Abstract
The prevalence of concurrent multitypic hepatitis C virus (HCV) infection is uncertain. A sensitive and specific approach to identifying minority HCV genotypes in blood is presented. Following serum extraction and reverse transcription PCR to amplify cDNA originating from the viral 5′ noncoding region, the amplified product mixture was treated with genotype-specific restriction endonuclease to digest the dominant genotype. Residual amplicons were subjected to PCR cloning and then to real-time DNA sequencing using a Pyrosequencer to identify the remaining genotypes. Dilution experiments showed that minority genotypes may be detected when they represent 1:10,000 of the total population and in serum specimens with viral loads as low as 1,000 IU/ml. Of 37 patients with bleeding disorders and 44 injecting drug users, infection by more than one HCV genotype was found in 7 (19%) and 4 (9%) patients, respectively. The low rate of detection in people at high risk of repeated HCV infection suggests that multitypic HCV carriage is uncommon.
Hepatitis C virus (HCV) exhibits substantial genetic variation (4). Six distinct viral genotypes and a variable number of subtypes have been described (3). Genotypes tend to segregate geographically. Thus, in England and Wales, genotype 1 (subtypes 1a and 1b) and genotype 3 (subtype 3a) are the most prevalent, while genotypes 4, 5, and 6 are not (8). As patients infected with different genotypes respond differently to antiviral drugs, identification of the infecting HCV genotype has become important to guide the choice of the mode and duration of antiviral therapy (24, 25).
Multitypic HCV infection has been reported in individuals at risk of multiple or repeated HCV exposures, e.g., patients with bleeding disorders given inadequately sterilized clotting factor concentrates (11, 16, 21) and injection drug users (IDUs) (1). Infection of a host with multiple HCV genotypes potentially complicates pre-antiviral therapy assessments. It has been proposed as a possible mechanism for nonresponse to alpha interferon-based antiviral therapy, as selection of minority genotype populations more refractory to antiviral treatment can emerge during treatment (18). Moreover, the precision of studies on the transmission of HCV also depends on whether or not minority genotypes can be tracked along with the dominant ones.
Genotyping has been carried out by identifying type-specific nucleotide sequence polymorphisms in products derived by consensus PCR sequencing of HCV cDNA (5, 19). This approach has limited value when applied to detect minority genotypes, as it lacks sensitivity. Furthermore, the predominant viral strain tends to be preferentially amplified (9). Thus, studies using these approaches to evaluate the prevalence of multitypic HCV infection likely lead to underestimates. Other approaches have been adopted to study multitypic HCV infection specifically (5, 9, 10, 18, 20-22). Those involving PCR cloning and sequencing are potentially the most effective to identify minority populations, but the impracticality and expense of sequencing large numbers of clones restrict their wider applicability.
We report the development of an approach to identify minority HCV genotypes circulating in people at risk of multiple or repeated exposures to HCV, namely, patients with bleeding disorders and IDUs. This approach involves the eradication of amplicons derived from the cDNA of the dominant genotype by genotype-specific restriction endonuclease digestion followed by real-time DNA sequencing to characterize PCR clones generated from residual, undigested amplicons.
MATERIALS AND METHODS
Strategy to identify minority HCV genotypes.
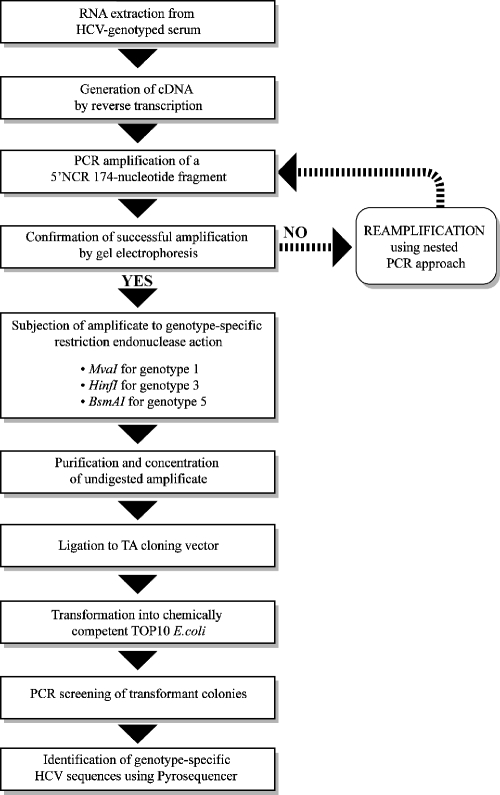
The strategy to identify minority HCV genotypes is summarized in Fig. 1.
FIG. 1.
Flow diagram summarizing the approach used to identify minority genotypes in serum.
Patient samples.
A panel of archived sera collected between May 2001 and July 2004 from 37 HCV-seropositive patients with bleeding disorders attending the Hemophilia Reference Center, St. Thomas' Hospital, London, United Kingdom, was assembled. The bleeding disorders and number of patients were the following: hemophilia A, 26 (70%); hemophilia B, 7 (19%); von Willebrand's disease, 3 (8%); and afibrinogenemia, 1 (3%). Bleeding severity was scored as severe in 21 (57%) patients, moderate in 2 (5%), and mild in 10 (27%); the severity was unknown for 4 (11%). All patients were naïve to anti-HCV chemotherapy, and their infecting HCV had earlier been genotyped by a protocol based on restriction-fragment length polymorphism (RFLP) analysis (15). Only individuals identified in this assay to be infected with genotypes 1a, 1b, or 3a and 5a were included in the study; those infected with other genotypes were not. Written informed consent was obtained from the patients agreeing to participate in the study. In addition to type of bleeding disorder and disease severity, the human immunodeficiency virus (HIV) coinfection status was recorded for each patient. Another panel of study samples, collected between March 2002 and December 2003, was derived from unlinked anonymous sera from 44 HCV-seropositive patients identified as IDUs undergoing diagnostic hepatitis C testing from centers participating in the ongoing Hepatitis C Denominator Study of England and Wales. The IDUs were newly identified as HCV infected and had not been given anti-HCV chemotherapy. Only individuals infected with genotype 1a, 1b, or 3a by the RFLP-based assay were included. The injecting drug use status was determined by information on the request form or from a follow-up questionnaire sent to the clinician requesting the test. No clinical data were available for this group. Sera derived from two additional patients, which were routinely referred to our laboratory for reference HCV testing, were used for dilution experiments.
HCV RNA extraction, cDNA synthesis, and PCR amplification.
Viral RNA was extracted from 300 μl of serum using the Ultra Sens Viral RNA kit (QIAGEN, Hilden, Germany) per the manufacturer's instructions. cDNA was generated by reverse transcription. In each reaction, 25 mM Tris (pH 8.4), 62.5 mM KCl, 5 mM MgCl2, 1 mM deoxynucleotide triphosphate mix, 20 U random hexameric oligonucleotides, 13.6 U RNasin (Promega, Madison, WI), and 200 U Moloney murine leukemia virus reverse transcriptase (Invitrogen, Paisley, United Kingdom) were mixed with 22.2 μl of RNA extract, which was adjusted to a total volume of 40 μl with nuclease-free water. The mixture was incubated at room temperature for 10 min followed by 37°C for 45 min, and it was then terminated after a further 5 min at 95°C. A 174-nucleotide fragment of the viral 5′ noncoding region (5′NCR) was amplified using a single-round PCR with oligonucleotide primers 126 and 299 (13). For each reaction, 10 μl of the cDNA reaction was added to 40 μl of the following reaction mix: 20 mM Tris (pH 8.4), 70 mM KCl, 1 mM MgCl2, 20 pmol each primer, and 1 U of Taq polymerase (Invitrogen). Reactions were cycled using a PTC-200 thermal cycler (MJ Research, Watertown, MA) with an initial incubation of 4 min at 94°C and then 40 cycles of 20 s at 94°C, 30 s at 54°C, and 35 s at 72°C, with a final extension of 3 min at 72°C. PCR products were electrophoretically separated and visualized under UV light. A number of specimens that failed to amplify using this single-round strategy were subjected to reamplification using a nested PCR approach. The first-round amplification used oligonucleotide primers 57 and 321 (13). The reaction mix was the same as that described above but with the following amplification conditions: 4 min at 94°C, and then 25 cycles of 20 s at 94°C, 40 s at 62°C, and 35 s at 72°C, with a final extension of 3 min at 72°C. For each second-round PCR, a 2-μl portion of the initial PCR was added to the following reaction mix: 20 mM Tris (pH 8.4), 72 mM KCl, 2 mM MgCl2, 20 pmol each of oligonucleotide primers 126 and 299, 0.2 mM deoxynucleotide triphosphate mix, 1 U of Taq polymerase. It was adjusted to 50 μl with nuclease-free water. Reactions were amplified using 25 cycles of 20 s at 94°C, 40 s at 68°C, and 30 s at 72°C, with a final extension of 3 min at 72°C.
Genotype-specific restriction digestion.
In order to selectively cleave the known dominant genotype amplicons, PCR products were subjected to a genotype-specific restriction endonuclease action. Genotype-specific restriction endonucleases were selected by aligning reference sequences representing genotypes 1 to 5 (Sequencher version 4.2; Ann Arbor, MI). Amplified product mixtures from specimens previously determined to carry HCV genotype 1 were treated with MvaI (Roche, Lewes, United Kingdom), those infected with genotype 3 were treated with HinfI (New England Biolabs, Beverly, MA), and the single specimen that carried genotype 5 was treated with BsmAI (New England Biolabs). Products were then purified using the GFX PCR DNA and gel band purification kit (Amersham-Pharmacia, Little Chalfont, United Kingdom) per the manufacturer's instructions and eluted into 12.5 μl of nuclease-free water.
HCV load determination.
The two HCV-carrying sera used for sensitivity studies had their viral loads quantified using the COBAS AmpliPrep/COBAS Taqman HCV assay (Roche). The input volume of serum was 1 ml. This approach has a dynamic range between 15 IU/ml and 6.9 × 107 IU/ml.
Cloning and transformant screening.
The digested PCR products were subjected to a reaction to ligate to the TOPO-TA cloning vector (Invitrogen), according to the manufacturer's instructions, and were transfected into chemically competent TOP10 Escherichia coli. Transformants were selected by overnight incubation on nutrient agar plates containing 50 μg/ml of ampicillin. Using DNA from whole cells as template, typically 15 colonies were screened using PCR amplification with 5′ biotinylated antisense oligonucleotide primer 299, whose sequence is described above, but with an initial incubation of 10 min at 80°C.
Pyrosequencing and analysis.
Pyrosequencing was performed using a PSQ 96 sample preparation kit and a PSQ MA analyzer (Biotage, Uppsala, Sweden). The technique enables rapid detection of single-nucleotide polymorphisms and the reading of small lengths of nucleotides from the PCR product mixture by a process known as “sequencing by synthesis,” based on the quantitative detection of inorganic pyrophosphate released following nucleotide incorporation into a growing DNA chain. The system uses coupled enzymatic reactions to monitor pyrophosphate released during nucleotide incorporation. Free pyrophosphate activates the enzyme cascade, resulting in light emission. Light signals proportional to the amount of pyrophosphate released are obtained by the concerted action of ATP sulfurylase and luciferase. During each minute-long cycle, unreacted nucleotides are degraded by apyrase, allowing iterative addition of nucleotides. The light signatures produced by the hydrolysis of luceferin are then recorded and plotted into a simple graphic form, known as a pyrogram, from which sequence data are obtained. A 42-nucleotide fragment of the viral 5′NCR, from positions −140 to −98 in the HCV genome (positions follow the system of Choo et al. [4]), constituted the fragment of analysis, as it encompasses genotype-specific base sequence polymorphisms. Oligonucleotide F-new (5′-CGGGTCCTTTCTTGG-3′) was annealed to 20 μl of the digested PCR product by heating for 2 min at 80°C and allowing it to cool to room temperature. The Pyrosequencer operator system enables the selection of a specific nucleotide dispensation order, adding defined nucleotides at each cycle which correspond to the region of interest. In order to determine this nucleotide dispensation order, an alignment of all the published full-length sequences representing the six genotypes (MegAlign 5.03; DNAstar Inc., Madison, WI) was assembled. Nucleotide sequences were characterized and given genotype assignments following alignments to reference sequences and BLAST analysis (2).
Determination of assay sensitivity using PCR amplicon titrations.
A 265-nucleotide PCR fragment of the 5′NCR (generated using oligonucleotide primers 57 and 321) was cloned from a serum sample known to be carrying genotype 1a and another sample carrying genotype 3a HCV, both of which had been referred for genotyping. Individual clones were screened for inserts, and plasmid DNA was isolated from overnight cultures using the Miniprep spin kit (QIAGEN). From each clonal template further amplicons were generated using primers 126 and 299, and the resulting DNA content was spectrophotometrically quantified at 260 nm. Amplified product mixtures produced from the same template were pooled and resuspended to a concentration of 1 ng/μl in nuclease-free water (representing a weakly positive PCR amplification). A panel consisting of the type 1-amplified products diluted in graduation with the type 3-amplified products were prepared in the following series: 1:2, 1:10, 1:100, 1:1,000, 1:10,000, and 1:100,000 (each having a total volume of 50 μl). A similar panel comprising the type 3-amplified products prepared with graduating dilutions of the type 1-amplified products were also prepared. Each dilution mixture was treated with the appropriate restriction endonuclease to digest the dominant genotype, and the undigested product was subjected to the same cloning and pyrosequencing procedure as that described above.
Determination of assay sensitivity using dilutions of virus in clinical serum samples.
A further two serum specimens derived from HCV-infected patients had been genotyped using the RFLP-based protocol as separately carrying HCV genotypes 3a and 1a. Their viral loads were determined and adjusted to 1 × 105 and 1 × 107 IU/ml, respectively, using anti HCV-seronegative normal human serum. The specimens were mixed such that virus from the genotype 3a-carrying specimen constituted 0.01% (equivalent to a ratio of 1:10,000) of the genotype 1a-carrying specimen in a total volume of 1 ml. This serum was then serially diluted to provide a range of 10-fold dilutions from 1 × 107 IU/ml to 100 IU/ml. Each dilution mixture was exposed to the minority genotype detection procedure without replicate testing.
DNA sequencing.
For each study sample from which a minority genotype was identified by pyrosequencing, the result was confirmed by nucleotide sequence analysis of PCR amplicons originating from one representative clone using the CEQ 2000 dye terminator cycle sequencing kit (Beckman-Coulter, Fullerton, CA).
RESULTS
Genotype identification by pyrosequencing.
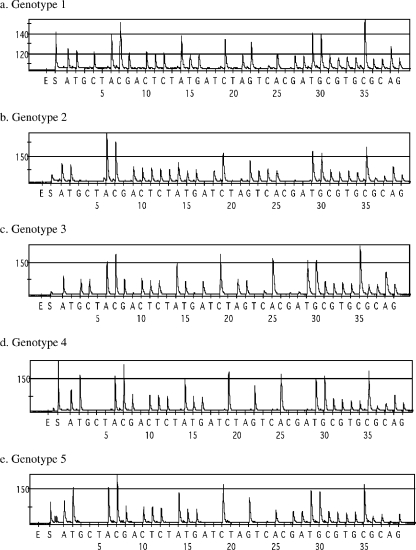
Representative pyrograms generated from study specimens that represent HCV genotypes 1 to 5 are shown in Fig. 2.
FIG. 2.
Characteristic pyrogram traces generated from 5′NCR of HCV belonging to different genotypes. The y axis shows signal intensity in arbitrary light units, and the x axis shows temporal dispensation of nucleotides in minutes. E, dispensation of enzyme mix. S, dispensation of lumogenic substrate.
Assay sensitivity.
Studies using the two dilution panels showed that, with the total amplicon concentration set at 50 ng/reaction, the minority genotype could be identified even when constituting 1:10,000 of the total population. This represents the lowest dilution at which at least one randomly selected clone contains an insert originating from the minority type. This level of sensitivity was achieved whether the genotype 1-amplified product mixture was diluted in the genotype 3-amplified product mixture or vice versa. A 10-fold dilution series of a mixture of two sera, with the serum carrying genotype 3a diluted in the serum carrying genotype 1a, was prepared. Fifteen randomly selected clones were analyzed at each dilution. From all test specimens representing an HCV genome concentration of 1,000 IU/ml or greater, one or more colonies could be found to contain a PCR insert derived from genotype 3a.
Comparison of multitypic infection between the two study groups.
A total of 81 specimens were tested, 37 from patients with bleeding disorders and 44 from IDUs. A total of 29 patient specimens failed to amplify using the single-round amplification strategy and therefore required reamplification by nested PCR. The infecting genotype as determined by RFLP analysis of the 5′NCR showed a predominance of type 1 over type 3 infection in the bleeding disorders group (23/37; 62%) compared to the IDU group (17/44; 39%) (P = 0.003; Fisher's exact test). Of the total number of specimens tested, 11 (14%) were found to carry more than one genotype. The difference in proportion of multitypic HCV carriage did not differ significantly between the samples from the bleeding disorders group (7/37; 19%) and the IDU group (4/44; 9%).
Multitypic infection in patients with bleeding disorders.
Patients in the bleeding disorders study group were between the ages of 27 and 71 years (mean, 42 years) at the time of sampling. The dominant HCV genotype as determined by RFLP analysis of the 5′NCR was genotype 1a in 23 (62%) patients, genotype 1b in 8 (22%), genotype 3a in 5 (14%), and genotype 5a in 1 (3%). HIV coinfection had been diagnosed in 10 (27%). Carriage of multitypic HCV was found in the serum of seven patients (19%). The combinations of minority genotypes detected are presented in Table 1. Multitypic infection tended to occur in patients aged between 38 and 53 years rather than in those <38 years or >53 years (maximum likelihood regression analysis against a quadratic effect of age, P = 0.038) and in hemophilia A patients than for other forms of bleeding disorders (P = 0.08; Fisher's exact test).
TABLE 1.
Distribution of minority HCV genotypes identified in sera of patients with bleeding disorders
| Genotype detected by 5′NCR RFLP | No. of patients with minority genotype(s):
|
Total | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 + 2 | 2 + 3 | None | ||
| 1a | 2 | 2 | 1 | 18 | 23 | ||
| 1b | 1 | 7 | 8 | ||||
| 3a | 1 | 4 | 5 | ||||
| 5a | 1 | 1 | |||||
Multitypic infection in IDUs.
The age range of the IDU study group was from 22 to 66 years (mean, 40 years). Injecting drug use was reported as current in 8 (18%) patients, previous in 19 (43%), and unknown in 17 (39%). The dominant HCV genotype was determined as 1a in 17 (38%) patients, 1b in 7 (16%), and 3a in 20 (54%). Multitypic HCV carriage was identified in 4 (9%) samples, in one current and one former drug user and in two subjects of unknown drug use status. The combinations of minority genotypes detected are presented in Table 2.
TABLE 2.
Distribution of minority HCV genotypes identified in sera of IDUs
| Genotype detected by 5′NCR RFLP | No. of patients with minority genotype(s):
|
Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 2 + 3 | None | ||
| 1a | 17 | 17 | ||||||
| 1b | 1 | 1 | 5 | 7 | ||||
| 3a | 1 | 1 | 18 | 20 | ||||
DISCUSSION
The prevalence of concurrent multitypic HCV infection remains difficult to ascertain. In patients with bleeding disorders receiving blood products from donors who have not been screened for anti-HCV antibody and who accordingly are more prone to multiple HCV infection, the prevalence ranges from 0% to 25% (10, 16, 20, 22). The wide variation reported may be explained by the variety of approaches for detecting mixed-genotype infection. Other than consensus PCR sequencing, approaches used to study the prevalence of multitypic HCV infection include the INNO-LiPA line probe assay (17), type-specific PCR (7, 20, 22), primer-specific mispair extension analysis (9), sequence analysis of PCR clones (6), and serotyping combined with genotyping (18). These differ in terms of sensitivity in the ability to detect minority genotypes and of specificity in the assignment of genotypes.
In the approach described here, which uses real-time nucleotide sequencing to characterize PCR clones generated after amplicons from the dominant HCV genotype carried in serum have been digested by genotype-specific restriction endonuclease action, minority genotypes belonging to types 1 to 5 could be identified. Such an approach confers a number of advantages. First, once the dominant HCV genotype is eliminated, characterization of the PCR clones originating from residual genomes, which represent those of the minority genotype, rapidly leads to assignment of that genotype. Each pyrosequencing reaction takes approximately 40 min to complete, enabling the sequences of a large number of PCR-derived clones to be characterized in a single run without the need for direct nucleotide sequencing. While from each undigested ampificate we usually screen 15 clones to identify minority genotypes, up to 96 clones per pyrosequencing run may be screened. Second, the approach can identify more than one minority genotype at a time. Third, it is exquisitely sensitive compared to other methods used to detect multitypic infection. In a viral population consisting of dominant and minority genotypes, a consensus PCR sequencing approach can detect minority genotypes, if present, at >10% (14), the INNO-LiPA line probe assay can detect minority genotypes, if present, at >3% (12), heteroduplex mobility assay can detect minority genotypes, if present, at >2% (23), and the semiautomated primer-specific mispair extension analysis can detect minority genotypes, if present, at >0.8% (9); these detection levels contrast with the sensitivity levels obtained using the approach described here. We were able to detect a minority genotype population of 1:10,000 when the overall viral load of the specimen was greater than 1,000 IU/ml. Some caution may need to be applied to accepting the stated sensitivity limit, as replicate testing of each dilution of the sera was not conducted. Fourth, specificity is assured, as the identity of the minority genotype detected is characterized from the sequence that is directly derived from the genome.
There are limitations to the use of this approach. First, it is qualitative: no information on the viral load of minority genotypes present in the sample can be determined. Second, specimens may carry minority genotypes that are still undetectable. Such a situation can arise in at least three ways. (i) The ability to detect minority genotypes following the digestion of the dominant genotype may relate to the quantity of the dominant genotype in the sample: high quantities may result in incomplete digestion by the given amount of restriction endonuclease added into the digestion reaction. (ii) The likelihood of detecting minority genotypes is directly proportional to the number of PCR clones available after cloning has been applied to the postdigestion amplified product mixture. (iii) The restriction endonuclease digestion used to cleave the PCR product originating from the dominant genotype is not completely genotype specific. Thus, the use of MvaI to cleave amplicons from genotype 1 can also cleave minority populations belonging to genotype 6, and the use of HinfI to cleave amplicons from genotype 3 can also cleave certain subtypes from genotype 4. We based this assessment of genotype specificity on the alignment of a small but representative sample of published sequences of genotypes 1 to 5. The possibility that some amplicons will not be cleaved by restriction endonucleases remains. No appropriate restriction endonucleases to specifically cleave amplicons from genotype 2 or 4 are available; for this reason, patients carrying genotype 2 or 4 were excluded from the study. We had intended to study the association between multitypic carriage and the viral load of the samples, but the volume of the residual specimens was too small to permit this. Lastly, the region of sequence used by this technique is insufficient to discriminate between genotypes 1 and 6. For this reason, patients carrying genotype 6 were also excluded from the study.
Despite the application of a very sensitive approach to detect minority HCV genotypes, the prevalence of multitypic infection in the two study groups was found to be low even though they were at high risk of multiple and repeated HCV exposure, particularly among those with bleeding disorders. The proportion was higher among this group but did not differ significantly from that in IDUs. The approach to identify multitypic HCV infection described here potentially permits the complex epidemiology of HCV infection to be unraveled. Its further application allows an evaluation of how the persistence of minority HCV genotypes may be associated with poor response to anti-HCV therapy and of the extent to which infection by minority genotypes affects molecular epidemiologic assessments of HCV transmission events.
Acknowledgments
This work was supported by a grant funded by the Department of Health, England.
We thank Lisa Brant for providing data relating to specimens originating from IDUs, David Gelb for support with statistical testing, and staff of the HIV/Hepatitis Reference Laboratory for HCV genotyping. William Irving of Queen's Medical Centre, Nottingham, England, and Clive Taylor of Health Protection Agency North East, Newcastle, England, provided additional specimens.
REFERENCES
- 1.Alter, M. J., D. Kruszon-Moran, O. V. Nainan, G. M. McQuillan, F. Gao, L. A. Moyer, R. A. Kaslow, and H. S. Margolis. 1999. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N. Engl. J. Med. 341:556-562. [DOI] [PubMed] [Google Scholar]
- 2.Altschul, S. F., W. Gish, W. Miller, E. W. Myers, and D. J. Lipman. 1990. Basic local alignment search tool. J. Mol. Biol. 215:403-410. [DOI] [PubMed] [Google Scholar]
- 3.Chan, S. W., F. McOmish, E. C. Holmes, B. Dow, J. F. Peutherer, E. Follett, P. L. Yap, and P. Simmonds. 1992. Analysis of a new hepatitis C virus type and its phylogenetic relationship to existing variants. J. Gen. Virol. 73:1131-1141. [DOI] [PubMed] [Google Scholar]
- 4.Choo, Q. L., K. H. Richman, J. H. Han, K. Berger, C. Lee, C. Dong, C. Gallegos, D. Coit, R. Medina-Selby, and P. J. Barr. 1991. Genetic organization and diversity of the hepatitis C virus. Proc. Natl. Acad. Sci. USA 88:2451-2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davidson, F., P. Simmonds, J. C. Ferguson, L. M. Jarvis, B. C. Dow, E. A. Follett, C. R. Seed, T. Krusius, C. Lin, and G. A. Medgyesi. 1995. Survey of major genotypes and subtypes of hepatitis C virus using RFLP of sequences amplified from the 5′ non-coding region. J. Gen. Virol. 76:1197-1204. [DOI] [PubMed] [Google Scholar]
- 6.Devereux, H., P. Telfer, G. Dusheiko, and C. Lee. 1995. Hepatitis C genotypes in haemophilic patients treated with alpha-interferon. J. Med. Virol. 45:284-287. [DOI] [PubMed] [Google Scholar]
- 7.Giannini, C., F. Giannelli, M. Monti, G. Careccia, M. E. Marrocchi, G. Laffi, P. Gentilini, and A. L. Zignego. 1999. Prevalence of mixed infection by different hepatitis C virus genotypes in patients with hepatitis C virus-related chronic liver disease. J. Lab. Clin. Med. 134:68-73. [DOI] [PubMed] [Google Scholar]
- 8.Harris, K. A., C. Gilham, P. P. Mortimer, and C. G. Teo. 1999. The most prevalent hepatitis C virus genotypes in England and Wales are 3a and 1a. J. Med. Virol. 58:127-131. [DOI] [PubMed] [Google Scholar]
- 9.Hu, Y. W., E. Balaskas, M. Furione, P. H. Yen, G. Kessler, V. Scalia, L. Chui, and G. Sher. 2000. Comparison and application of a novel genotyping method, semiautomated primer-specific and mispair extension analysis, and four other genotyping assays for detection of hepatitis C virus mixed-genotype infections. J. Clin. Microbiol. 38:2807-2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isobe, K., M. Imoto, Y. Fukuda, Y. Koyama, I. Nakano, T. Hayakawa, and J. Takamatsu. 1995. Hepatitis C virus infection and genotypes in Japanese hemophiliacs. Liver 15:131-134. [DOI] [PubMed] [Google Scholar]
- 11.Kao, J. H., P. J. Chen, M. Y. Lai, P. M. Yang, J. C. Sheu, T. H. Wang, and D. S. Chen. 1994. Mixed infections of hepatitis C virus as a factor in acute exacerbations of chronic type C hepatitis. J. Infect. Dis. 170:1128-1133. [DOI] [PubMed] [Google Scholar]
- 12.Laperche, S., F. Lunel, J. Izopet, S. Alain, P. Deny, G. Duverlie, C. Gaudy, J. M. Pawlotsky, J. C. Plantier, B. Pozzetto, V. Thibault, F. Tosetti, and J. J. Lefrere. 2005. Comparison of hepatitis C virus NS5b and 5′ noncoding gene sequencing methods in a multicenter study. J. Clin. Microbiol. 43:733-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin, H. J., N. Shi, M. Mizokami, and F. B. Hollinger. 1992. Polymerase chain reaction assay for hepatitis C virus RNA using a single tube for reverse transcription and serial rounds of amplification with nested primer pairs. J. Med. Virol. 38:220-225. [DOI] [PubMed] [Google Scholar]
- 14.Nolte, F. S., A. M. Green, K. R. Fiebelkorn, A. M. Caliendo, C. Sturchio, A. Grunwald, and M. Healy. 2003. Clinical evaluation of two methods for genotyping hepatitis C virus based on analysis of the 5′ noncoding region. J. Clin. Microbiol. 41:1558-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pohjanpelto, P., M. Lappalainen, A. Widell, K. Asikainen, and M. Paunio. 1996. Hepatitis C genotypes in Finland determined by RFLP. Clin. Diagn. Virol. 7:7-16. [DOI] [PubMed] [Google Scholar]
- 16.Preston, F. E., L. M. Jarvis, M. Makris, L. Philp, J. C. Underwood, C. A. Ludlam, and P. Simmonds. 1995. Heterogeneity of hepatitis C virus genotypes in hemophilia: relationship with chronic liver disease. Blood 85:1259-1262. [PubMed] [Google Scholar]
- 17.Qian, K. P., S. N. Natov, B. J. Pereira, and J. Y. Lau. 2000. Hepatitis C virus mixed genotype infection in patients on haemodialysis. J. Viral Hepat. 7:153-160. [DOI] [PubMed] [Google Scholar]
- 18.Schroter, M., H. H. Feucht, B. Zollner, P. Schafer, and R. Laufs. 2003. Multiple infections with different HCV genotypes: prevalence and clinical impact. J. Clin. Virol. 27:200-204. [DOI] [PubMed] [Google Scholar]
- 19.Stuyver, L., A. Wyseur, W. van Arnhem, F. Hernandez, and G. Maertens. 1996. Second-generation line probe assay for hepatitis C virus genotyping. J. Clin. Microbiol. 34:2259-2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Toyoda, H., Y. Fukuda, T. Hayakawa, T. Kumada, S. Nakano, J. Takamatsu, and H. Saito. 1999. Presence of multiple genotype-specific antibodies in patients with persistent infection with hepatitis C virus (HCV) of a single genotype: evidence for transient or occult superinfection with HCV of different genotypes. Am. J. Gastroenterol. 94:2230-2236. [DOI] [PubMed] [Google Scholar]
- 21.Tuveri, R., C. Rothschild, S. Pol, D. Reijasse, T. Persico, C. Gazengel, C. Brechot, and V. Thiers. 1997. Hepatitis C virus genotypes in French haemophiliacs: kinetics and reappraisal of mixed infections. J. Med. Virol. 51:36-41. [DOI] [PubMed] [Google Scholar]
- 22.Viazov, S., A. Widell, and E. Nordenfelt. 2000. Mixed infection with two types of hepatitis C virus is probably a rare event. Infection 28:21-25. [DOI] [PubMed] [Google Scholar]
- 23.White, P. A., X. Zhai, I. Carter, Y. Zhao, and W. D. Rawlinson. 2000. Simplified hepatitis C virus genotyping by heteroduplex mobility analysis. J. Clin. Microbiol. 38:477-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zein, N. N., J. Rakela, E. L. Krawitt, K. R. Reddy, T. Tominaga, D. H. Persing, and the Collaborative Study Group. 1996. Hepatitis C virus genotypes in the United States: epidemiology, pathogenicity, and response to interferon therapy. Ann. Intern. Med. 125:634-639. [DOI] [PubMed] [Google Scholar]
- 25.Zeuzem, S., S. V. Feinman, J. Rasenack, E. J. Heathcote, M. Y. Lai, E. Gane, J. O'Grady, J. Reichen, M. Diago, A. Lin, J. Hoffman, and M. J. Brunda. 2000. Peginterferon alfa-2a in patients with chronic hepatitis C. N. Engl. J. Med. 343:1666-1672. [DOI] [PubMed] [Google Scholar]