Abstract
AIMS/BACKGROUND—The aim of this study was to assess the morbidity associated with harvesting autogenous fascia lata for brow suspension ptosis surgery. METHODS—A retrospective study by postal questionnaire of 24 consecutive patients. RESULTS—Early postoperative problems with pain on walking (67%), limping (38%), and wound pain (57%) occurred mostly for less than 1 week. The final cosmetic appearance of the scar caused minor concern in 38% of patients. CONCLUSION—Fascia lata is the preferred material for permanent ptosis correction when a brow suspension is required. Most of the patients, following fascia lata harvest, experienced some symptoms of leg pain and limping for less than 1 week. The only long term problem was the scar. 38% of patients found the final cosmetic appearance caused minor concern.
Full Text
The Full Text of this article is available as a PDF (68.4 KB).
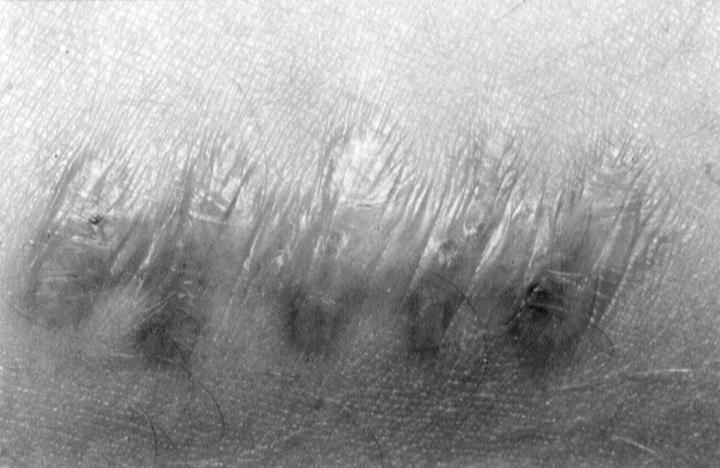
Figure 1 .
A leg scar with a poor cosmetic result from harvesting fascia lata.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Crawford J. S., Doucet T. W. Uses of fascia in ophthalmology and the benefits of autogenous sources. J Pediatr Ophthalmol Strabismus. 1982 Jul-Aug;19(4):21–25. doi: 10.3928/0191-3913-19820701-07. [DOI] [PubMed] [Google Scholar]
- Crawford J. S. Fascia lata: its nature and fate after implantation and its use in ophthalmic surgery. Trans Am Ophthalmol Soc. 1968;66:673–745. [PMC free article] [PubMed] [Google Scholar]
- Crawford J. S. Repair of ptosis using frontalis muscle and fascia lata: a 20-year review. Ophthalmic Surg. 1977 Aug;8(4):31–40. [PubMed] [Google Scholar]
- Dubiel W. T., Wigren A. Functional status of the lower extremity after resection of fascia lata. A clinical and physiological follow-up study in patients with fascia lata heart valve replacement. Acta Orthop Scand. 1974;45(4):599–613. doi: 10.3109/17453677408989183. [DOI] [PubMed] [Google Scholar]
- Fox S. A. Complications of frontalis sling surgery. Am J Ophthalmol. 1967 Apr;63(4):758–762. doi: 10.1016/0002-9394(67)91302-5. [DOI] [PubMed] [Google Scholar]
- Hintschich C. R., Zürcher M., Collin J. R. Mersilene mesh brow suspension: efficiency and complications. Br J Ophthalmol. 1995 Apr;79(4):358–361. doi: 10.1136/bjo.79.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leone C. R., Jr, Shore J. W., Van Gemert J. V. Silicone rod frontalis sling for the correction of blepharoptosis. Ophthalmic Surg. 1981 Dec;12(12):881–887. [PubMed] [Google Scholar]
- Manners R. M., Tyers A. G., Morris R. J. The use of Prolene as a temporary suspensory material for brow suspension in young children. Eye (Lond) 1994;8(Pt 3):346–348. doi: 10.1038/eye.1994.72. [DOI] [PubMed] [Google Scholar]
- Wagner R. S., Mauriello J. A., Jr, Nelson L. B., Calhoun J. H., Flanagan J. C., Harley R. D. Treatment of congenital ptosis with frontalis suspension: a comparison of suspensory materials. Ophthalmology. 1984 Mar;91(3):245–248. doi: 10.1016/s0161-6420(84)34298-1. [DOI] [PubMed] [Google Scholar]
- Wilson M. E., Johnson R. W. Congenital ptosis. Long-term results of treatment using lyophilized fascia lata for frontalis suspensions. Ophthalmology. 1991 Aug;98(8):1234–1237. [PubMed] [Google Scholar]
- Zweep H. P., Spauwen P. H. Evaluation of expanded polytetrafluoroethylene (e-PTFE) and autogenous fascia lata in frontalis suspension. A comparative clinical study. Acta Chir Plast. 1992;34(3):129–137. [PubMed] [Google Scholar]