Introduction
Accessory spleen is a variation of spleen development.[1] The most common location of an accessory spleen is at the splenic hilum.[1–3] Wandering accessory spleens may mimic tumors, such as pancreatic tumor, adnexal tumor, abdominal tumor, retroperitoneal tumor, adrenal tumor, or testicular tumor, according to its location.[1–7] Accessory spleens are usually smaller than 3 cm. However, in this patient it is larger than 6 cm. These wandering accessory spleens are indicated for surgery when there are symptoms, such as pain, rupture, infarction, or vascular torsion.[1–4]
Case Report
A 41-year-old man had a health examination in China Medical University Hospital, Taichung, Taiwan, in January 2004. Abdominal sonography was performed, and a left suprarenal tumor about 7 cm in diameter was noted. The serum cortisol level (12.3 mcg/dL at 8 am and 4.35 mcg/dL at 4 pm), the serum adrenocorticotropic hormone level (40.55 pg/dL), the 24-hour urine vanillylmandelic acid level (3.52 mg/dL), and the plasma renin activity were within the normal range. Computed tomography (CT) and magnetic resonance imaging (MRI) were arranged and showed a 7-cm × 6-cm tumor at the upper pole of the left kidney. The kidney axis was deviated because of tumor compression. Cancer of the adrenal gland was suspected.
Laparoscopic resection was arranged to treat the tumor. A purple, smooth-surface tumor was found at the suprarenal area in the retroperitoneal space just above the kidney during the operation. After dissecting the surrounding tissues, a feeding artery from the descending aorta was noted. The accessory spleen was impressed and the pathological report confirmed the diagnosis.
Discussions
There are variants of spleen development, such as splenic clefts, notches, lobulations, an accessory spleen, polysplenia, and wandering spleen.[1] When an accessory spleen wanders to another place, it may mimic some tumors. Adnexal tumor, pancreatic tumor, retroperitoneal tumor, and testicular tumor had been reported.[1,2,4–6] In this case, it mimics an adrenal carcinoma.
The diagnosis of adrenal carcinoma should always be kept in mind when a solitary adrenal mass is greater than 5 cm in diameter.[8] There is no study mentioned about an accessory spleen greater than 5 cm at the suprarenal area. Typically, an accessory spleen is located at the splenic hilum and is less than 3 cm in diameter.[1–3] This patient had a huge suprarenal tumor about 7 × 6 cm in size. We performed laparoscopic resection for this patient due to the initial diagnosis of adrenal carcinoma, not an accessory spleen.
Treatment of an accessory spleen is controversial. It is usually asymptomatic. When an accessory spleen is located in the abdomen without any symptoms, treatment is not necessary. However, torsion of the pedicle of the wandering accessory spleen may happen and can result in rupture and infarction.[3] Laparoscopic resection to treat the wandering accessory spleen is recommended by some investigators when there is a hematologic problem, such as anemia, or symptoms, such as pain or torsion.[3]
We reported this special image of an accessory spleen mimicking the adrenal carcinoma and suggested that for a homogeneous solid adrenal mass, magnetic resonance angiography (MRA) and damaged red blood cell (RBC) scintigraphy may be indicated to rule out the possibility of an accessory spleen from an adrenal tumor.[3,5,6] For an accessory spleen that requires surgical intervention, MRA is indicated due to the more detailed anatomic structure. For a small asymptomatic accessory spleen, damaged RBC scintigraphy is the most specific evaluation technique.[3] For an asymptomatic accessory spleen that is incidentally discovered during laparoscopic surgery, we suggest that splenectomy should be performed if the accessory spleen still has a chance of torsion and the laparoscopic splenectomy is simple and harmless.
Figure 1.
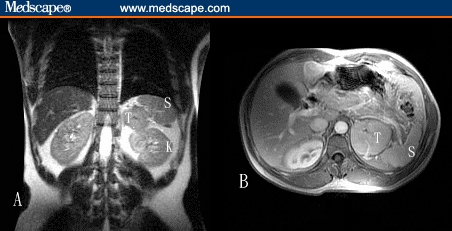
Magnetic resonance image of the left adrenal tumor: (A) coronal section and (B) transverse section (K, = kidney; S = spleen; T = tumor).
Figure 2.
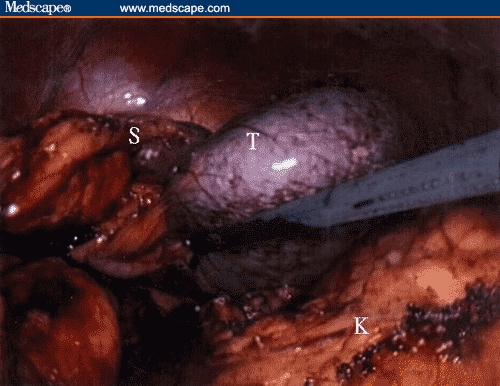
Laparoscopic finding of the suprarenal tumor (K = kidney; S = spleen; T = tumor).
Contributor Information
Chieh-Hsiao Chen, Department of Urology, China Medical University Hospital, Taichung, Taiwan.
Hsi-Chin Wu, Department of Urology, China Medical University Hospital, Taichung, Taiwan.
Chao-Hsiang Chang, Department of Urology, China Medical University Hospital, Taichung, Taiwan. Email: abtchang@www.cmuh.org.tw.
References
- 1.Gayer G, Zissin R, Apter S, Atar E, Portnoy O, Itzchak Y. CT findings in congenital anomalies of the spleen. Br J Radiol. 2001;74:767–772. doi: 10.1259/bjr.74.884.740767. [DOI] [PubMed] [Google Scholar]
- 2.Mortele KJ, Mortele B, Silverman SG. CT features of the accessory spleen. AJR. 2004;183:1653–1657. doi: 10.2214/ajr.183.6.01831653. [DOI] [PubMed] [Google Scholar]
- 3.Velanovich V, Shurafa M. Laparoscopic excision of accessory spleen. Am J Surg. 2000;180:62–64. doi: 10.1016/s0002-9610(00)00417-7. [DOI] [PubMed] [Google Scholar]
- 4.Rosenthal CL, Bishop MC. Accessory spleen presenting as a retroperitoneal tumour. Eur Urol. 1981;7:314–316. doi: 10.1159/000473248. [DOI] [PubMed] [Google Scholar]
- 5.Stiris MG. Accessory spleen versus left adrenal tumor: computed tomographic and abdominal angiographic evaluation. J Computer Assisted Tomography. 1980;4:543–544. doi: 10.1097/00004728-198008000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Tsuchiyaa N, Satoa K, Shimodaa N, et al. An accessory spleen mimicking a nonfunctional adrenal tumor: a potential pitfall in the diagnosis of a left adrenal tumor. Urol Int. 2000;65:226–228. doi: 10.1159/000064885. [DOI] [PubMed] [Google Scholar]
- 7.Kapoor A, Jain A, Mahajan G, Singh A, Bajwa VS, Brar GS. Elusive retroperitoneal accessory spleen. Indian J Surg. 2004;66:298–299. [Google Scholar]
- 8.Campbell MF, Walsh PC, Retik AB, editors. Campell's Urology. 8th ed. New York: WB Saunders & Co.; 2002. pp. 3523–3525. [Google Scholar]


