Abstract
Objective: To compare the resistance in vitro of different devices used for the delivery of nasal continuous positive airway pressure (NCPAP) in neonates.
Design: Flows of 4–8 litres/min were passed through a selection of neonatal NCPAP devices (single prong, Duotube, Argyle prong, Hudson prong, Infant Flow Driver), and the resultant fall in pressure measured using a calibrated pressure transducer.
Results: The decrease in pressure (cm H2O) for each device (size in parentheses) at a constant flow of 6 litres/min was: Duotube: (2.5), 21; (3.0), 6.2; (3.5), 2.3; single prong: (2.5), 4.4; (3.0), 2.1; (3.5), 1.2; Argyle prong: (XS), 3.6; (S), 1.9; (L), 1.5; Hudson prong: (0), 3.1; (1), 1.8; (2), 0.6; (3), 0.4; (4), 0.3; Infant Flow Driver: (small), 0.3; (medium), -0.3; (large), -0.5.
Conclusions: A large variation in the potential fall in pressure may occur in the clinical setting. Devices with short double prongs had the lowest resistance to flow. These results have implications in the selection of the optimal device/s for clinical application and for future comparisons in randomised trials of NCPAP in neonates.
Full Text
The Full Text of this article is available as a PDF (134.8 KB).
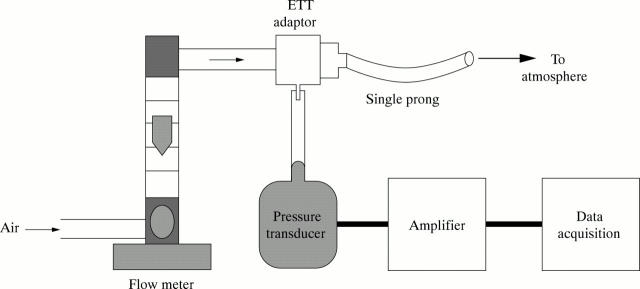
Figure 1 .
Apparatus connected to a single prong device.
Figure 2 .
Pressure measured in nasal continuous positive airway pressure (NCPAP) devices at a flow rate of 6 litres/min. Device sizes are given in parentheses.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahluwalia J. S., White D. K., Morley C. J. Infant Flow Driver or single prong nasal continuous positive airway pressure: short-term physiological effects. Acta Paediatr. 1998 Mar;87(3):325–327. doi: 10.1080/08035259850157408. [DOI] [PubMed] [Google Scholar]
- Caliumi-Pellegrini G., Agostino R., Orzalesi M., Nodari S., Marzetti G., Savignoni P. G., Bucci G. Twin nasal cannula for administration of continuous positive airway pressure to newborn infants. Arch Dis Child. 1974 Mar;49(3):228–230. doi: 10.1136/adc.49.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney S. E., Pyon K. H., Saslow J. G., Arnold G. K., Pandit P. B., Habib R. H. Lung recruitment and breathing pattern during variable versus continuous flow nasal continuous positive airway pressure in premature infants: an evaluation of three devices. Pediatrics. 2001 Feb;107(2):304–308. doi: 10.1542/peds.107.2.304. [DOI] [PubMed] [Google Scholar]
- Field D., Vyas H., Milner A. D., Hopkin I. E. Continuous positive airway pressure via a single nasal catheter in preterm infants. Early Hum Dev. 1985 Sep;11(3-4):275–280. doi: 10.1016/0378-3782(85)90081-7. [DOI] [PubMed] [Google Scholar]
- Goldman S. L., Brady J. P., Dumpit F. M. Increased work of breathing associated with nasal prongs. Pediatrics. 1979 Aug;64(2):160–164. [PubMed] [Google Scholar]
- Gregory G. A., Kitterman J. A., Phibbs R. H., Tooley W. H., Hamilton W. K. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971 Jun 17;284(24):1333–1340. doi: 10.1056/NEJM197106172842401. [DOI] [PubMed] [Google Scholar]
- Gustafson K., Hagberg H., Bengtsson B. A., Brantsing C., Isgaard J. Possible protective role of growth hormone in hypoxia-ischemia in neonatal rats. Pediatr Res. 1999 Mar;45(3):318–323. doi: 10.1203/00006450-199903000-00005. [DOI] [PubMed] [Google Scholar]
- Jarreau P. H., Louis B., Dassieu G., Desfrere L., Blanchard P. W., Moriette G., Isabey D., Harf A. Estimation of inspiratory pressure drop in neonatal and pediatric endotracheal tubes. J Appl Physiol (1985) 1999 Jul;87(1):36–46. doi: 10.1152/jappl.1999.87.1.36. [DOI] [PubMed] [Google Scholar]
- Kattwinkel J., Fleming D., Cha C. C., Fanaroff A. A., Klaus M. H. A device for administration of continuous positive airway pressure by the nasal route. Pediatrics. 1973 Jul;52(1):131–134. [PubMed] [Google Scholar]
- Kattwinkel J., Nearman H. S., Fanaroff A. A., Katona P. G., Klaus M. H. Apnea of prematurity. Comparative therapeutic effects of cutaneous stimulation and nasal continuous positive airway pressure. J Pediatr. 1975 Apr;86(4):588–592. doi: 10.1016/s0022-3476(75)80158-2. [DOI] [PubMed] [Google Scholar]
- Kavvadia V., Greenough A., Dimitriou G. Effect on lung function of continuous positive airway pressure administered either by infant flow driver or a single nasal prong. Eur J Pediatr. 2000 Apr;159(4):289–292. doi: 10.1007/s004310050072. [DOI] [PubMed] [Google Scholar]
- Loftus B. C., Ahn J., Haddad J., Jr Neonatal nasal deformities secondary to nasal continuous positive airway pressure. Laryngoscope. 1994 Aug;104(8 Pt 1):1019–1022. doi: 10.1288/00005537-199408000-00018. [DOI] [PubMed] [Google Scholar]
- Moa G., Nilsson K., Zetterström H., Jonsson L. O. A new device for administration of nasal continuous positive airway pressure in the newborn: an experimental study. Crit Care Med. 1988 Dec;16(12):1238–1242. doi: 10.1097/00003246-198812000-00013. [DOI] [PubMed] [Google Scholar]
- Novogroder M., MacKuanying N., Eidelman A. I., Gartner L. M. Nasopharyngeal ventilation in respiratory distress syndrome. A simple and efficient method of delivering continuous positive airway pressure. J Pediatr. 1973 Jun;82(6):1059–1062. doi: 10.1016/s0022-3476(73)80447-0. [DOI] [PubMed] [Google Scholar]
- Robertson N. J., McCarthy L. S., Hamilton P. A., Moss A. L. Nasal deformities resulting from flow driver continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 1996 Nov;75(3):F209–F212. doi: 10.1136/fn.75.3.f209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speidel B. D., Dunn P. M. Use of nasal continuous positive airway pressure to treat severe recurrent apnoea in very preterm infants. Lancet. 1976 Sep 25;2(7987):658–660. doi: 10.1016/s0140-6736(76)92468-5. [DOI] [PubMed] [Google Scholar]
- Wall M. A. Infant endotracheal tube resistance: effects of changing length, diameter, and gas density. Crit Care Med. 1980 Jan;8(1):38–40. [PubMed] [Google Scholar]
- Wung J. T., Driscoll J. M., Jr, Epstein R. A., Hyman A. I. A new device for CPAP by nasal route. Crit Care Med. 1975 Mar-Apr;3(2):76–78. doi: 10.1097/00003246-197503000-00006. [DOI] [PubMed] [Google Scholar]