Abstract
Background: It is difficult to identify the range of gait deviations associated with juvenile idiopathic arthritis (JIA) using simple clinical observations.
Aims: To use objective gait analysis to accurately describe biomechanical gait abnormalities in JIA and to search for common patterns, which may subsequently serve as a basis for therapeutic intervention.
Methods: Children with persistent polyarticular arthritis and symmetrical joint involvement were referred to the Gait Analysis Laboratory and independently assessed by a multidisciplinary team. Gait analysis was performed using an in-house Visual Vector System and the Novel PEDAR in-shoe plantar pressure measurement system. Clinical groupings were based on the extent of joint restriction: minimal (group A), and moderate–severe (with supinatory foot deformity (group B), or with pronatory foot deformity (group C)). Gait analysis enabled classification of each subject into one of four gait patterns: either near normal (pattern I) or one of three adaptive patterns defined by the predominant abnormality—lower limb pain (pattern II), lower limb deformity (pattern III), or a combination of pain and deformity of the lower limb (pattern IV).
Results: Of the 15 subjects assessed as part of this study, seven were placed into clinical group A, six into group B, and two into group C. All the subjects with gait patterns I and II were found in clinical group A. Both subjects from clinical group C exhibited gait pattern III. All subjects from clinical group B and the remainder from group A exhibited a mixture of gait patterns III and IV.
Conclusion: Despite the initial clinical observations it was not always possible to predict the resultant gait pattern. Scientific gait analysis allowed a clear distinction to be made between primary and secondary gait deviations, and accurate targeting of physiotherapy and orthotic interventions to suit each individual. Prospective quantitative analysis in a larger sample is under way to support the clinical effectiveness of these findings.
Full Text
The Full Text of this article is available as a PDF (182.2 KB).
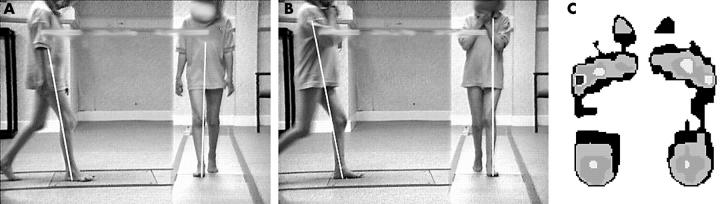
Figure 1 .
VV and PPP data for patient 7. The subject number relates to tables 1, 2, and 3. VV data for both L and R limbs at contralateral final contact shows posterior sagittal vector displacement at the knee—increasing knee flexion during loading response. Patient 7 also displayed associated increased R knee external varus moment, and L knee valgus moment. PPP data illustrated increased hallux and 5th MTH pressure.
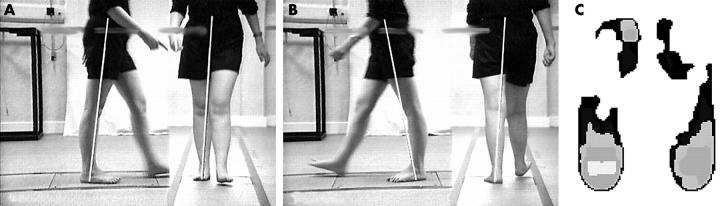
Figure 2 .
VV and PPP data for patient 4. The subject number relates to tables 1, 2, and 3. VV data for both L and R limbs at contralateral initial contact showed posterior sagittal vector displacement in the hindfoot, and anterior displacement at the knee. Bilateral knee joint hyperextension and minimal bilateral forefoot pressures are apparent.
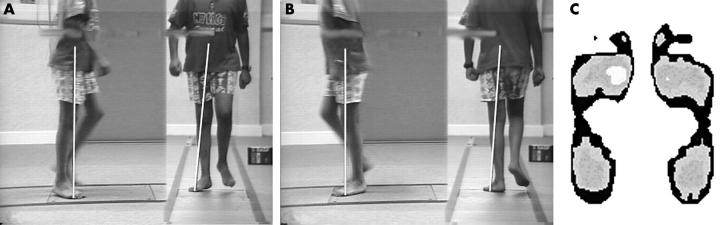
Figure 3 .
VV and PPP data for patient 13. The subject number relates to tables 1, 2, and 3. VV data for both L and R limbs at kinematic midstance showed bilateral forefoot abduction, and anterior medial vector displacement in the forefoot. Anterior sagittal vector displacement at the knee produced an increased external extension moment, and premature heel rise was apparent. PPP data showed increased medial forefoot pressure.
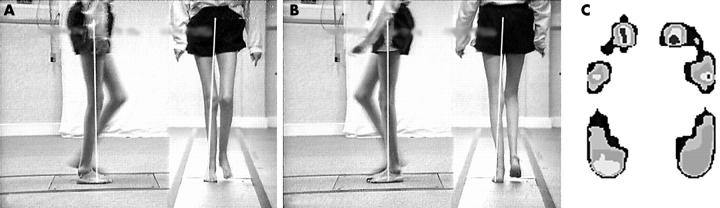
Figure 4 .
VV and PPP data for patient 8. The subject number relates to tables 1, 2, and 3. VV data for both L and R limbs at kinematic midstance showed lateral deviation of the coronal vector in the foot because of excessive supination, and at the knee because of femoral adduction. The latter produced a consequent increase in external valgus moment during stance. PPP data illustrated lateral displacement of pressure distribution, particularly in the MTH region.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dhanendran M., Hutton W. C., Klenerman L., Witemeyer S., Ansell B. M. Foot function in juvenile chronic arthritis. Rheumatol Rehabil. 1980 Feb;19(1):20–24. doi: 10.1093/rheumatology/19.1.20. [DOI] [PubMed] [Google Scholar]
- Lechner D. E., McCarthy C. F., Holden M. K. Gait deviations in patients with juvenile rheumatoid arthritis. Phys Ther. 1987 Sep;67(9):1335–1341. doi: 10.1093/ptj/67.9.1335. [DOI] [PubMed] [Google Scholar]
- Petty R. E., Southwood T. R., Baum J., Bhettay E., Glass D. N., Manners P., Maldonado-Cocco J., Suarez-Almazor M., Orozco-Alcala J., Prieur A. M. Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban, 1997. J Rheumatol. 1998 Oct;25(10):1991–1994. [PubMed] [Google Scholar]
- Southwood T. R. ABC of rheumatology. Arthritis in children. BMJ. 1995 Mar 18;310(6981):728–732. doi: 10.1136/bmj.310.6981.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witemeyer S., Ansell B. M., Ashburn A., Wall J., Klenerman L. Gait analysis: a pilot study- a possible mode of assessment of lower limb function in juvenile chronic arthritis. Rheumatol Rehabil. 1981 Feb 1;20(1):31–37. doi: 10.1093/rheumatology/20.1.31. [DOI] [PubMed] [Google Scholar]