Abstract
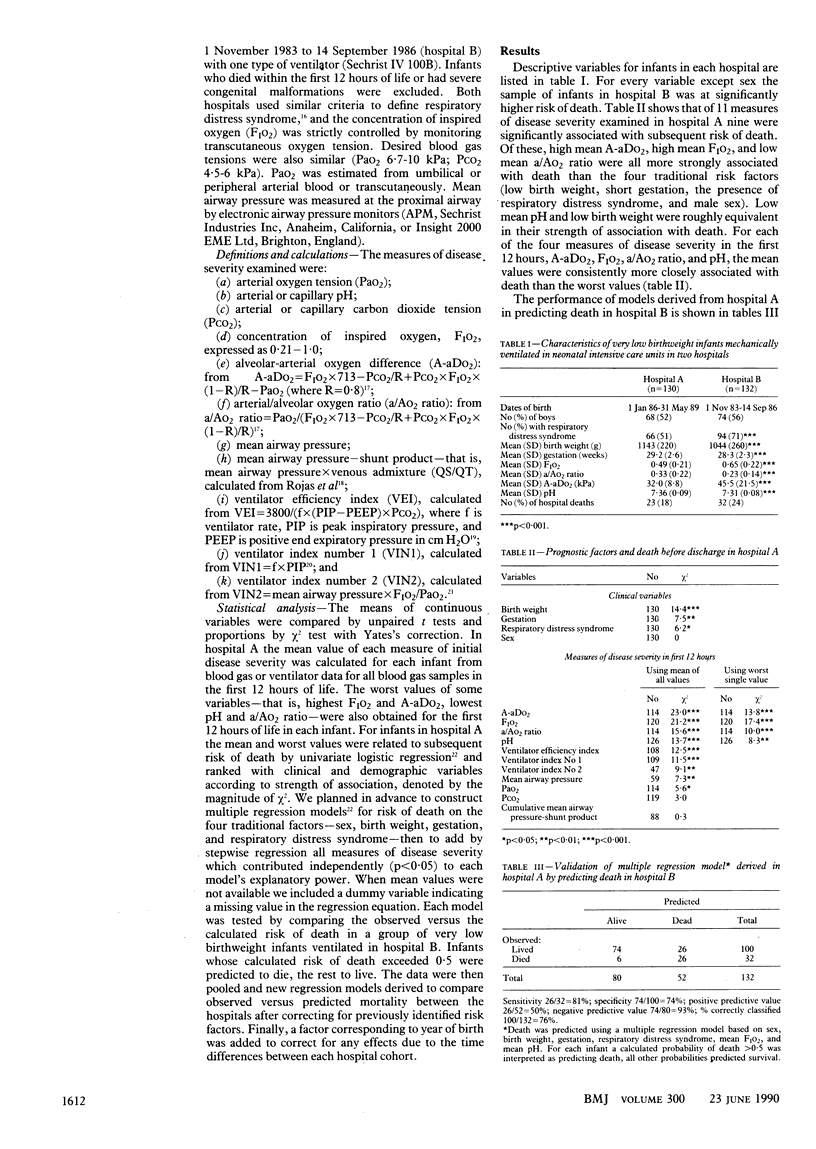
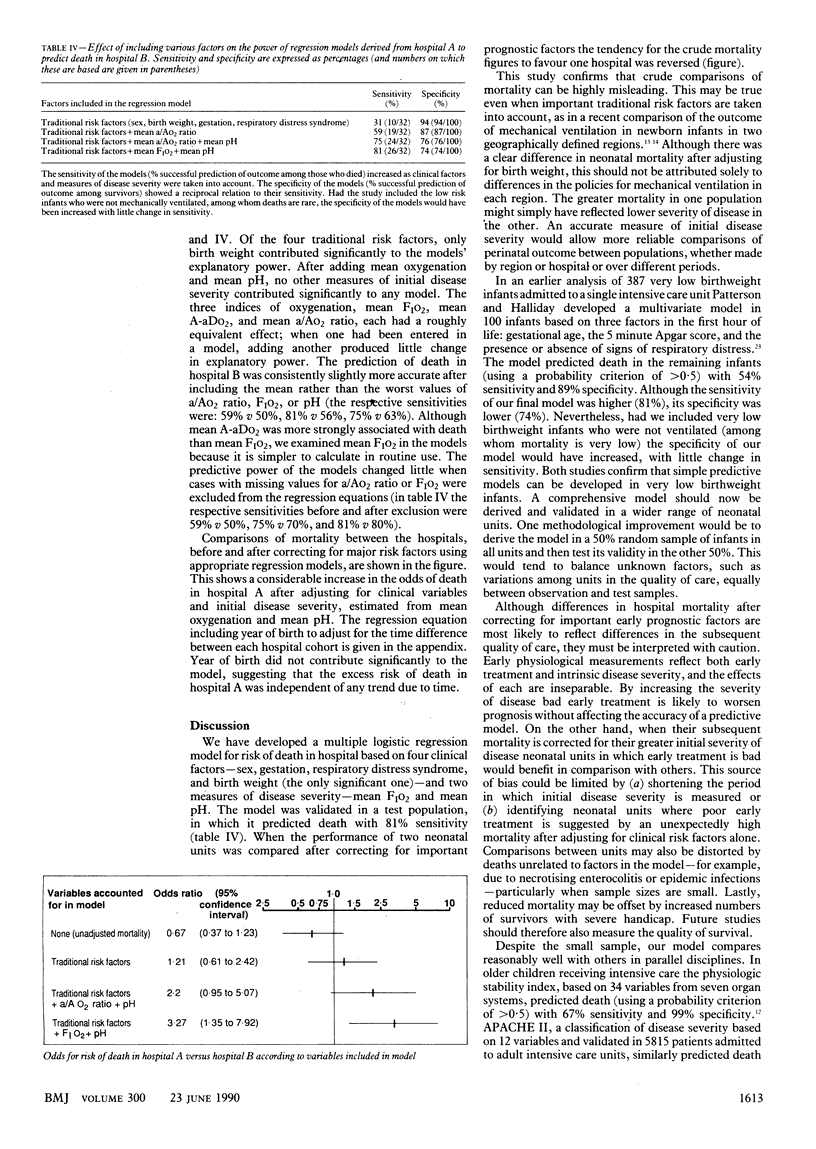
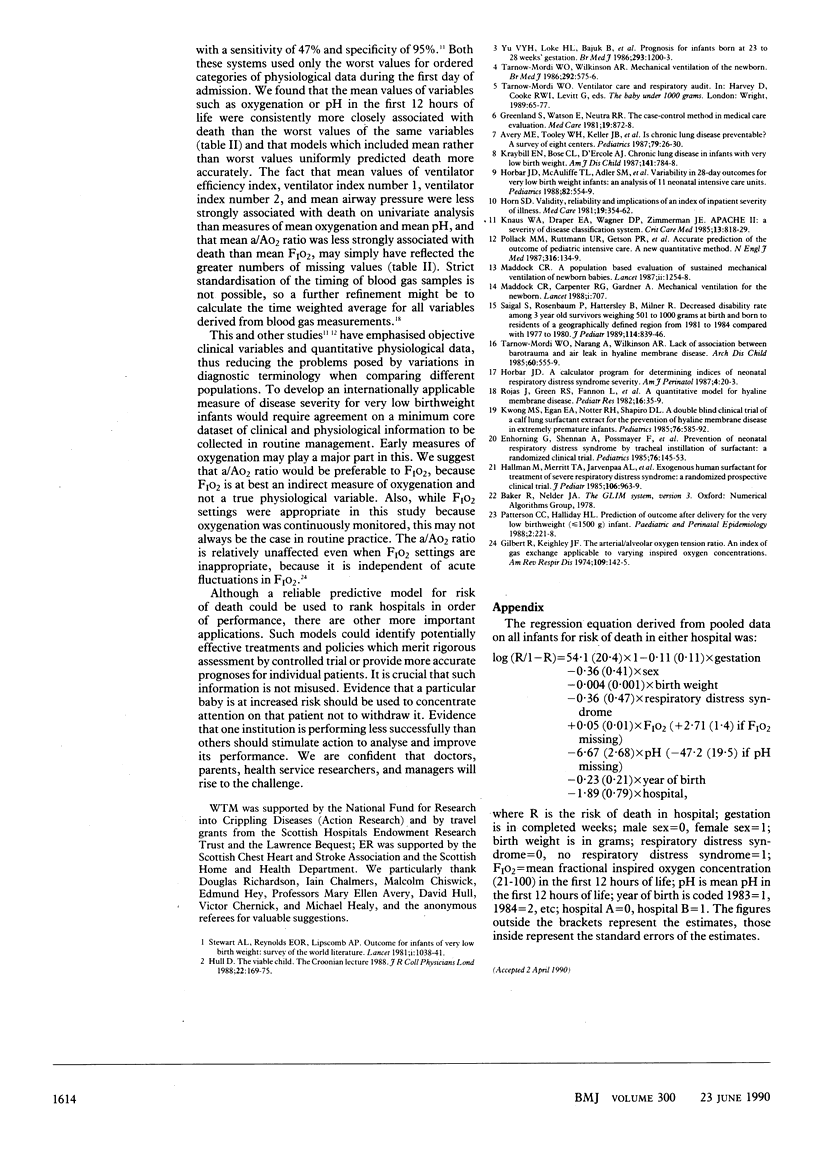
OBJECTIVES--To investigate (a) which clinical variables and physiological measures of disease severity best predict death in very low birthweight infants and (b) their use in comparing mortality between two neonatal units. DESIGN--Retrospective study of two cohorts of very low birthweight infants from overlapping time periods who received mechanical ventilation. SETTING--Two neonatal intensive care units (hospitals A and B). SUBJECTS--262 Very low birthweight infants, 130 in hospital A, 132 in hospital B. MAIN OUTCOME MEASURE--Death in hospital. RESULTS--In hospital A the mean level of oxygenation in the first 12 hours of life, whether measured as inspired oxygen requirement (FIO2), arterial/alveolar oxygen (a/AO2) ratio, or alveolar-arterial oxygen difference (A-aDO2), was more closely associated with death than any of four "traditional" risk factors: low birth weight, short gestation, the diagnosis of respiratory distress syndrome, and male sex. Mean pH in the first 12 hours was as strongly associated with death as birth weight. Multiple logistic regression models were derived in infants from hospital A using the four traditional risk factors with measures of oxygenation and pH. The validity of each model was then tested in infants from hospital B. The model based on the four traditional risk factors alone predicted death in hospital B with only 31% sensitivity. Adding mean a/AO2 ratio and mean pH increased its sensitivity to 75%, and when mean a/AO2 ratio was replaced by mean FIO2 its sensitivity increased further to 81%. Based on crude mortality rates alone, the odds of death in hospital A versus hospital B were 0.67 (95% confidence interval 0.37 to 1.23). After correcting for traditional risk factors and mean FIO2 and mean pH, however, the odds of death in hospital A increased to 3.27 (1.35 to 7.92; p less than 0.01). This increased risk persisted after adjusting for the time difference between each cohort. CONCLUSIONS--Crude comparisons of hospital mortality can be highly misleading. Reliable assessment of neonatal outcome is impossible without correcting for major risk factors, particularly initial disease severity. International agreement on a minimum core dataset of clinical and physiological information could improve neonatal audit and help to identify effective treatments and policies.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avery M. E., Tooley W. H., Keller J. B., Hurd S. S., Bryan M. H., Cotton R. B., Epstein M. F., Fitzhardinge P. M., Hansen C. B., Hansen T. N. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987 Jan;79(1):26–30. [PubMed] [Google Scholar]
- Enhorning G., Shennan A., Possmayer F., Dunn M., Chen C. P., Milligan J. Prevention of neonatal respiratory distress syndrome by tracheal instillation of surfactant: a randomized clinical trial. Pediatrics. 1985 Aug;76(2):145–153. [PubMed] [Google Scholar]
- Gilbert R., Keighley J. F. The arterial-alveolar oxygen tension ratio. An index of gas exchange applicable to varying inspired oxygen concentrations. Am Rev Respir Dis. 1974 Jan;109(1):142–145. doi: 10.1164/arrd.1974.109.1.142. [DOI] [PubMed] [Google Scholar]
- Greenland S., Watson E., Neutra R. R. The case-control method in medical care evaluation. Med Care. 1981 Aug;19(8):872–878. doi: 10.1097/00005650-198108000-00006. [DOI] [PubMed] [Google Scholar]
- Horbar J. D., McAuliffe T. L., Adler S. M., Albersheim S., Cassady G., Edwards W., Jones R., Kattwinkel J., Kraybill E. N., Krishnan V. Variability in 28-day outcomes for very low birth weight infants: an analysis of 11 neonatal intensive care units. Pediatrics. 1988 Oct;82(4):554–559. [PubMed] [Google Scholar]
- Horn S. D. Validity, reliability and implications of an index of inpatient severity of illness. Med Care. 1981 Mar;19(3):354–362. doi: 10.1097/00005650-198103000-00010. [DOI] [PubMed] [Google Scholar]
- Hull D. The viable child. The Croonian lecture 1988. J R Coll Physicians Lond. 1988 Jul;22(3):169–175. [PMC free article] [PubMed] [Google Scholar]
- Knaus W. A., Draper E. A., Wagner D. P., Zimmerman J. E. APACHE II: a severity of disease classification system. Crit Care Med. 1985 Oct;13(10):818–829. [PubMed] [Google Scholar]
- Kraybill E. N., Bose C. L., D'Ercole A. J. Chronic lung disease in infants with very low birth weight. A population-based study. Am J Dis Child. 1987 Jul;141(7):784–788. doi: 10.1001/archpedi.1987.04460070086031. [DOI] [PubMed] [Google Scholar]
- Kwong M. S., Egan E. A., Notter R. H., Shapiro D. L. Double-blind clinical trial of calf lung surfactant extract for the prevention of hyaline membrane disease in extremely premature infants. Pediatrics. 1985 Oct;76(4):585–592. [PubMed] [Google Scholar]
- Maddock C. R. A population-based evaluation of sustained mechanical ventilation of newborn babies. Lancet. 1987 Nov 28;2(8570):1254–1258. doi: 10.1016/s0140-6736(87)91862-9. [DOI] [PubMed] [Google Scholar]
- Maddock C. R., Carpenter R. G., Gardner A. Mechanical ventilation for the newborn. Lancet. 1988 Mar 26;1(8587):707–707. doi: 10.1016/s0140-6736(88)91508-5. [DOI] [PubMed] [Google Scholar]
- Patterson C. C., Halliday H. L. Prediction of outcome shortly after delivery for the very low birthweight (less than or equal to 1500 g) infant. Paediatr Perinat Epidemiol. 1988 Jul;2(3):221–228. doi: 10.1111/j.1365-3016.1988.tb00211.x. [DOI] [PubMed] [Google Scholar]
- Pollack M. M., Ruttimann U. E., Getson P. R. Accurate prediction of the outcome of pediatric intensive care. A new quantitative method. N Engl J Med. 1987 Jan 15;316(3):134–139. doi: 10.1056/NEJM198701153160304. [DOI] [PubMed] [Google Scholar]
- Rojas J., Green R. S., Fannon L., Olssen T., Lindstrom D. P., Stahlman M. T., Cotton R. B. A quantitative model for hyaline membrane disease. Pediatr Res. 1982 Jan;16(1):35–39. doi: 10.1203/00006450-198201001-00007. [DOI] [PubMed] [Google Scholar]
- Saigal S., Rosenbaum P., Hattersley B., Milner R. Decreased disability rate among 3-year-old survivors weighing 501 to 1000 grams at birth and born to residents of a geographically defined region from 1981 to 1984 compared with 1977 to 1980. J Pediatr. 1989 May;114(5):839–846. doi: 10.1016/s0022-3476(89)80150-7. [DOI] [PubMed] [Google Scholar]
- Stewart A. L., Reynolds E. O., Lipscomb A. P. Outcome for infants of very low birthweight: survey of world literature. Lancet. 1981 May 9;1(8228):1038–1040. doi: 10.1016/s0140-6736(81)92198-x. [DOI] [PubMed] [Google Scholar]
- Tarnow-Mordi W. O., Narang A., Wilkinson A. R. Lack of association between barotrauma and air leak in hyaline membrane disease. Arch Dis Child. 1985 Jun;60(6):555–559. doi: 10.1136/adc.60.6.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarnow-Mordi W., Wilkinson A. Mechanical ventilation of the newborn. Br Med J (Clin Res Ed) 1986 Mar 1;292(6520):575–576. doi: 10.1136/bmj.292.6520.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu V. Y., Loke H. L., Bajuk B., Szymonowicz W., Orgill A. A., Astbury J. Prognosis for infants born at 23 to 28 weeks' gestation. Br Med J (Clin Res Ed) 1986 Nov 8;293(6556):1200–1203. doi: 10.1136/bmj.293.6556.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]


