Abstract
AIM—To compare the frequency and site of visual field progression and changes in visual acuity in patients with normal pressure glaucoma (NPG) with and without pre-existing visual field loss. METHOD—Patients with normal tension glaucoma were selected who had at least 10 visual fields over 5 or more years of follow up and no other condition that might influence the visual field or visual acuity. Alternate left and right eyes were selected from patients in random order. These eyes were then subdivided according to visual field defect threatening fixation, visual field defect not threatening fixation, and no visual field defect (fellow eyes). Eyes were defined as showing a threat to fixation according to the presence of a visual field defect involving one of more of four paracentral visual field locations. Pointwise linear regression analysis was applied to each visual field series using PROGRESSOR software. Progression of visual field loss was defined as the appearance of a regression slope 1 dB per year or more with a significance of p<0.01, which remained consistent with the addition of two of three successive visual fields to the series. The number of patients showing progression and the number where progression occurred in one of the four paracentral visual field locations was noted. The number of eyes losing two or more lines of Snellen visual acuity over the follow up period was also noted. RESULTS—174 eyes of 174 patients were selected. 106 eyes had visual field loss threatening fixation, 46 eyes had visual field loss that did not threaten fixation, and 22 were fellow eyes with normal visual fields. The median follow up was 7.2 years. Eight eyes (36.4%) in the "normal visual fields" group, 31 eyes (67.4%) in the "visual field loss away from fixation" group, and 87 eyes (82.1%) in the "threat to fixation" group showed progression in any part of the visual field. Two eyes (9.1%) in the "normal visual fields" group, nine eyes (19.6%) in the "visual field loss away from fixation" group, and 45 eyes (42.5%) in the "threat to fixation" group showed progression at "threat to fixation". The Cox proportional hazards regression model showed an increased risk of progression at any part of the visual field for female sex and a decreased risk for eyes with normal visual fields. For progression at threat to fixation this model showed an increased risk with pre-existing threat to fixation. Eyes from older patients and those that went on to have progressive visual field loss at fixation were more likely to lose two lines of Snellen visual acuity over the follow up period. CONCLUSION—Since 20-30% of previously field damaged eyes and over 60% without prior field loss fail to demonstrate progressive visual field damage over a long follow up it is recommended that normal pressure glaucoma patients be monitored for progression and that potentially harmful therapy be withheld until progression is demonstrated. Although the presence of visual field loss that threatens fixation does not constitute an increased risk of visual field progression it does indicate an increased risk of further loss of visual field close to fixation which is in turn associated with loss of central acuity. In the light of this finding, patients with visual field loss that threatens fixation should be managed more aggressively.
Full Text
The Full Text of this article is available as a PDF (155.7 KB).
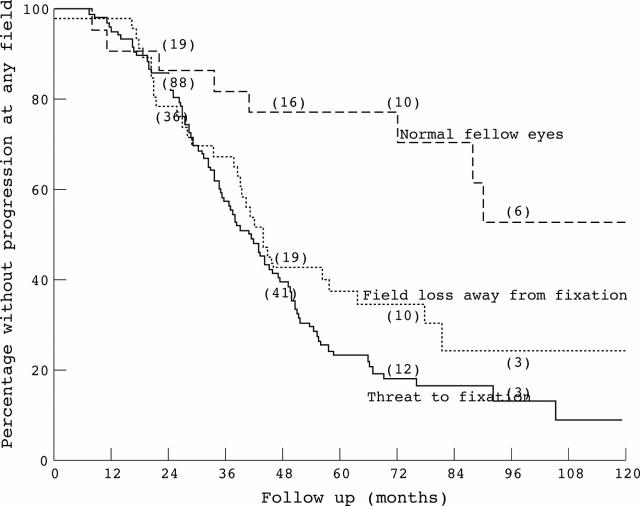
Figure 1 .
Survivals plot where survival is defined as lack of progression at any field location, groups defined by initial field group. (n=number surviving.)
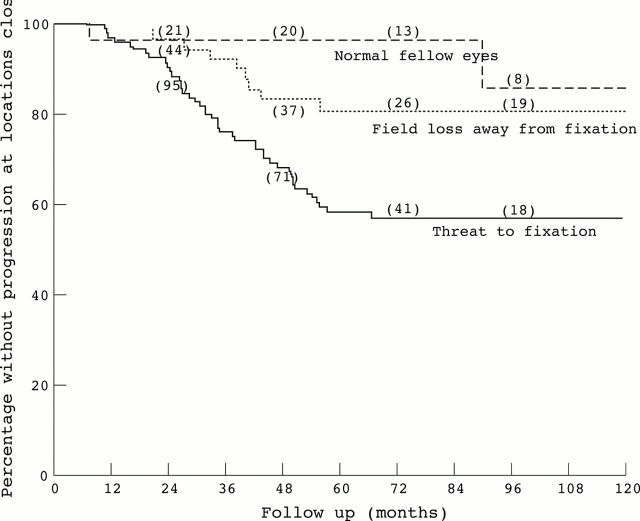
Figure 2 .
Survival plot where survival is defined as lack of progression at locations close to fixation, groups defined by initial field group. (n=number surviving.)
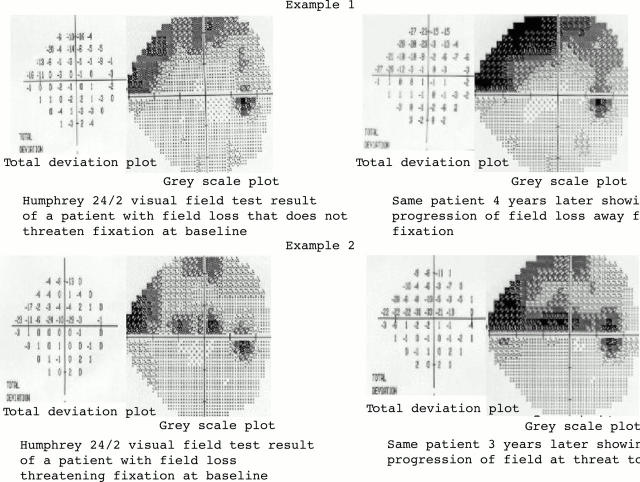
Figure 3 .
Humphrey 24/2 visual fields from two patients. Example 1 is of a patient with visual field loss away from fixation at the start of follow up (top left) who shows progression away from fixation at the end of a 4 year follow up period (top right). Example 2 is of a patient with visual field loss threatening fixation at the start of follow up (bottom left) who shows progression at threat to fixation at the end of a 3 year follow up period (bottom right).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Araie M., Kitazawa M., Koseki N. Intraocular pressure and central visual field of normal tension glaucoma. Br J Ophthalmol. 1997 Oct;81(10):852–856. doi: 10.1136/bjo.81.10.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araie M., Yamagami J., Suziki Y. Visual field defects in normal-tension and high-tension glaucoma. Ophthalmology. 1993 Dec;100(12):1808–1814. doi: 10.1016/s0161-6420(93)31394-1. [DOI] [PubMed] [Google Scholar]
- Bonomi L., Marchini G., Marraffa M., Bernardi P., De Franco I., Perfetti S., Varotto A., Tenna V. Prevalence of glaucoma and intraocular pressure distribution in a defined population. The Egna-Neumarkt Study. Ophthalmology. 1998 Feb;105(2):209–215. doi: 10.1016/s0161-6420(98)92665-3. [DOI] [PubMed] [Google Scholar]
- Caprioli J., Sears M., Miller J. M. Patterns of early visual field loss in open-angle glaucoma. Am J Ophthalmol. 1987 Apr 15;103(4):512–517. doi: 10.1016/s0002-9394(14)74273-4. [DOI] [PubMed] [Google Scholar]
- Caprioli J., Spaeth G. L. Comparison of visual field defects in the low-tension glaucomas with those in the high-tension glaucomas. Am J Ophthalmol. 1984 Jun;97(6):730–737. doi: 10.1016/0002-9394(84)90505-1. [DOI] [PubMed] [Google Scholar]
- Coffey M., Reidy A., Wormald R., Xian W. X., Wright L., Courtney P. Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol. 1993 Jan;77(1):17–21. doi: 10.1136/bjo.77.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dielemans I., Vingerling J. R., Wolfs R. C., Hofman A., Grobbee D. E., de Jong P. T. The prevalence of primary open-angle glaucoma in a population-based study in The Netherlands. The Rotterdam Study. Ophthalmology. 1994 Nov;101(11):1851–1855. doi: 10.1016/s0161-6420(94)31090-6. [DOI] [PubMed] [Google Scholar]
- Fitzke F. W., Hitchings R. A., Poinoosawmy D., McNaught A. I., Crabb D. P. Analysis of visual field progression in glaucoma. Br J Ophthalmol. 1996 Jan;80(1):40–48. doi: 10.1136/bjo.80.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gliklich R. E., Steinmann W. C., Spaeth G. L. Visual field change in low-tension glaucoma over a five-year follow-up. Ophthalmology. 1989 Mar;96(3):316–320. doi: 10.1016/s0161-6420(89)33070-3. [DOI] [PubMed] [Google Scholar]
- Hitchings R. A., Anderton S. A. A comparative study of visual field defects seen in patients with low-tension glaucoma and chronic simple glaucoma. Br J Ophthalmol. 1983 Dec;67(12):818–821. doi: 10.1136/bjo.67.12.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamal D., Hitchings R. Normal tension glaucoma--a practical approach. Br J Ophthalmol. 1998 Jul;82(7):835–840. doi: 10.1136/bjo.82.7.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolker A. E. Visual prognosis in advanced glaucoma: a comparison of medical and surgical therapy for retention of vision in 101 eyes with advanced glaucoma. Trans Am Ophthalmol Soc. 1977;75:539–555. [PMC free article] [PubMed] [Google Scholar]
- Koseki N., Araie M., Suzuki Y., Yamagami J. Visual field damage proximal to fixation in normal- and high-tension glaucoma eyes. Jpn J Ophthalmol. 1995;39(3):274–283. [PubMed] [Google Scholar]
- Lachenmayr B. J., Drance S. M. Central function and visual field damage in glaucoma. Int Ophthalmol. 1992 Sep;16(4-5):203–209. doi: 10.1007/BF00917962. [DOI] [PubMed] [Google Scholar]
- McNaught A. I., Crabb D. P., Fitzke F. W., Hitchings R. A. Modelling series of visual fields to detect progression in normal-tension glaucoma. Graefes Arch Clin Exp Ophthalmol. 1995 Dec;233(12):750–755. doi: 10.1007/BF00184085. [DOI] [PubMed] [Google Scholar]
- McNaught A. I., Crabb D. P., Fitzke F. W., Hitchings R. A. Visual field progression: comparison of Humphrey Statpac2 and pointwise linear regression analysis. Graefes Arch Clin Exp Ophthalmol. 1996 Jul;234(7):411–418. doi: 10.1007/BF02539406. [DOI] [PubMed] [Google Scholar]
- Viswanathan A. C., Fitzke F. W., Hitchings R. A. Early detection of visual field progression in glaucoma: a comparison of PROGRESSOR and STATPAC 2. Br J Ophthalmol. 1997 Dec;81(12):1037–1042. doi: 10.1136/bjo.81.12.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiter J. H., Shin D. H., Juzych M. S., Jarvi T. S., Spoor T. C., Zwas F. Visual field defects in patients with normal-tension glaucoma and patients with high-tension glaucoma. Am J Ophthalmol. 1992 Dec 15;114(6):758–763. doi: 10.1016/s0002-9394(14)74056-5. [DOI] [PubMed] [Google Scholar]
- Zhang L., Drance S. M., Douglas G. R. Automated perimetry in detecting threats to fixation. Ophthalmology. 1997 Nov;104(11):1918–1920. doi: 10.1016/s0161-6420(97)30007-4. [DOI] [PubMed] [Google Scholar]