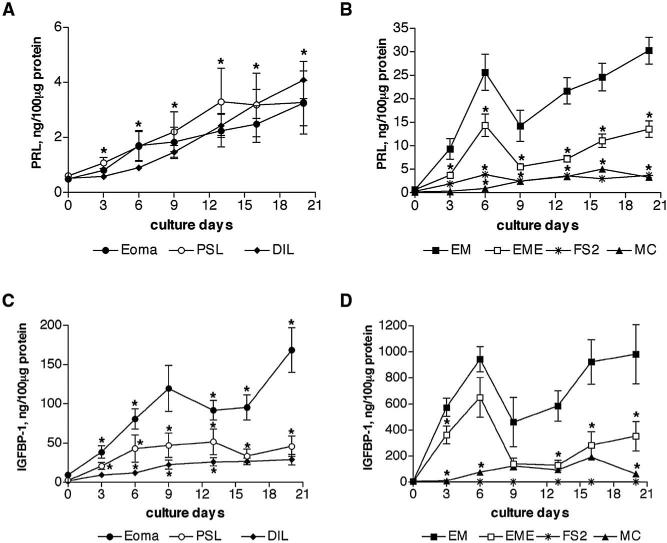
FIGURE 5.
Time-dependent secretion of PRL and IGFBP-1 in endometriotic and endometrial stromal cells. Endometriotic stromal cells (A, C) and endometrial stromal cells (B, D) were allowed to decidualize in vitro, in response to 0.5 mM of 8-Br-cAMP for 20 days. The PRL and IGFBP-1 secretion by stromal cells into supernatants was measured every 3–4 days and normalized to total protein contents. Secretion of PRL was similar by all three types of endometriotic stromal cells, dermal fibroblasts, and myometrial myocytes. Endometrial stromal cells secreted tenfold more PRL in comparison with endometriotic stromal cells (*P<.001 throughout culture period). The PRL secretion by endometrial stromal cells from women with endometriosis was also reduced by half in comparison with normal endometrial stromal cells (*P<.05, B). (C) Secretion of IGFBP-1 was >threefold higher in stromal cells derived from ovarian endometrioma compared with peritoneal surface lesions and deeply infiltrating lesions. The difference between endometrioma and deeply infiltrating lesions was significant throughout the culture period. (D) Endometrial stromal cells secreted 20-fold more IGFBP-1 in comparison with endometriotic stromal cells (*P<.001 throughout the culture period). Secretion of IGFBP-1 was also lower in endometrial stromal cells from women with endometriosis compared with those from women without endometriosis (*P<.05). (○, PSL, n = 5) peritoneal surface lesion; (diamond, DIL, n = 5) deeply infiltrating lesion; (filled circle, Eoma, n = 5) ovarian endometrioma; (asterisk, FS2, n = 1) foreskin fibroblasts; (closed square, EM, n = 5) endometrium; (open square, EME, n = 5) endometrium from women with endometriosis; (triangle, MC, n = 1) myometrial myocytes.