The most common aetiology for organic erectile dysfunction (ED) is vasculogenic. Men with hypertension have a 15% probability of developing complete ED (increasing to 20% if they smoke).1 Those with diabetes have a 28% probability of developing complete ED compared with only a 9% chance in non-diabetics. Other studies have demonstrated that men with a history of ischaemic heart disease and/or peripheral vascular disease have incidences of ED ranging from 39–64%.2
Many men with a history of cardiovascular disease (CVD) do not receive help for ED. The fear of resuming sexual activity following a cardiac event may cause the individual to avoid seeking medical advice. Lack of awareness by the medical practitioner in managing ED in cardiovascular patients may also decrease confidence among those trying to seek medical advice.
The Princeton and British consensus panels, comprising cardiologists, urologists, pharmacologists, and psychiatrists, evaluated the scientific evidence on sexual activity and its risk in cardiac patients. They produced specific guidelines for the management of ED in cardiac patients, based on the principle that sexual activity poses a very small but definite risk of a cardiac event.3 In particular, they identify a role for exercise treadmill testing (ETT) in cardiovascular risk assessment for men presenting with ED. We report on the success of the implementation of these guidelines and in particular the usefulness of ETT in the management of ED.
METHODS
Cardiovascular patients complaining of ED were referred to a specialised ED/CVD clinic. The diagnosis of ED was established using the international index of erectile function4 and all men were questioned about previous ED treatment. A cardiologist initially assessed patients and implemented the British consensus guidelines (table 1). Asymptomatic patients without any physical abnormality on examination were considered low risk and had ED management offered immediately.
Table 1.
Management recommendations based on graded cardiovascular risk assessment (reproduced from Jackson et al, Int J Clin Pract 1999;53:445–51, with permission)
| Grading of risk | Cardiovascular status upon presentation | ED management recommendations for the primary care physician |
| Low risk |
|
|
| Intermediate risk |
|
|
| High risk |
|
|
CAD, coronary artery disease; CHF, congestive heart failure; CVA, cerebral vascular accident; echo, echocardiogram; ED, erectile dysfunction; ETT, exercise tolerance test; LVD, left ventricular dysfunction; NYHA, New York Heart Association; SBP, systolic blood pressure.
Patients who had exercise limiting symptoms and/or abnormal findings during physical examination were referred for cardiological investigations such as ETT and/or echocardiography to aid risk stratification. Men undergoing ETT were exercised to a specific end point (fatigue, chest pain, shortness of breath, hyper- or hypotension or ECG changes), to establish their cardiovascular reserve for resuming sexual activity safely. Patients were stratified into low, intermediate or high cardiac risk. Patients performing more than four minutes (4.5–6.0 METs) on the Bruce protocol with a normal blood pressure response and without any symptoms or ECG changes were stratified as low risk. These men were offered ED treatment. Men who had symptoms, ECG changes or abnormal blood pressure responses before reaching four minutes of the ETT were stratified as intermediate/high risk. ED management in these men was deferred until their cardiac condition was further evaluated and stabilised. Patients already awaiting coronary angiography/intervention were automatically considered high cardiac risk and did not undergo ETT.
RESULTS
Data from 115 men were assessed. The average age was 61 years old (range 25–76 years); 97% (n = 112) had ED. Three men had ejaculatory problems but no ED and required urological assessment.
Fifty nine per cent of men (n = 68) had ischaemic heart disease, and an additional 10% (n = 12) had arrhythmias, cardiomyopathy, or valvar heart disease. The remaining 31% (n = 39) had risk factors for CVD, including hypertension, diabetes, hyperlipidaemia, and a history of smoking.
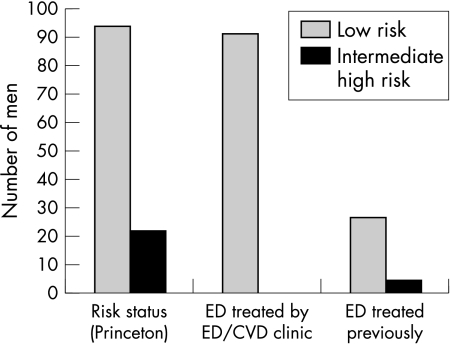
Seventy five per cent of men (85/112) underwent ETT (fig 1); 58% of these men (n = 68) achieved more than four minutes (> 4.5 METS) of the Bruce protocol before reaching an end point. They were low risk and offered ED treatment immediately.
Figure 1.
Erectile dysfunction (ED) treatment according to initial cardiovascular disease (CVD) risk.
Fourteen per cent of men (n = 17) reached an end point before four minutes on the ETT. Three of these men had recent coronary angiography showing minimal disease. They were stratified as low risk and given ED treatment. The remaining 14 men were intermediate/high risk and underwent priority specialised cardiac investigations.
ETT was not performed in 30% of men (n = 27); 19/27 men were asymptomatic with fewer than three risk factors and were stratified as low risk. The remaining eight were already awaiting cardiac interventions and were classified as intermediate/high risk.
Final analysis demonstrated that 81% of the cohort was low risk (n = 93) and 19% was intermediate/high risk (n = 22). Interestingly, almost 25% of the intermediate/high risk men had previously received advice for ED. Only 26/90 low risk men had been previously advised. We successfully treated ED in all 90 without any subsequent cardiac events.
DISCUSSION
During sexual intercourse, the average maximal heart rate is 120–130 beats per minute with a systolic blood pressure increase to 150–180 mm Hg.5 This equates to a minimum of four minutes (4.5 METS) of the Bruce treadmill protocol. Sexual activity can trigger a myocardial infarction but the absolute risk is very low. Low risk patients have a risk for a cardiac event of one chance in a million per hour. This risk is doubled during sexual activity to two chances per million, but only for a two hour period post-intercourse. Patients with coronary artery disease have a 10 fold higher risk but this equates to only 20 chances per million.
ETT identifies cardiac patients with ED who may be at high risk of subsequent cardiac events. Patients unable to achieve four minutes (4.5 METs) on the ETT before reaching an end point may not have the cardiovascular reserve required to resume sexual activity safely. They are high risk and further cardiovascular evaluation and investigation is the priority. The low risk group comprises those who demonstrate the physiological reserve to resume sexual activity. A third group is intermediate risk and these patients must have ED management deferred until further cardiovascular evaluation restratifies them into either a low or high risk group.
The Princeton and British guidelines are extremely valuable for managing ED in cardiac patients. Among our cohort, almost 25% of high risk men previously received ED treatment, while only 23% of low risk men previously received ED treatment. Although the absolute risk of a cardiac event in cardiac patients is small during sexual activity, this risk must be kept to a minimum by exercise testing patients before initiating ED treatment. Without performing this precautionary measure, high risk patients may not be identified and could remain at risk of a potentially fatal cardiac event. Alternatively, failure to perform an exercise test to demonstrate a low cardiac risk status can lead to unnecessary evasion of ED treatment.
Abbreviations
CVD, cardiovascular disease
ED, erectile dysfunction
ETT, exercise treadmill testing
METS, metabolic equivalents
REFERENCES
- 1.Feldman HA, Goldstein I, Hatzichristou DG, et al. Impotence and its medical and psychosocial correlates: results of the Massachusetts male aging study. J Urol 1994;151:54–61. [DOI] [PubMed] [Google Scholar]
- 2.Bortolotti A, Parazzini F, Colli E, et al. The epidemiology of erectile dysfunction and its risk factors. Int J Androl 1997;20:323–34. [DOI] [PubMed] [Google Scholar]
- 3.DeBusk R, Drory Y, Goldstein I, et al. Management of sexual dysfunction in patients with cardiovascular disease: recommendations of the Princeton consensus panel. Am J Cardiol 2000;86:175–81. [DOI] [PubMed] [Google Scholar]
- 4.Rosen RC, Riley A, Wagner G, et al. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997;49:822–30. [DOI] [PubMed] [Google Scholar]
- 5.Jackson G. Sexual intercourse and stable angina pectoris. Am J Cardiol 2000;86:35F–7F. [DOI] [PubMed] [Google Scholar]