Abstract
OBJECTIVE—To investigate the hypothesis that in coronary artery disease large plaques in compensatorily enlarged segments are associated with acute coronary syndromes, whereas smaller plaques in shrunken segments are associated with stable angina pectoris. METHODS—Patients selected for percutaneous transluminal coronary angioplasty (PTCA) were divided into two groups, one with stable angina pectoris (stable group, n = 37) and one with unstable angina or postmyocardial infarction angina of the infarct related artery (unstable group, n = 32). In both groups, remodelling at the culprit lesion site was determined by intravascular ultrasound before the intervention. Remodelling was calculated as relative vessel area: [vessel area culprit lesion site ÷ mean vessel area of both proximal and distal reference sites] × 100%. Compensatory enlargement was defined as remodelling of ⩾ 105%, whereas shrinkage was defined as remodelling of ⩽ 95%. RESULTS—In the unstable group, the vessel area at the culprit lesion site was larger than in the stable group, at mean (SD) 18.1 (5.3) v 14.6 (5.4) mm2 (p = 0.008). Lumen areas were similar. Consequently, plaque area and percentage remodelling were larger in the unstable group than in the stable group: mean (SD) 14.8 (4.8) v 11.6 (4.9) mm2 (p = 0.009) and 112 (31)% v 95 (17)% (p = 0.005), respectively. Significantly more culprit lesion sites were classified as shrunken in the stable group (21/37) than in the unstable group (8/32; p = 0.014). On the other hand, more lesion sites were classified as enlarged in the unstable group (16/23) than in the stable group (8/37; p = 0.022). CONCLUSIONS—In patients selected for PTCA, the mode of remodelling is related to clinical presentation. Keywords: atherosclerosis; coronary disease; remodelling; intravascular ultrasound
Full Text
The Full Text of this article is available as a PDF (91.7 KB).
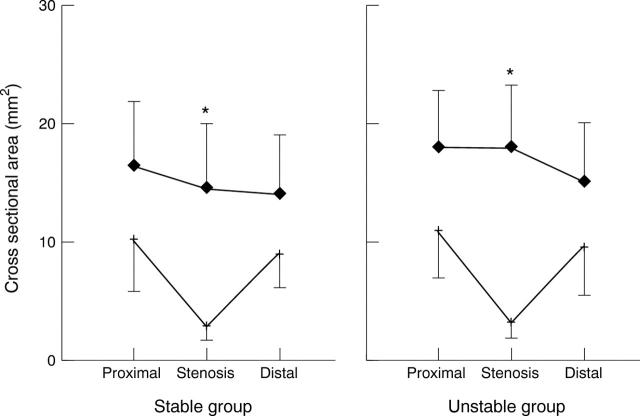
Figure 1 .
Mean cross sectional area values of lumen (+) and vessel (♦) at the proximal reference, stenosis, and distal reference sites in the two groups of patients. Error bars are standard deviations. Only vessel area at the stenosis site (*) was significantly different between the groups: 14.6 (5.4) v 18.1 (5.3) mm2 (p = 0.008).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ambrose J. A., Tannenbaum M. A., Alexopoulos D., Hjemdahl-Monsen C. E., Leavy J., Weiss M., Borrico S., Gorlin R., Fuster V. Angiographic progression of coronary artery disease and the development of myocardial infarction. J Am Coll Cardiol. 1988 Jul;12(1):56–62. doi: 10.1016/0735-1097(88)90356-7. [DOI] [PubMed] [Google Scholar]
- Braunwald E. Unstable angina. A classification. Circulation. 1989 Aug;80(2):410–414. doi: 10.1161/01.cir.80.2.410. [DOI] [PubMed] [Google Scholar]
- Falk E. Plaque rupture with severe pre-existing stenosis precipitating coronary thrombosis. Characteristics of coronary atherosclerotic plaques underlying fatal occlusive thrombi. Br Heart J. 1983 Aug;50(2):127–134. doi: 10.1136/hrt.50.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M. C., Siegel R. J. How big are coronary atherosclerotic plaques that rupture? Circulation. 1996 Nov 15;94(10):2662–2666. doi: 10.1161/01.cir.94.10.2662. [DOI] [PubMed] [Google Scholar]
- Glagov S., Weisenberg E., Zarins C. K., Stankunavicius R., Kolettis G. J. Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med. 1987 May 28;316(22):1371–1375. doi: 10.1056/NEJM198705283162204. [DOI] [PubMed] [Google Scholar]
- Horie T., Sekiguchi M., Hirosawa K. Coronary thrombosis in pathogenesis of acute myocardial infarction. Histopathological study of coronary arteries in 108 necropsied cases using serial section. Br Heart J. 1978 Feb;40(2):153–161. doi: 10.1136/hrt.40.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearney P., Erbel R., Rupprecht H. J., Ge J., Koch L., Voigtländer T., Stähr P., Görge G., Meyer J. Differences in the morphology of unstable and stable coronary lesions and their impact on the mechanisms of angioplasty. An in vivo study with intravascular ultrasound. Eur Heart J. 1996 May;17(5):721–730. doi: 10.1093/oxfordjournals.eurheartj.a014939. [DOI] [PubMed] [Google Scholar]
- Kragel A. H., Gertz S. D., Roberts W. C. Morphologic comparison of frequency and types of acute lesions in the major epicardial coronary arteries in unstable angina pectoris, sudden coronary death and acute myocardial infarction. J Am Coll Cardiol. 1991 Sep;18(3):801–808. doi: 10.1016/0735-1097(91)90805-j. [DOI] [PubMed] [Google Scholar]
- Kragel A. H., Reddy S. G., Wittes J. T., Roberts W. C. Morphometric analysis of the composition of atherosclerotic plaques in the four major epicardial coronary arteries in acute myocardial infarction and in sudden coronary death. Circulation. 1989 Dec;80(6):1747–1756. doi: 10.1161/01.cir.80.6.1747. [DOI] [PubMed] [Google Scholar]
- Little W. C., Constantinescu M., Applegate R. J., Kutcher M. A., Burrows M. T., Kahl F. R., Santamore W. P. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988 Nov;78(5 Pt 1):1157–1166. doi: 10.1161/01.cir.78.5.1157. [DOI] [PubMed] [Google Scholar]
- Mann J. M., Davies M. J. Assessment of the severity of coronary artery disease at postmortem examination. Are the measurements clinically valid? Br Heart J. 1995 Nov;74(5):528–530. doi: 10.1136/hrt.74.5.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mintz G. S., Kent K. M., Pichard A. D., Satler L. F., Popma J. J., Leon M. B. Contribution of inadequate arterial remodeling to the development of focal coronary artery stenoses. An intravascular ultrasound study. Circulation. 1997 Apr 1;95(7):1791–1798. doi: 10.1161/01.cir.95.7.1791. [DOI] [PubMed] [Google Scholar]
- Moreno P. R., Falk E., Palacios I. F., Newell J. B., Fuster V., Fallon J. T. Macrophage infiltration in acute coronary syndromes. Implications for plaque rupture. Circulation. 1994 Aug;90(2):775–778. doi: 10.1161/01.cir.90.2.775. [DOI] [PubMed] [Google Scholar]
- Nishioka T., Luo H., Eigler N. L., Berglund H., Kim C. J., Siegel R. J. Contribution of inadequate compensatory enlargement to development of human coronary artery stenosis: an in vivo intravascular ultrasound study. J Am Coll Cardiol. 1996 Jun;27(7):1571–1576. doi: 10.1016/0735-1097(96)00071-x. [DOI] [PubMed] [Google Scholar]
- Pasterkamp G., Borst C., Gussenhoven E. J., Mali W. P., Post M. J., The S. H., Reekers J. A., van den Berg F. G. Remodeling of De Novo atherosclerotic lesions in femoral arteries: impact on mechanism of balloon angioplasty. J Am Coll Cardiol. 1995 Aug;26(2):422–428. doi: 10.1016/0735-1097(95)80017-b. [DOI] [PubMed] [Google Scholar]
- Pasterkamp G., Schoneveld A. H., van Wolferen W., Hillen B., Clarijs R. J., Haudenschild C. C., Borst C. The impact of atherosclerotic arterial remodeling on percentage of luminal stenosis varies widely within the arterial system. A postmortem study. Arterioscler Thromb Vasc Biol. 1997 Nov;17(11):3057–3063. doi: 10.1161/01.atv.17.11.3057. [DOI] [PubMed] [Google Scholar]
- Pasterkamp G., Schoneveld A. H., van der Wal A. C., Haudenschild C. C., Clarijs R. J., Becker A. E., Hillen B., Borst C. Relation of arterial geometry to luminal narrowing and histologic markers for plaque vulnerability: the remodeling paradox. J Am Coll Cardiol. 1998 Sep;32(3):655–662. doi: 10.1016/s0735-1097(98)00304-0. [DOI] [PubMed] [Google Scholar]
- Pasterkamp G., Wensing P. J., Hillen B., Post M. J., Mali W. P., Borst C. Impact of local atherosclerotic remodeling on the calculation of percent luminal narrowing. Am J Cardiol. 1997 Feb 15;79(4):402–405. doi: 10.1016/s0002-9149(96)00775-8. [DOI] [PubMed] [Google Scholar]
- Pasterkamp G., Wensing P. J., Post M. J., Hillen B., Mali W. P., Borst C. Paradoxical arterial wall shrinkage may contribute to luminal narrowing of human atherosclerotic femoral arteries. Circulation. 1995 Mar 1;91(5):1444–1449. doi: 10.1161/01.cir.91.5.1444. [DOI] [PubMed] [Google Scholar]
- Potkin B. N., Bartorelli A. L., Gessert J. M., Neville R. F., Almagor Y., Roberts W. C., Leon M. B. Coronary artery imaging with intravascular high-frequency ultrasound. Circulation. 1990 May;81(5):1575–1585. doi: 10.1161/01.cir.81.5.1575. [DOI] [PubMed] [Google Scholar]
- Qiao J. H., Fishbein M. C. The severity of coronary atherosclerosis at sites of plaque rupture with occlusive thrombosis. J Am Coll Cardiol. 1991 Apr;17(5):1138–1142. doi: 10.1016/0735-1097(91)90844-y. [DOI] [PubMed] [Google Scholar]
- Smits P. C., Bos L., Quarles van Ufford M. A., Eefting F. D., Pasterkamp G., Borst C. Shrinkage of human coronary arteries is an important determinant of de novo atherosclerotic luminal stenosis: an in vivo intravascular ultrasound study. Heart. 1998 Feb;79(2):143–147. doi: 10.1136/hrt.79.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenguang L., Gussenhoven W. J., Zhong Y., The S. H., Di Mario C., Madretsma S., van Egmond F., de Feyter P., Pieterman H., van Urk H. Validation of quantitative analysis of intravascular ultrasound images. Int J Card Imaging. 1991;6(3-4):247–253. doi: 10.1007/BF01797856. [DOI] [PubMed] [Google Scholar]
- van der Wal A. C., Becker A. E., van der Loos C. M., Das P. K. Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation. 1994 Jan;89(1):36–44. doi: 10.1161/01.cir.89.1.36. [DOI] [PubMed] [Google Scholar]