Abstract
Primary cardiac sarcomas are rare. In such tumors, surgical resection is sometimes considered necessary to correct obstruction of flow caused by the tumor and to accomplish complete resection. The anatomic difficulties associated with large, primary, intracavitary left-sided sarcomas have led us to use cardiac explantation, ex vivo tumor resection, and cardiac autotransplantation to meet the anatomic challenges of left atrial tumors.
We report the case of a patient who had a large, primary, intracavitary, left ventricular sarcoma that was successfully removed by cardiac explantation and ex vivo reconstruction with use of the cardiac autotransplantation technique. This is the 1st report describing the use of cardiac autotransplantation to surgically resect an intracavitary left ventricular malignancy.
Key words: Cardiac surgical; procedures/methods; heart neoplasms/primary/surgery; heart ventricles/surgery; sarcoma/surgery; transplantation, autologous/methods
Primary cardiac neoplasms are rare. Of the primary cardiac tumors reported, 25% are malignant, and 75% of these malignant tumors are sarcomas.1,2 Cardiac sarcomas often respond poorly to chemotherapy, and death is frequently due to obstruction of blood flow as a result of the anatomic location of the tumor. Consequently, surgical resection should be considered for those patients who have obstructive symptoms and in whom complete resection may achieve tumor eradication. The crucial problems facing the cardiac surgeon in these patients are the dificult anatomic locations of the tumors and the need to resect the affected myocardium while preserving overall cardiac function. Large left atrial primary sarcomas are often the most challenging for the cardiac surgeon, because achieving anatomic exposure of this location is dificult. This technical challenge led us to irst successfully use the approach of explantation of the heart with ex vivo resection of the tumor, reconstruction of the heart, and cardiac autotransplantation to treat these tumors.1
We present the case of a young patient who had a large, primary, intracavitary, left ventricular tumor that was thought to be a sarcoma. Because of its dificult location, large size, and impending left ventricular outflow tract obstruction, we performed surgical excision using the cardiac autotransplantation technique.
Case Report
A 31-year-old woman who had a long, symptom-free history of mitral regurgitation had been observed yearly with echocardiography for about 10 years. The patient's early history included treatment for Stage IIB Hodgkin's disease at 8 years of age. This therapy involved chemotherapy, and irradiation of the neck, mediastinum, and inverted “Y” lower mantle. After treatment, she remained free of Hodgkin's disease; however, she developed both pulmonary ibrosis and the aforementioned mitral insuficiency.
One year before the surgery discussed herein, echocardiography revealed a small mass at the base of her posterior medial papillary muscle, which was followed clinically with repeat echocardiograms. An echocardiogram done 1 month before hospital admission revealed a large left ventricular mass approximately 3 cm in size (Fig. 1). Cardiac magnetic resonance imaging showed a soft-tissue lesion involving the basal and mid-interventricular septum with anterior–superior extension. The lesion was polypoid in nature and extended superiorly into the left ventricular outflow tract. These indings were considered most consistent with a left ventricular neoplasm, likely a sarcoma. Abdominal and chest computed tomographic scans showed no other masses. A positron-emission tomographic scan revealed no disease outside the region of the heart.
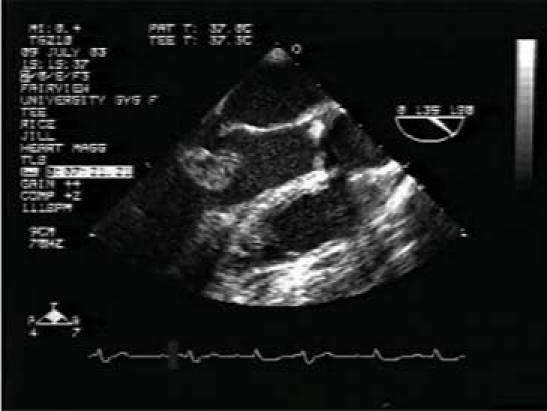
Fig. 1 Echocardiogram shows a 3-cm left ventricular mass.
With impending left ventricular outflow tract obstruction and no evidence of metastatic disease, the patient underwent surgery in September 2003. Through a standard median sternotomy, we performed direct cannulation of the superior vena cava–inferior vena cava lateral junction and of the distal ascending aorta. This enabled the institution of cardiopulmonary bypass. Caval tapes were placed around the superior vena cava and inferior vena cava. The ascending aorta and pulmonary artery were dissected free of one another. The ascending aorta was cross-clamped and antegrade cardioplegic solution was given. The aorta was then divided in a transverse fashion, approximately 1 cm distal to the sinotubular junction. This allowed retraction of the aortic valve and visualization of the tumor, for a possible transaortic resection. The tumor was very large; therefore, resection through a small aortic root was not feasible. The superior vena cava and inferior vena cava were then transected, the pulmonary artery was transected just proximal to the bifurcation, and the left atrium was opened in the interatrial groove. The incision was extended just anterior to the left pulmonary veins and just behind the atrial appendage and mitral valve. This enabled complete explantation of the heart, which was placed in a basin of iced saline solution. The anterior leaflet of the mitral valve was initially taken down to expose the tumor, which could then be seen to extensively iniltrate the base of the posterior medial papillary muscle (Fig. 2). Therefore, the anterior leaflet of the mitral valve was excised, along with the posterior medial papillary muscle and the interventricular septum at its base. The septum was repaired with bovine pericardium, and the mitral valve was replaced with a 25-mm St. Jude Medical® mechanical mitral valve (St. Jude Medical, Inc.; St. Paul, Minn) (Fig. 3). The heart was then reimplanted, warm blood potassium cardioplegic solution was given using antegrade delivery, and the cross-clamp was removed. Spontaneous cardiac activity resumed. The patient's postoperative course was uneventful, and she was discharged from the hospital on the 12th postoperative day. Final histopathology revealed a primary cardiac chondroblastic osteosarcoma with margins free of tumor.
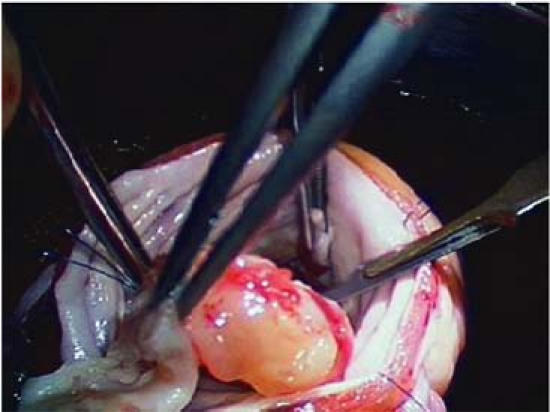
Fig. 2 The anterior leaflet of the mitral valve is held aside to expose the tumor.
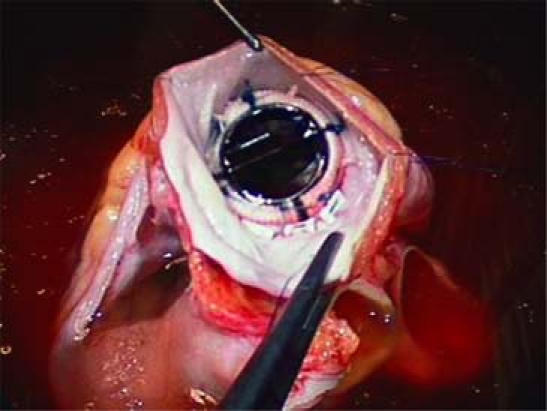
Fig. 3 The mitral valve is replaced with a 25-mm mechanical valve.
Follow-up contact in October 2006 revealed that the patient was doing well. Results of a recent computed tomographic scan showed no disease.
Discussion
Primary cardiac sarcomas are rare; they are found in 0.001% to 0.03% of autopsies.3 Chemotherapy and radiotherapy have been used to treat these tumors, but surgical resection provides better symptom relief in cases of intracavitary obstruction. In addition, the use of chemotherapy and radiotherapy does not substantially increase the ability to surgically resect these lesions.4–7 Intracavitary sarcomas often cause anatomic obstruction to blood flow, which results in severe congestive heart failure. Surgery has been used for relief of the symptoms of obstruction, and for attempted complete surgical resection.8 Anatomic constraints due to inadequate visualization, along with incomplete resection of left atrial sarcomas, have often led to loco-regional recurrence.4–9 We therefore introduced complete cardiac explantation, ex vivo tumor resection, and reconstruction with subsequent cardiac autotransplantation in 1998 to manage the technical dificulties of large left atrial primary sarcomas.1 We have now used this treatment for left atrial tumors successfully on 11 occasions, and once, in the current patient, for a left ventricular tumor.10 The current report describes the 1st use of the autotransplantation technique for a left ventricular tumor.
Left ventricular intracavitary tumors can be approached through a transaortic11 or left ventricular incision,11,12 or through the mitral valve.13,14 In the case presented herein, the large size of the tumor prohibited removal by a transaortic route. A left ventricular approach in this patient would have required an incision through normal left ventricular muscle for tumor exposure, possibly impairing left ventricular function. The left ventricular approach is most useful for tumors of the left ventricular free wall, such as ibromas. In our patient, cardiac explantation allowed excellent exposure of the left ventricular cavity through the mitral valve without injuring non-involved left ventricular myocardium. In addition, our technique provided adequate visualization of the tumor and enabled resection with a sufficient oncologic margin. Resection of the large, intracavitary, primary cardiac sarcoma of the left ventricle was greatly facilitated by the use of cardiac explantation, ex vivo resection, and cardiac reconstruction with subsequent cardiac autotransplantation. We believe this to be a useful approach for treatment of these dificult malignant tumors.
Footnotes
Address for reprints: M.J. Reardon, MD, 6560 Fannin St., #1002, Houston, TX 77030. E-mail: mreardon@tmh.tmc.edu
References
- 1.Reardon MJ, DeFelice CA, Sheinbaum R, Baldwin JC. Cardiac autotransplant for surgical treatment of a malignant neoplasm. Ann Thorac Surg 1999;67:1793–5. [DOI] [PubMed]
- 2.Bakaeen FG, Reardon MJ, Coselli JS, Miller CC, Howell JF, Lawrie GM, et al. Surgical outcome in 85 patients with primary cardiac tumors. Am J Surg 2003;186:641–7. [DOI] [PubMed]
- 3.Straus R, Merliss R. Primary tumours of the heart. Arch Pathol 1945;39:74–80.
- 4.Dein JR, Frist WH, Stinson EB, Miller DC, Baldwin JC, Oyer PE, et al. Primary cardiac neoplasms. Early and late results of surgical treatment in 42 patients. J Thorac Cardiovasc Surg 1987;93:502–11. [PubMed]
- 5.Murphy MC, Sweeney MS, Putnam JB Jr, Walker WE, Frazier OH, Ott DA, Cooley DA. Surgical treatment of cardiac tumors: a 25-year experience. Ann Thorac Surg 1990;49: 612–8. [DOI] [PubMed]
- 6.Okita Y, Miki S, Ueda Y, Tahata T, Sakai T, Matsuyama K. Recurrent malignant fibrous histiocytoma of the left atrium with extracardiac extension. Am Heart J 1994;127:1624–8. [DOI] [PubMed]
- 7.Putnam JB Jr, Sweeney MS, Colon R, Lanza LA, Frazier OH, Cooley DA. Primary cardiac sarcomas. Ann Thorac Surg 1991;51:906–10. [DOI] [PubMed]
- 8.Sanoudos G, Reed GE. Primary cardiac sarcoma. J Thorac Cardiovasc Surg 1972;63:482–5. [PubMed]
- 9.Gabelman C, Al-Sadir J, Lamberti J, Fozzard HA, Laufer E, Replogle RL, Myerowitz PD. Surgical treatment of recurrent primary malignant tumor of the left atrium. J Thorac Cardiovasc Surg 1979;77:914–21. [PubMed]
- 10.Reardon MJ, Malaisrie SC, Walkes JC, Vaporciyan AA, Rice DC, Smythe WR, et al. Cardiac autotransplantation for primary cardiac tumors. Ann Thorac Surg 2006;82:645–50. [DOI] [PubMed]
- 11.Cho JM, Danielson GK, Puga FJ, Dearani JA, McGregor CG, Tazelaar HD, Hagler DJ. Surgical resection of ventricular cardiac fibromas: early and late results. Ann Thorac Surg 2003;76:1929–34. [DOI] [PubMed]
- 12.Schoondyke JW, Burress JW, Shabaneh B, Giorgadze TA, Costello PN, Fahrig S, Whitaker J. Papillary fibroelastoma involving the left ventricular wall. Rev Cardiovasc Med 2003;4:184–7. [PubMed]
- 13.Bortolotti U, Mazzucco A, Valfre C, Valente M, Pennelli N, Gallucci V. Right ventricular myxoma: review of the literature and report of two patients. Ann Thorac Surg 1982; 33:277–84. [DOI] [PubMed]
- 14.Yoshikai M, Kamohara K, Fumoto H, Kawasaki H. Left ventricular myxoma originating from the papillary muscle. J Heart Valve Dis 2003;12:177–9. [PubMed]


