Abstract
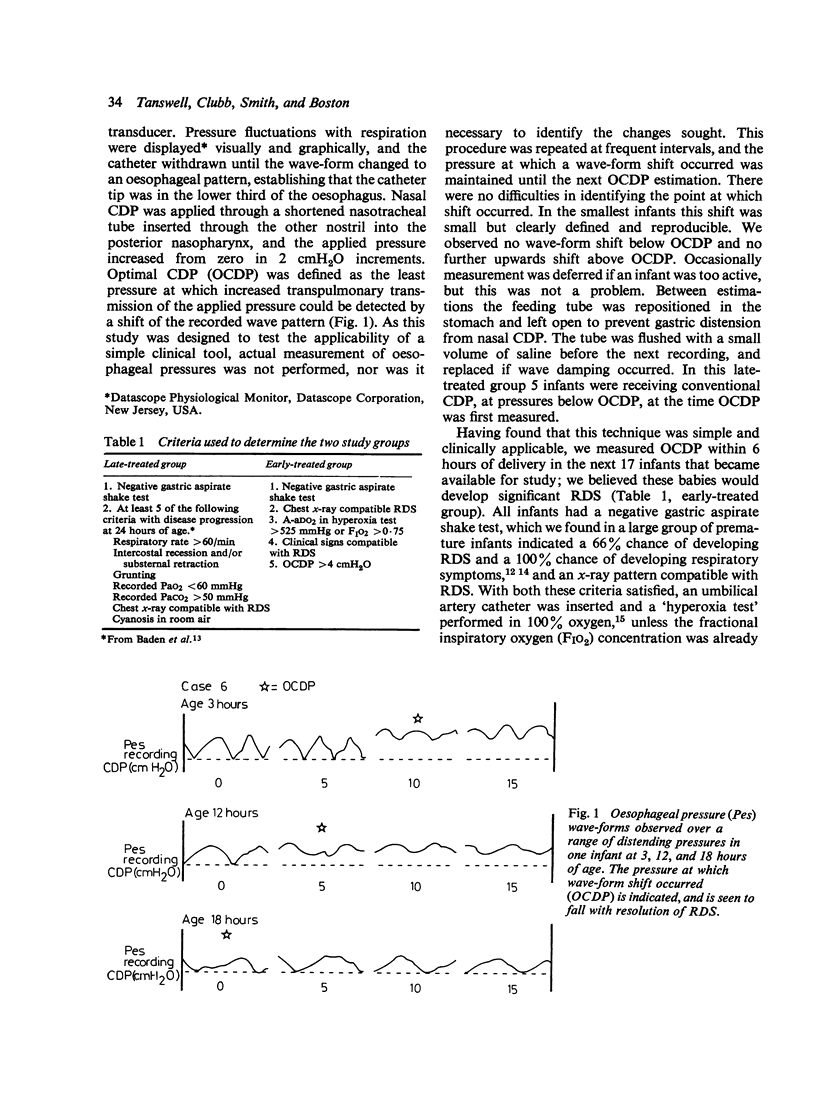
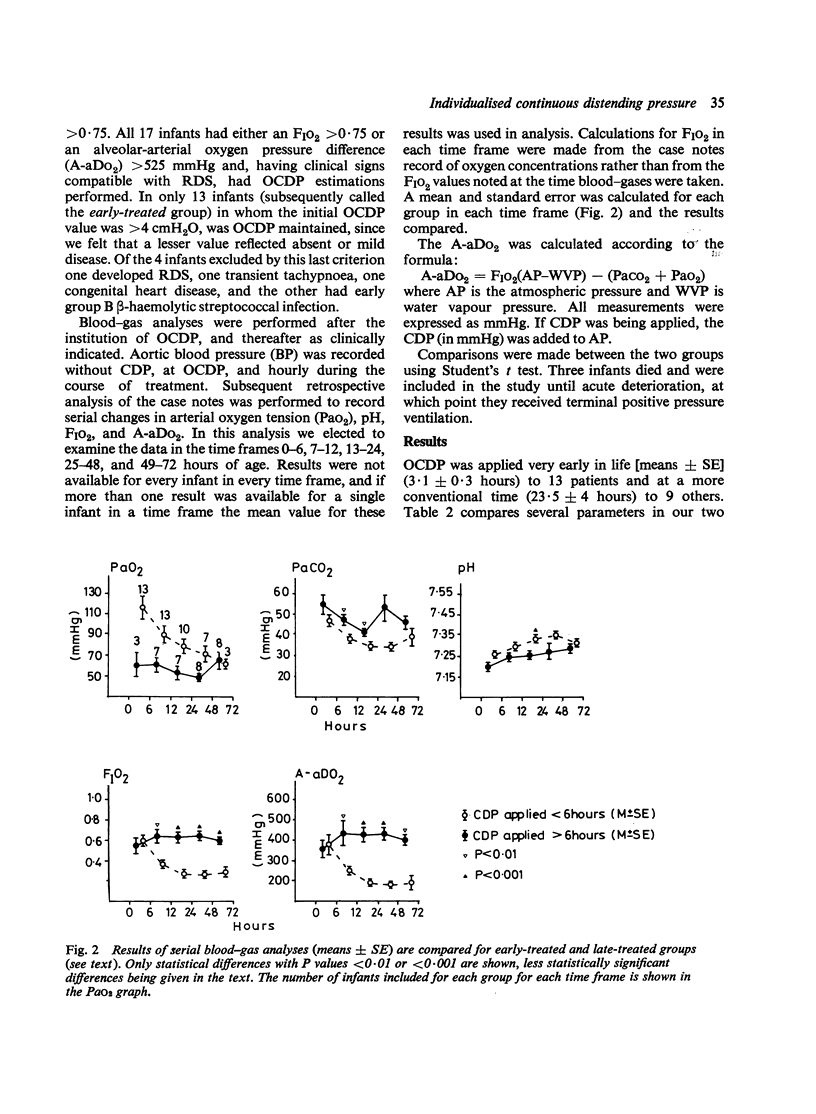
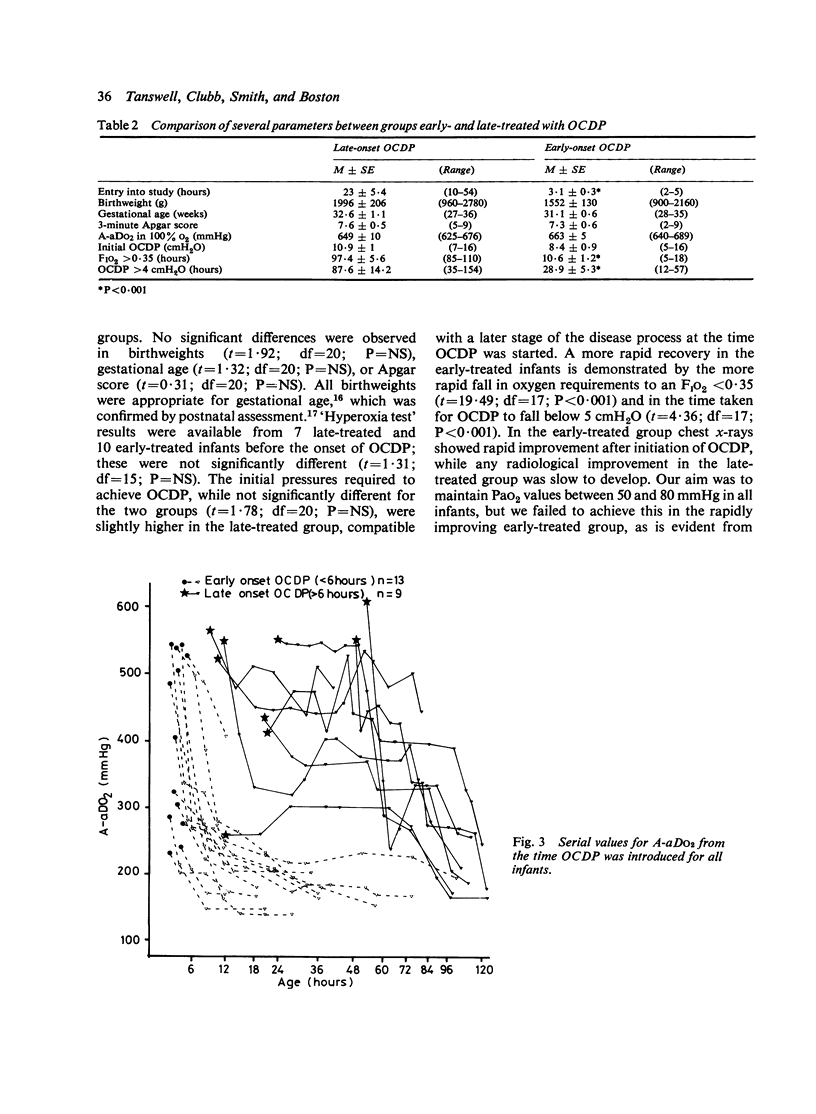
A preliminary study was performed in which a simple clinical technique for estimating appropriate levels of continuous distending pressure (CDP) in infants with respiratory distress syndrome (RDS) was used to compare two groups of infants; one group had CDP started very early in life (3.1 +/- 0.3 hours) while in the other treatment was started at a more conventional age (23 +/- 5.4 hours). Appropriate CDP was identified as the point at which transpulmonary transmission of airways pressure to the oesophagus was seen suddenly to increase, while serial measurements allowed CDP levels to be instituted and varied according to physiological signs during the course of each infant's disease. Oxygen requirements fell to less than 35% more rapidly in the early-treated group (10.6 +/- 1.2 v. 67.4 +/- 5.6 hours; P less than 0.001), as did the requirement for a CDP greater than 4 cmH2O (28.9 +/- 5.3 v. 87.6 +/- 14.2 hours; P less than 0.001). Better (P less than 0.01) values for pH, PaCO2, and A-aDO2 were observed in the early-treated group. We believe that the use of this simple technique has numerous advantages and that very early introduction of CDP can be realised in a manner selective enought for it to be used in those infants in whom intervention is justified.
Full text
PDF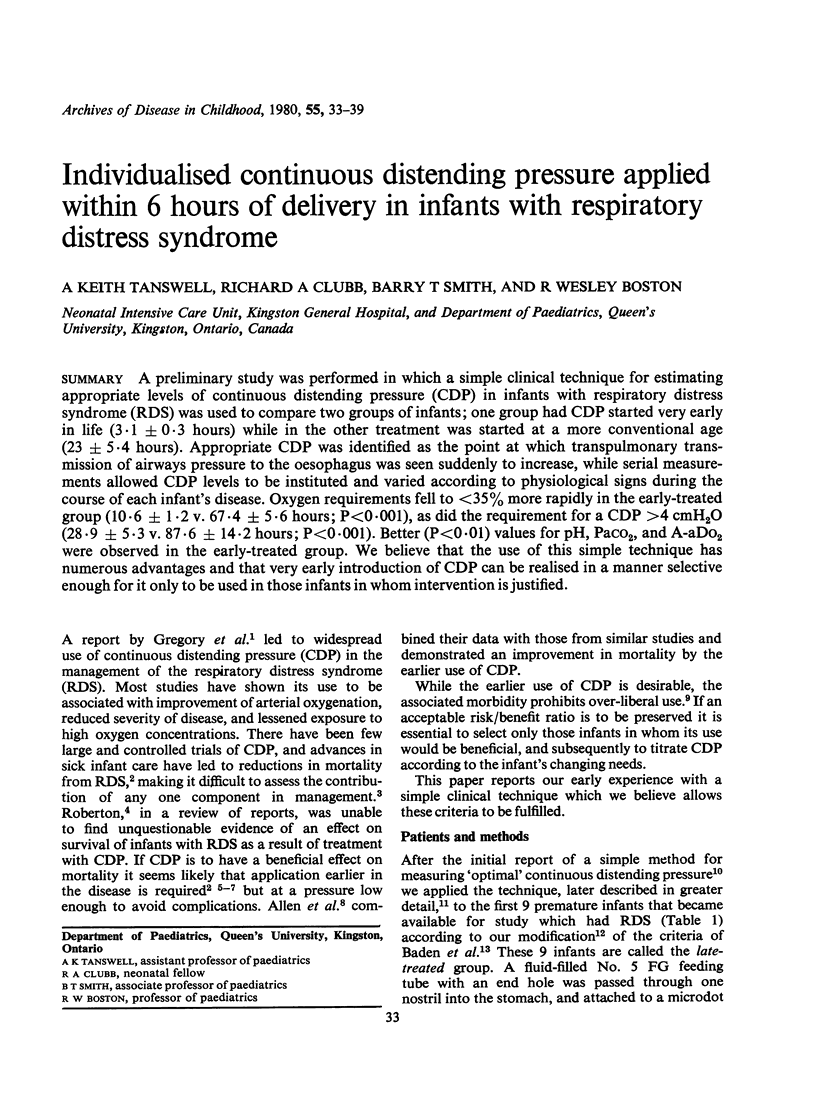

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahlström H., Jonson B., Svenningsen N. W. Continuous postive airways pressure treatment by a face chamber in idiopathic respiratory distress syndrome. Arch Dis Child. 1976 Jan;51(1):13–21. doi: 10.1136/adc.51.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen L. P., Reynolds E. R., Rivers R. P., Le Souëf P. M., Wimberley P. D. Controlled trial of continuous positive airway pressure given by face mask for hyaline membrane disease. Arch Dis Child. 1977 May;52(5):373–378. doi: 10.1136/adc.52.5.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baden M., Bauer C. R., Colle E., Klein G., Taeusch H. W., Jr, Stern L. A controlled trial of hydrocortisone therapy in infants with respiratory distress syndrome. Pediatrics. 1972 Oct;50(4):526–534. [PubMed] [Google Scholar]
- Bancalari E., Garcia O. L., Jesse M. J. Effects of continuous negative pressure on lung mechanics in idiopathic respiratory distress syndrome. Pediatrics. 1973 Mar;51(3):485–493. [PubMed] [Google Scholar]
- Bonta B. W., Uauy R., Warshaw J. B., Motoyama E. K. Determination of optimal continuous positive airway pressure for the treatment of IRDS by measurement of esophageal pressure. J Pediatr. 1977 Sep;91(3):449–454. doi: 10.1016/s0022-3476(77)81323-1. [DOI] [PubMed] [Google Scholar]
- Boston R. W., Geller F., Smith C. A. Arterial blood gas tensions and acid-base balance in the management of the respiratory distress syndrome. J Pediatr. 1966 Jan;68(1):74–89. doi: 10.1016/s0022-3476(66)80424-9. [DOI] [PubMed] [Google Scholar]
- Chernick V. Continuous distending pressure in hyaline membrane disease: of devices, disadvantages, and a daring study. Pediatrics. 1973 Jul;52(1):114–115. [PubMed] [Google Scholar]
- Chernick V., Vidyasagar D. Continuous negative chest wall pressure in hyaline membrane disease: one year experience. Pediatrics. 1972 May;49(5):753–760. [PubMed] [Google Scholar]
- Colgan F. J., Barrow R. E., Fanning G. L. Constant positive-pressure breathing and cardiorespiratory function. Anesthesiology. 1971 Feb;34(2):145–151. doi: 10.1097/00000542-197102000-00012. [DOI] [PubMed] [Google Scholar]
- Dubowitz L. M., Dubowitz V., Goldberg C. Clinical assessment of gestational age in the newborn infant. J Pediatr. 1970 Jul;77(1):1–10. doi: 10.1016/s0022-3476(70)80038-5. [DOI] [PubMed] [Google Scholar]
- Egan E. A., Hessler J. R. Positive end expiratory pressure (PEEP) and right to left shunting in immature goats. Pediatr Res. 1976 Nov;10(11):932–937. doi: 10.1203/00006450-197611000-00006. [DOI] [PubMed] [Google Scholar]
- Faridy E. E., Permutt S., Riley R. L. Effect of ventilation on surface forces in excised dogs' lungs. J Appl Physiol. 1966 Sep;21(5):1453–1462. doi: 10.1152/jappl.1966.21.5.1453. [DOI] [PubMed] [Google Scholar]
- Farrell P. M., Avery M. E. Hyaline membrane disease. Am Rev Respir Dis. 1975 May;111(5):657–688. doi: 10.1164/arrd.1975.111.5.657. [DOI] [PubMed] [Google Scholar]
- Gairdner D., Pearson J. A growth chart for premature and other infants. Arch Dis Child. 1971 Dec;46(250):783–787. doi: 10.1136/adc.46.250.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory G. A., Kitterman J. A., Phibbs R. H., Tooley W. H., Hamilton W. K. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971 Jun 17;284(24):1333–1340. doi: 10.1056/NEJM197106172842401. [DOI] [PubMed] [Google Scholar]
- Kumar A., Falke K. J., Geffin B., Aldredge C. F., Laver M. B., Lowenstein E., Pontoppidan H. Continuous positive-pressure ventilation in acute respiratory failure. N Engl J Med. 1970 Dec 24;283(26):1430–1436. doi: 10.1056/NEJM197012242832603. [DOI] [PubMed] [Google Scholar]
- Mockrin L. D., Bancalari E. H. Early versus delayed initiation of continuous negative pressure in infants with hyaline membrane disease. J Pediatr. 1975 Oct;87(4):596–600. doi: 10.1016/s0022-3476(75)80833-x. [DOI] [PubMed] [Google Scholar]
- Nelson R. M., Egan E. A., Eitzman D. V. Increased hypoxemia in neonates secondary to the use of continuous positive airway pressure. J Pediatr. 1977 Jul;91(1):87–91. doi: 10.1016/s0022-3476(77)80454-x. [DOI] [PubMed] [Google Scholar]
- Richardson C. P., Jung A. L. Effects of continuous positive airway pressure on pulmonary function and blood gases of infants with respiratory distress syndrome. Pediatr Res. 1978 Jul;12(7):771–774. doi: 10.1203/00006450-197807000-00006. [DOI] [PubMed] [Google Scholar]
- Roberton N. R. Management of neonatal respiratory failure. J R Coll Physicians Lond. 1977 Jul;11(4):389–400. [PMC free article] [PubMed] [Google Scholar]
- Robertson N. R., Tizard J. P. Prognosis for infants with idiopathic respiratory distress syndrome. Br Med J. 1975 Aug 2;3(5978):271–274. doi: 10.1136/bmj.3.5978.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suter P. M., Fairley B., Isenberg M. D. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975 Feb 6;292(6):284–289. doi: 10.1056/NEJM197502062920604. [DOI] [PubMed] [Google Scholar]
- Tanswell A. K., Sherwin E., Smith B. T. Single-step gastric aspirate shake test: bedside predictor of neonatal pulmonary morbidity. Arch Dis Child. 1977 Jul;52(7):541–544. doi: 10.1136/adc.52.7.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanswell A. K., Smith B. T. The gastric-aspirate shake test. N Engl J Med. 1977 Dec 29;297(26):1471–1471. doi: 10.1056/nejm197712292972615. [DOI] [PubMed] [Google Scholar]
- Tierney D. F., Clements J. A., Trahan H. J. Rates of replacement of lecithins and alveolar instability in rat lungs. Am J Physiol. 1967 Sep;213(3):671–676. doi: 10.1152/ajplegacy.1967.213.3.671. [DOI] [PubMed] [Google Scholar]
- Vert P., Andre M., Sibout M. Continuous positive airway pressure and hydrocephalus. Lancet. 1973 Aug 11;2(7824):319–319. doi: 10.1016/s0140-6736(73)90816-7. [DOI] [PubMed] [Google Scholar]
- Wyszogrodski I., Kyei-Aboagye K., Taeusch H. W., Jr, Avery M. E. Surfactant inactivation by hyperventilation: conservation by end-expiratory pressure. J Appl Physiol. 1975 Mar;38(3):461–466. doi: 10.1152/jappl.1975.38.3.461. [DOI] [PubMed] [Google Scholar]


