets (Figure 3b) and/or ECs (Figure 1b) may constitute additional sources of the factor. In contrast, in the macrophage- and EC-free lesions caused by deep mechanical injury (Figure 4), platelets may constitute the primary local source of HGF/SF in the subendothelium.
The finding that SMCs are a key target of HGF/SF in arterial injury and atherogenesis has implications for the clinical use of HGF/SF in vascular disease. It is widely accepted that endothelial integrity and repair prevents lesion development while SMC migration and proliferation in the intima are typical features of advanced lesions.2 HGF/SF promotes endothelial repair (Figure 3) but appears to be equally and critically involved in the SMC response (Figures 4 and 5). We argue that endothelial repair, on the one hand, and SMC migration and proliferation, on the other, are complementary aspects and stages of the arterial response to injury. From an evolutionary view point we believe it should be no surprise that the same signaling system may be involved in both processes. This, however, has interesting implications for both diagnosis and therapy of arterial disease.
There is probably no clinical counterpart to the localized, superficial endothelial injury illustrated in Figure 3b, whose repair is greatly enhanced by HGF/SF (Figure 3d). Chronic endothelial damage however, with or without cell loss, is probably critical for lesion formation and for SMC activation. Our data suggest that activated SMCs express MET and may migrate toward a source of HGF/SF in the endothelial or subendothelial area. We are aware of data indicating that HGF/SF reduces intimal thickening in balloon-injured rabbit arteries.61 Further studies will be required, however, to establish complete role of HGF/SF and MET in atherogenesis, and we suggest that mouse models in which the HGF/SF or MET genes are overexpressed or ablated in either the SMC or EC lineages may contribute considerably.
Footnotes
Address reprint requests to Ermanno Gherardi, MRC Centre, Hills Rd., Cambridge CB2 2QH, UK. E-mail: egherard@mrc-lmb.cam.ac.uk.
Supported by a research studentship (H.M.) and a program grant (E.G.) from the Medical Research Council of the United Kingdom; and a grant from the National Institutes of Health, Bethesda, MD (NIH-HL070858 to M.R.).
References
- Ross R. The pathogenesis of atherosclerosis: an update. N Engl J Med. 1986;314:488–500. doi: 10.1056/NEJM198602203140806. [DOI] [PubMed] [Google Scholar]
- Ross R. Atherosclerosis: an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- Ross R, Glomset JA. The pathogenesis of atherosclerosis (first of two parts). N Engl J Med. 1976;295:369–377. doi: 10.1056/NEJM197608122950707. [DOI] [PubMed] [Google Scholar]
- Ross R, Glomset JA. The pathogenesis of atherosclerosis (second of two parts). N Engl J Med. 1976;295:420–425. doi: 10.1056/NEJM197608192950805. [DOI] [PubMed] [Google Scholar]
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- Jawien A, Bowen-Pope DF, Lindner V, Schwartz SM, Clowes AW. Platelet-derived growth factor promotes smooth muscle migration and intimal thickening in a rat model of balloon angioplasty. J Clin Invest. 1992;89:507–511. doi: 10.1172/JCI115613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferns GA, Raines EW, Sprugel KH, Motani AS, Reidy MA, Ross R. Inhibition of neointimal smooth muscle accumulation after angioplasty by an antibody to PDGF. Science. 1991;253:1129–1132. doi: 10.1126/science.1653454. [DOI] [PubMed] [Google Scholar]
- Banai S, Wolf Y, Golomb G, Pearle A, Waltenberger J, Fishbein I, Schneider A, Gazit A, Perez L, Huber R, Lazarovichi G, Rabinovich L, Levitzki A, Gertz SD. PDGF-receptor tyrosine kinase blocker AG1295 selectively attenuates smooth muscle cell growth in vitro and reduces neointimal formation after balloon angioplasty in swine. Circulation. 1998;97:1960–1969. doi: 10.1161/01.cir.97.19.1960. [DOI] [PubMed] [Google Scholar]
- Jackson CL, Reidy MA. Basic fibroblast growth factor: its role in the control of smooth muscle cell migration. Am J Pathol. 1993;143:1024–1031. [PMC free article] [PubMed] [Google Scholar]
- Miyazawa K, Tsubouchi H, Naka D, Takahashi K, Okigaki M, Arakaki N, Nakayama H, Hirono S, Sakiyama O, Takahashi K, Gohda E, Daikuhara Y, Kitamura N. Molecular cloning and sequence analysis of cDNA for human hepatocyte growth factor. Biochem Biophys Res Commun. 1989;163:967–973. doi: 10.1016/0006-291x(89)92316-4. [DOI] [PubMed] [Google Scholar]
- Nakamura T, Nishizawa T, Hagiya M, Seki T, Shimonishi M, Sugimura A, Tashiro K, Shimizu S. Molecular cloning and expression of human hepatocyte growth factor. Nature. 1989;342:440–443. doi: 10.1038/342440a0. [DOI] [PubMed] [Google Scholar]
- Zarnegar R, Michalopoulos G. Purification and biological characterization of human hepatopoietin A, a polypeptide growth factor for hepatocytes. Cancer Res. 1989;49:3314–3320. [PubMed] [Google Scholar]
- Stoker M, Gherardi E, Perryman M, Gray J. Scatter factor is a fibroblast-derived modulator of epithelial cell mobility. Nature. 1987;327:239–242. doi: 10.1038/327239a0. [DOI] [PubMed] [Google Scholar]
- Gherardi E, Gray J, Stoker M, Perryman M, Furlong R. Purification of scatter factor, a fibroblast-derived basic protein that modulates epithelial interactions and movement. Proc Natl Acad Sci USA. 1989;86:5844–5848. doi: 10.1073/pnas.86.15.5844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottaro DP, Rubin JS, Faletto DL, Chan AM, Kmiecik TE, Vande Woude GF, Aaronson SA. Identification of the hepatocyte growth factor receptor as the c-met proto-oncogene product. Science. 1991;251:802–804. doi: 10.1126/science.1846706. [DOI] [PubMed] [Google Scholar]
- Naldini L, Weidner KM, Vigna E, Gaudino G, Bardelli A, Ponzetto C, Narsimhan RP, Hartmann G, Zarnegar R, Michalopoulos GK, Birchmeierl W, Comoglio PM. Scatter factor and hepatocyte growth factor are indistinguishable ligands for the MET receptor. EMBO J. 1991;10:2867–2878. doi: 10.1002/j.1460-2075.1991.tb07836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han S, Stuart LA, Degen SJ. Characterization of the DNF15S2 locus on human chromosome 3: identification of a gene coding for four kringle domains with homology to hepatocyte growth factor. Biochemistry. 1991;30:9768–9780. doi: 10.1021/bi00104a029. [DOI] [PubMed] [Google Scholar]
- Yoshimura T, Yuhki N, Wang MH, Skeel A, Leonard EJ. Cloning, sequencing, and expression of human macrophage stimulating protein (MSP, MST1) confirms MSP as a member of the family of kringle proteins and locates the MSP gene on chromosome 3. J Biol Chem. 1993;268:15461–15468. [PubMed] [Google Scholar]
- Donate LE, Gherardi E, Srinivasan N, Sowdhamini R, Aparicio S, Blundell TL. Molecular evolution and domain structure of plasminogen-related growth factors (HGF/SF and HGF1/MSP). Protein Sci. 1994;3:2378–2394. doi: 10.1002/pro.5560031222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naldini L, Tamagnone L, Vigna E, Sachs M, Hartmann G, Birchmeier W, Daikuhara Y, Tsubouchi H, Blasi F, Comoglio PM. Extracellular proteolytic cleavage by urokinase is required for activation of hepatocyte growth factor/scatter factor. EMBO J. 1992;11:4825–4833. doi: 10.1002/j.1460-2075.1992.tb05588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars WM, Zarnegar R, Michalopoulos GK. Activation of hepatocyte growth factor by the plasminogen activators uPA and tPA. Am J Pathol. 1993;143:949–958. [PMC free article] [PubMed] [Google Scholar]
- Miyazawa K, Shimomura T, Kitamura A, Kondo J, Morimoto Y, Kitamura N. Molecular cloning and sequence analysis of the cDNA for a human serine protease responsible for activation of hepatocyte growth factor: structural similarity of the protease precursor to blood coagulation factor XII. J Biol Chem. 1993;268:10024–10028. [PubMed] [Google Scholar]
- Bladt F, Riethmacher D, Isenmann S, Aguzzi A, Birchmeier C. Essential role for the c-met receptor in the migration of myogenic precursor cells into the limb bud [see comments]. Nature. 1995;376:768–771. doi: 10.1038/376768a0. [DOI] [PubMed] [Google Scholar]
- Schmidt C, Bladt F, Goedecke S, Brinkmann V, Zschiesche W, Sharpe M, Gherardi E, Birchmeier C. Scatter factor/hepatocyte growth factor is essential for liver development. Nature. 1995;373:699–702. doi: 10.1038/373699a0. [DOI] [PubMed] [Google Scholar]
- Uehara Y, Minowa O, Mori C, Shiota K, Kuno J, Noda T, Kitamura N. Placental defect and embryonic lethality in mice lacking hepatocyte growth factor/scatter factor. Nature. 1995;373:702–705. doi: 10.1038/373702a0. [DOI] [PubMed] [Google Scholar]
- Borowiak M, Garratt AN, Wustefeld T, Strehle M, Trautwein C, Birchmeier C. Met provides essential signals for liver regeneration. Proc Natl Acad Sci USA. 2004;101:10608–10613. doi: 10.1073/pnas.0403412101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh CG, Factor VM, Sanchez A, Uchida K, Conner EA, Thorgeirsson SS. Hepatocyte growth factor/c-met signaling pathway is required for efficient liver regeneration and repair. Proc Natl Acad Sci USA. 2004;101:4477–4482. doi: 10.1073/pnas.0306068101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujiwara K, Nagoshi S, Ohno A, Hirata K, Ohta Y, Mochida S, Tomiya T, Higashio K, Kurokawa K. Stimulation of liver growth by exogenous human hepatocyte growth factor in normal and partially hepatectomized rats. Hepatology. 1993;18:1443–1449. [PubMed] [Google Scholar]
- Burr AW, Toole K, Chapman C, Hines JE, Burt AD. Anti-hepatocyte growth factor antibody inhibits hepatocyte proliferation during liver regeneration. J Pathol. 1998;185:298–302. doi: 10.1002/(SICI)1096-9896(199807)185:3<298::AID-PATH88>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- Kawaida K, Matsumoto K, Shimazu H, Nakamura T. Hepatocyte growth factor prevents acute renal failure and accelerates renal regeneration in mice. Proc Natl Acad Sci USA. 1994;91:4357–4361. doi: 10.1073/pnas.91.10.4357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohmichi H, Matsumoto K, Nakamura T. In vivo mitogenic action of HGF on lung epithelial cells: pulmotrophic role in lung regeneration. Am J Physiol. 1996;270:L1031–L1039. doi: 10.1152/ajplung.1996.270.6.L1031. [DOI] [PubMed] [Google Scholar]
- Nakamura T, Mizuno S, Matsumoto K, Sawa Y, Matsuda H. Myocardial protection from ischemia/reperfusion injury by endogenous and exogenous HGF. J Clin Invest. 2000;106:1511–1519. doi: 10.1172/JCI10226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen EM, Goldberg ID, Kacinski BM, Buckholz T, Vinter DW. Smooth muscle releases an epithelial cell scatter factor which binds to heparin. In Vitro Cell Dev Biol. 1989;25:163–173. doi: 10.1007/BF02626174. [DOI] [PubMed] [Google Scholar]
- Rosen EM, Carley W, Goldberg ID. Scatter factor regulates vascular endothelial cell motility. Cancer Invest. 1990;8:647–650. doi: 10.3109/07357909009018936. [DOI] [PubMed] [Google Scholar]
- Van Belle E, Witzenbichler B, Chen D, Silver M, Chang L, Schwall R, Isner JM. Potentiated angiogenic effect of scatter factor/hepatocyte growth factor via induction of vascular endothelial growth factor: the case for paracrine amplification of angiogenesis. Circulation. 1998;97:381–390. doi: 10.1161/01.cir.97.4.381. [DOI] [PubMed] [Google Scholar]
- Sengupta S, Sellers LA, Cindrova T, Skepper J, Gherardi E, Sasisekharan R, Fan TP. Cyclooxygenase-2-selective nonsteroidal anti-inflammatory drugs inhibit hepatocyte growth factor/scatter factor-induced angiogenesis. Cancer Res. 2003;63:8351–8359. [PubMed] [Google Scholar]
- Sengupta S, Sellers LA, Li RC, Gherardi E, Zhao G, Watson N, Sasisekharan R, Fan TP. Targeting of mitogen-activated protein kinases and phosphatidylinositol 3 kinase inhibits hepatocyte growth factor/scatter factor-induced angiogenesis. Circulation. 2003;107:2955–2961. doi: 10.1161/01.CIR.0000077501.19266.E5. [DOI] [PubMed] [Google Scholar]
- Sengupta S, Gherardi E, Sellers LA, Wood JM, Sasisekharan R, Fan TP. Hepatocyte growth factor/scatter factor can induce angiogenesis independently of vascular endothelial growth factor. Arterioscler Thromb Vasc Biol. 2003;23:69–75. doi: 10.1161/01.atv.0000048701.86621.d0. [DOI] [PubMed] [Google Scholar]
- Bussolino F, Di Renzo MF, Ziche M, Bocchietto E, Olivero M, Naldini L, Gaudino G, Tamagnone L, Coffer A, Comoglio PM. Hepatocyte growth factor is a potent angiogenic factor which stimulates endothelial cell motility and growth. J Cell Biol. 1992;119:629–641. doi: 10.1083/jcb.119.3.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant DS, Kleinman HK, Goldberg ID, Bhargava MM, Nickoloff BJ, Kinsella JL, Polverini P, Rosen EM. Scatter factor induces blood vessel formation in vivo. Proc Natl Acad Sci USA. 1993;90:1937–1941. doi: 10.1073/pnas.90.5.1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura Y, Morishita R, Higaki J, Kida I, Aoki M, Moriguchi A, Yamada K, Hayashi S, Yo Y, Matsumoto K, Nakamura T, Ogihara T. Expression of local hepatocyte growth factor system in vascular tissues. Biochem Biophys Res Commun. 1995;215:483–488. doi: 10.1006/bbrc.1995.2490. [DOI] [PubMed] [Google Scholar]
- Nakamura Y, Morishita R, Higaki J, Kida I, Aoki M, Moriguchi A, Yamada K, Hayashi S, Yo Y, Nakano H, Matsumoto K, Nakamura T, Ogihara T. Hepatocyte growth factor is a novel member of the endothelium-specific growth factors: additive stimulatory effect of hepatocyte growth factor with basic fibroblast growth factor but not with vascular endothelial growth factor. J Hypertens. 1996;14:1067–1072. doi: 10.1097/00004872-199609000-00004. [DOI] [PubMed] [Google Scholar]
- Rosen EM, Laterra J, Joseph A, Jin L, Fuchs A, Way D, Witte M, Weinand M, Goldberg ID. Scatter factor expression and regulation in human glial tumors. Int J Cancer. 1996;67:248–255. doi: 10.1002/(SICI)1097-0215(19960717)67:2<248::AID-IJC16>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Ma H, Calderon TM, Kessel T, Ashton AW, Berman JW. Mechanisms of hepatocyte growth factor-mediated vascular smooth muscle cell migration. Circ Res. 2003;93:1066–1073. doi: 10.1161/01.RES.0000102867.54523.7F. [DOI] [PubMed] [Google Scholar]
- Taher TE, Derksen PW, de Boer OJ, Spaargaren M, Teeling P, van der Wal AC, Pals ST. Hepatocyte growth factor triggers signaling cascades mediating vascular smooth muscle cell migration. Biochem Biophys Res Commun. 2002;298:80–86. doi: 10.1016/s0006-291x(02)02397-5. [DOI] [PubMed] [Google Scholar]
- Walter JJ, Sane DC. Angiostatin binds to smooth muscle cells in the coronary artery and inhibits smooth muscle cell proliferation and migration in vitro. Arterioscler Thromb Vasc Biol. 1999;19:2041–2048. doi: 10.1161/01.atv.19.9.2041. [DOI] [PubMed] [Google Scholar]
- Rosen EM, Goldberg ID. Regulation of angiogenesis by scatter factor. EXS. 1997;79:193–208. doi: 10.1007/978-3-0348-9006-9_8. [DOI] [PubMed] [Google Scholar]
- Aoyagi M, Yamamoto S, Azuma H, Yamamoto M, Tamaki M, Niimi Y, Hirakawa K, Yamamoto K. Localization and effects of hepatocyte growth factor on smooth muscle cells during neointimal formation after balloon denudation. Histochem Cell Biol. 1999;111:419–428. doi: 10.1007/s004180050377. [DOI] [PubMed] [Google Scholar]
- McMurray HF, Parrott DP, Bowyer DE. A standardised method of culturing aortic explants, suitable for the study of factors affecting the phenotypic modulation, migration and proliferation of aortic smooth muscle cells. Atherosclerosis. 1991;86:227–237. doi: 10.1016/0021-9150(91)90219-s. [DOI] [PubMed] [Google Scholar]
- Bornfeldt KE, Raines EW, Nakano T, Graves LM, Krebs EG, Ross R. Insulin-like growth factor-I and platelet-derived growth factor-BB induce directed migration of human arterial smooth muscle cells via signaling pathways that are distinct from those of proliferation. J Clin Invest. 1994;93:1266–1274. doi: 10.1172/JCI117081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakashima Y, Plump AS, Raines EW, Breslow JL, Ross R. ApoE-deficient mice develop lesions of all phases of atherosclerosis throughout the arterial tree. Arterioscler Thromb. 1994;14:133–140. doi: 10.1161/01.atv.14.1.133. [DOI] [PubMed] [Google Scholar]
- Virchow R. Virchow R, editor. Frankfurt: Von Meidinger Sohn; Phlogose und thrombose in geraβsystem. Gesammelte Abhandlungen zur Wissenchaftichen Medicin. 1856:pp 458–521. [Google Scholar]
- Ross R, Harker L. Platelets, endothelium, and smooth muscle cells in atherosclerosis. Adv Exp Med Biol. 1978;102:135–141. doi: 10.1007/978-1-4757-1217-9_8. [DOI] [PubMed] [Google Scholar]
- Reidy MA, Schwartz SM. Endothelial regeneration: III. Time course of intimal changes after small defined injury to rat aortic endothelium. Lab Invest. 1981;44:301–308. [PubMed] [Google Scholar]
- Nakamura T, Nawa K, Ichihara A, Kaise N, Nishino T. Purification and subunit structure of hepatocyte growth factor from rat platelets. FEBS Lett. 1987;224:311–316. doi: 10.1016/0014-5793(87)80475-1. [DOI] [PubMed] [Google Scholar]
- Noji S, Tashiro K, Koyama E, Nohno T, Ohyama K, Taniguchi S, Nakamura T. Expression of hepatocyte growth factor gene in endothelial and Kupffer cells of damaged rat livers, as revealed by in situ hybridization. Biochem Biophys Res Commun. 1990;173:42–47. doi: 10.1016/s0006-291x(05)81018-6. [DOI] [PubMed] [Google Scholar]
- Yamada T, Hisanaga M, Nakajima Y, Mizuno S, Matsumoto K, Nakamura T, Nakano H. Enhanced expression of hepatocyte growth factor by pulmonary ischemia-reperfusion injury in the rat. Am J Respir Crit Care Med. 2000;162:707–715. doi: 10.1164/ajrccm.162.2.9908064. [DOI] [PubMed] [Google Scholar]
- Takeishi T, Hirano K, Kobayashi T, Hasegawa G, Hatakeyama K, Naito M. The role of Kupffer cells in liver regeneration. Arch Histol Cytol. 1999;62:413–422. doi: 10.1679/aohc.62.413. [DOI] [PubMed] [Google Scholar]
- Ma H, Calderon TM, Fallon JT, Berman JW. Hepatocyte growth factor is a survival factor for endothelial cells and is expressed in human atherosclerotic plaques. Atherosclerosis. 2002;164:79–87. doi: 10.1016/s0021-9150(02)00062-x. [DOI] [PubMed] [Google Scholar]
- Ueda H, Imazu M, Hayashi Y, Ono K, Yasui W, Yamakido M. Immunohistochemical analysis of hepatocyte growth factor in human coronary atherectomy specimens: comparison with transforming growth factor beta isoforms. Virchows Arch. 1997;430:407–415. doi: 10.1007/s004280050050. [DOI] [PubMed] [Google Scholar]
- Hayashi K, Nakamura S, Morishita R, Moriguchi A, Aoki M, Matsumoto K, Nakamura T, Kaneda Y, Sakai N, Ogihara T. In vivo transfer of human hepatocyte growth factor gene accelerates re-endothelialization and inhibits neointimal formation after balloon injury in rat model. Gene Ther. 2000;7:1664–1671. doi: 10.1038/sj.gt.3301284. [DOI] [PubMed] [Google Scholar]