Abstract
Background: A recent study using a Doppler guide wire showed that coronary flow velocity measurements immediately after coronary reperfusion were useful in predicting recovery of regional left ventricular function. The value of coronary flow velocity analyses during follow up after reperfusion has not been established in the clinical setting.
Objective: To evaluate coronary flow velocity measurements in predicting recovery of regional left ventricular function during short term follow up after acute anterior myocardial infarction, using transthoracic Doppler echocardiography (TTDE).
Methods: 30 consecutive patients with anterior acute myocardial infarction were studied. They all underwent successful coronary angioplasty for lesions in the left anterior descending coronary artery (LAD). Using TTDE, coronary flow velocity in the LAD was recorded on days 1 and 3, and at one and two weeks after reperfusion. Regional wall motion was analysed by the wall motion score index (WMSI), calculated as an average of segmental scores in the LAD territory before reperfusion and one month after the infarction.
Results: Deceleration time of diastolic flow velocity (DDT) in patients with viable myocardium (WMSI in LAD territory at one month, < 2.0) was significantly longer after recanalisation than in patients without viable myocardium (WMSI in LAD territory at one month, > 2.0): 657 (226) v 271 (117) ms on day 1, p < 0.001; 732 (219) v 373 (217) ms on day 3, p < 0.01; and 903 (107) v 577 (300) ms at one week, p < 0.01. However, the difference at two weeks (991 (75) v 795 (281) ms) was not significant. For the prediction of viable myocardium, DDT > 600 ms had a sensitivity of 78% and a specificity of 92% on day 1, and a sensitivity of 78% and a specificity of 84% on day 3. At one and two weeks, DDT > 600 ms was sensitive (100% and 100%, respectively) but less specific (46% and 26%, respectively) for predicting viable myocardium.
Conclusions: Non-invasive assessment of coronary flow velocity using TTDE within three days of successful coronary angioplasty in patients with anterior acute myocardial infarction is useful in predicting recovery of regional left ventricular function.
Keywords: echocardiography, myocardial blood flow, coronary artery disease
Coronary reperfusion treatment is widely undertaken to restore blood flow to the ischaemic myocardium after acute myocardial infarction, because of its known beneficial effects on the patency of the infarct related artery.1–3 However, it has been reported that the patency of this vessel as assessed by coronary angiography does not always signal successful myocardial salvage.4–6 Although cross sectional echocardiography provides non-invasive assessment of cardiac wall motion, it is difficult to differentiate viable myocardium from irreversibly injured myocardium until the wall motion improves during follow up.5
Analysis of coronary flow velocity using a Doppler guide wire has been used to evaluate myocardial viability.7,8 We recently showed that a rapid deceleration time of diastolic coronary flow velocity immediately after coronary reperfusion reflects a greater degree of microvascular damage in the risk area.8 However, coronary flow velocity analysis by Doppler guide wire is invasive and available only in catheterisation laboratories. Furthermore, previous studies have shown that serial changes to the coronary circulation may occur after coronary reperfusion.9,10 Thus the value of coronary flow velocity analysis during follow up after reperfusion has not been established in the clinical setting.
Recently, we reported that coronary flow velocity in the left anterior descending coronary artery (LAD) can be assessed non-invasively using transthoracic Doppler echocardiography (TTDE) under the guidance of colour flow mapping with a high frequency transducer.11–13 This non-invasive technique may enable us to assess coronary flow velocity serially in the LAD during the follow up period after successful coronary angioplasty in patients with anterior acute myocardial infarction. Our aim in this study was to evaluate the use of coronary flow velocity analysis by TTDE during short term follow up to predict recovery of regional left ventricular function after myocardial infarction.
METHODS
Study patients
The study population consisted of 30 consecutive patients (20 men, 10 women; mean (SD) age, 62 (8) years) with anterior acute myocardial infarction who were successfully recanalised with primary coronary angioplasty within 12 hours of the onset of symptoms. The inclusion criteria were as follows:
first anterior acute myocardial infarction
successful recanalisation with coronary angioplasty (defined as residual diameter stenosis < 50%) within 12 hours after the onset of symptoms
informed consent from the patient to carry out coronary angioplasty.
The diagnosis of acute myocardial infarction was based on the following: more than 30 minutes of continuous chest pain; ST elevation of more than 2.0 mm in two or more contiguous ECG leads; a greater than threefold increase over normal value in serum creatine kinase; and TIMI (thrombolysis in myocardial infarction) flow grade 0, 1, or 2 at initial coronary angiography. Exclusion criteria were previous myocardial infarction and a cardiac event during follow up.
All the participants gave informed consent to the protocol approved by the committee for the protection of human subjects in research at Kobe General Hospital.
Wall motion analysis by TTDE
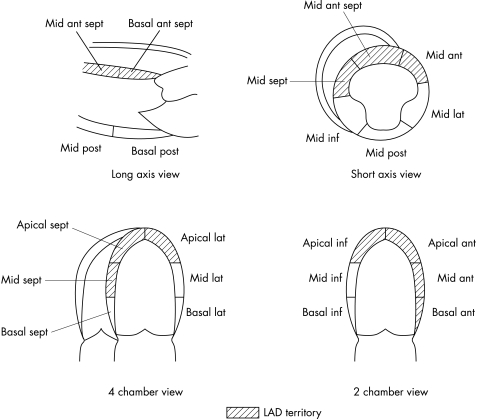
Regional wall motion was examined by TTDE before and one month after the coronary angioplasty. The left ventricular wall was divided into 16 segments and the regional wall motion of each segment was examined and scored according to a modification of the recommendations of the American Society of Echocardiography,14 in which 1 is normal, 1.5 is mild hypokinesis, 2 is hypokinesis, 2.5 is severe hypokinesis, 3 is akinesis, and 4 is dyskinesis.15 Nine of the 16 segments were determined to be LAD territory, and the wall motion score index (WMSI) in the LAD territory was calculated as an average of the wall motion score in these nine segments (fig 1).16 We estimated change in WMSI as that between before reperfusion and one month after reperfusion.
Figure 1.
Diagram of left anterior descending coronary artery (LAD) territory. Ant, anterior; Inf, inferior; Lat, lateral; Post, posterior; Sept, septal.
Serial coronary flow velocity measurements by TTDE
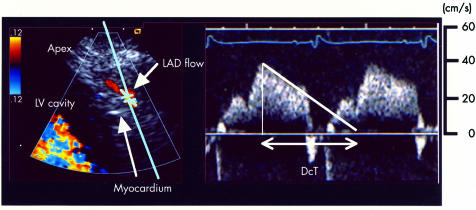
Coronary flow velocity measurement by TTDE was done on days 1 and 3, and at one and two weeks after reperfusion, with a Toshiba SSA-380A ultrasound system (frequency 5.0 or 7.5 MHz), an Acuson Sequoia ultrasound system (frequency 5.0 MHz), or a GE Logic 500 ultrasound system (frequency 3.5–8.0 MHz). In colour flow mapping, the velocity range was set at ±8.1 to ±24.0 cm/s in the Toshiba system, ±8.9 to ±24.0 cm/s in the Acuson system, and ±8.7 to ±20.0 cm/s in the GE system for the purpose of visualising the coronary flow signal. To obtain coronary flow velocity in the mid to distal LAD, the acoustic window was around the mid-clavicular line in the fourth or fifth intercostal spaces in the left lateral decubitus position. First, the left ventricle was imaged in the long axis cross section and the ultrasound beam was inclined laterally. Then mid to distal LAD flow was sought under the guidance of colour flow mapping.10–12 We set the sample volume (2.0 mm wide) in the LAD flow signal. Doppler spectral tracings of coronary flow velocity were recorded on ½12 inch super-VHS videotape (fig 2). Angle correction was undertaken in each Doppler measurement (mean (SD) incident angle, 39 (6)°).
Figure 2.
Coronary flow imaging in the distal left anterior descending coronary artery (LAD) (left) and spectral Doppler flow recording (right) obtained by placing a sample volume in the LAD. LV, left ventricle.
Analysis of coronary flow velocity
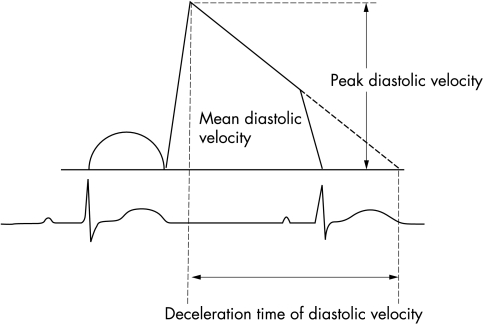
The coronary flow velocity spectrum recorded on super-VHS videotape was digitised by off-line computed planimetry. The digitised coronary flow velocity spectrum provided mean diastolic velocity (MDV), peak diastolic velocity (PDV), and deceleration time of diastolic flow velocity (DDT) (fig 3). An average of the measurements in three cardiac cycles was obtained.
Figure 3.
Measurements of variables of coronary flow velocity recording.
Coronary angiography
All patients received an intravenous bolus injection of 4000 U heparin before angiography, and 0.5 mg/kg/min glyceryl trinitrate was given continuously intravenously soon after establishing the diagnosis. Intracoronary isosorbide dinitrate (2 mg) was given before coronary angiography. Diagnostic coronary angiography was done by the femoral approach using the Judkins technique. After an additional intravenous or intra-arterial bolus injection of 6000 U of heparin, percutaneous transluminal coronary angioplasty, including rescue stenting, was undertaken. Stents were deployed by high pressure implantation techniques. An angiographic criterion of < 50% residual stenosis was used to determine the end point of the angioplasty procedures. Serum creatine kinase was measured serially every three hours after recanalisation until the peak value was obtained. Patients received conventional drug treatment according to individual need, which was determined by the attending physician. The stented patients received anticoagulation with a ticlopidine and aspirin regimen (ticlopidine 100 mg twice a day and aspirin 81 mg twice a day).
Angiographic analysis
Quantitative analysis of per cent diameter stenosis was done using auto-edge detection with a validated technique (CMS; Medical Imaging Systems)17 from a cineangiogram taken before and after coronary intervention. Contrast flow through the infarct related coronary artery was graded by the standard TIMI flow scale of 0 to 3 from the final coronary angiogram.18 Collateral flow was graded according to the Rentrop classification of 0 to 3 from the initial coronary angiogram.19
Statistical analysis
Parametric data are expressed as mean (SD). The difference between wall motion score index in the anterior wall before recanalisation and at one month after recanalisation was evaluated by paired Student’s t test. Comparisons between the two groups for continuous variables were made with an unpaired Student’s t test. The χ2 test was used to compare categorical variables. Analysis of variance and post-hoc t test with Bonferoni corrections was used to analyse repeated measures of coronary flow velocity index. Spearman’s correlation was applied to estimate the relation between variables obtained from coronary flow velocity and WMSI measurements at one month after recanalisation. A probability value of p < 0.05 was considered significant.
Interobserver and intraobserver variabilities were assessed for the measurements of MDV, PDV, and DDT in 15 recordings in seven randomly selected patients. Interobserver variability was calculated as the standard deviation of the differences between the measurements of the two independent observers who were unaware of the other patient data, and expressed as a percentage of the average value. Intraobserver variability was calculated as the standard deviation of the differences between the first and second determinations (a three week interval) for a single observer, and expressed as a percentage of the average value. Interobserver and intraobserver variabilities for the measurements of MDV were 4.8% and 3.9%, respectively; for measurement of PDV they were 5.2% and 4.1%, respectively; and for measurement of DDT they were 5.1% and 4.3%, respectively.
RESULTS
Using TTDE, adequate spectral Doppler recordings of coronary flow in the LAD for coronary flow velocity analysis were obtained during follow up after reperfusion in 22 of the 30 patients (73%). These 22 patients formed the final study group.
Clinical characteristics, clinical, and angiographic results
These data are shown in table 1. Of the 22 patients, 11 had a history of hypertension, 10 had diabetes mellitus, nine had a cholesterol concentration of more than 5.79 mmol/l, and 13 were smokers. Mean (SD) time from the onset of symptoms to coronary perfusion was 374 (171) minutes. The peak creatine kinase level was 4454 (3385) IU/l. Twenty patients developed Q wave infarction, while the other two had non-Q wave infarction. There was no clinical, ECG, or enzymatic evidence of reinfarction in any patient during one month of follow up. In-hospital drug treatment was as follows: nitrates (17), angiotensin converting enzyme inhibitors (18), β adrenergic blocking agents (17), and calcium antagonists (3).
Table 1.
Comparisons between groups
| Variable | Viable myocardium | Non-viable myocardium | p Value |
| n | 9 | 13 | |
| Age (years) | 64 (8) | 62 (10) | 0.65 |
| Male (%) | 5 (56%) | 5 (38%) | 0.43 |
| Onset to recanalisation time (min) | 337 (177) | 353 (135) | 0.84 |
| Proximal LAD occlusion | 5 (56%) | 8 (62%) | 0.78 |
| Per cent diameter stenosis after coronary angioplasty | 27 (12) | 25 (9) | 0.78 |
| TIMI grade 3 flow | 7 (78%) | 10 (77%) | 0.96 |
| Peak creatine kinase (IU/l) | 1939 (1173) | 6526 (3240) | 0.0014 |
| Wall motion score index on admission | 3.2 (0.5) | 3.2 (0.4) | 0.76 |
| Wall motion score index at one month | 1.6 (0.3) | 3.0 (0.6) | 0.0001 |
| Collateral flow on coronary angiogram (Rentrop grade ⩽1) (%) | 3 (33%) | 3 (23%) | 0.60 |
Values are mean (SD) or n (%).
LAD, left anterior descending coronary artery; TIMI, thrombolysis in myocardial infarction trial flow grade.
Coronary angioplasty was successful in all the patients. The culprit lesion was the proximal LAD in 13 and the mid LAD in nine. Fifteen patients had single vessel disease, five had double vessel disease, and one had triple vessel disease. No patient showed good collateral flow (Rentrop grade 3), three had fair collateral flow (Rentrop grade 2), three had poor collateral (Rentrop grade 1), and the remaining 16 had no collateral flow (Rentrop grade 0) on the initial coronary angiogram. Coronary stenting was done in 11 patients. Per cent diameter stenosis after coronary angioplasty was 25 (10)%. Five patients showed TIMI grade 2 reflow, and the remaining 17 patients showed TIMI grade 3 reflow.
Baseline and follow up echocardiography
Wall motion index in the LAD territory decreased significantly from baseline to follow up (from 3.2 (0.4) to 2.4 (0.9), p < 0.001), and the change in WMSI was 0.8 (0.8). We defined viable myocardium as a WMSI at one month of < 2.00 according to a previous report on low dose dobutamine echocardiography.16 We divided the study patients into two groups, one with viable myocardium and one with non-viable myocardium. Table 1 shows a comparison between these two groups. Except for peak creatine kinase, there were no significant differences in baseline characteristics, residual stenosis, WMSI before recanalisation, existence of collateral flow on the initial angiogram, or existence of TIMI grade 3 flow after recanalisation.
Relation between coronary flow velocity pattern and late results
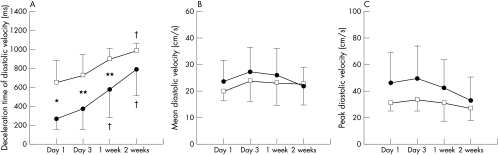
Figure 4 shows coronary flow velocity data during the follow up period in each group. DDT was significantly longer on day 1 in the group with viable myocardium than in the group with non-viable myocardium, at 657 (226) v 271 (117) ms, p < 0.001 (fig 4, panel A). There were significant differences in DDT on day 3 and at one week between the groups with viable and non-viable myocardium (732 (219) v 373 (217) ms, p < 0.01; and 903 (107) v 577 (300) ms, p < 0.01, respectively) (fig 4A). At two weeks, however, the difference in DDT between the two groups was no longer significant (991 (75) v 795 (281) ms) (fig 4, panel A). There were no differences in MDV and PDV values during follow up between the two groups, although there was a trend for PDV to be higher on day 1 in the non-viable group than in the viable group (fig 4, panels B and C). In addition, there were no significant differences in DDT, ADV, and MPV during follow up period between the patients with TIMI grade 2 reflow (n = 5) and TIMI grade 3 reflow (n = 17).
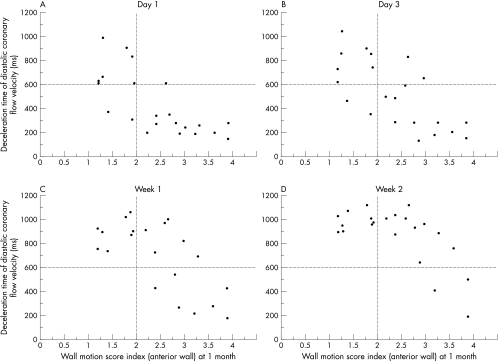
Figure 4.
Time course of deceleration time of diastolic flow velocity (A), mean diastolic velocity (B), and peak diastolic velocity (C) in the viable myocardium group (square symbols) and the non-viable myocardium group (round symbols). *p < 0.001 between groups; **p < 0.01 between groups; †p < 0.01 v day 1 and day 3.
DDT values on days 1 and 3 showed a good correlation with WMSI in the LAD territory at one month after recanalisation (r = −0.79 and −0.71, respectively) (fig 5, panels A and B). Weaker correlations between DDT and WMSI at one month were shown at one week and two weeks of follow up (r = −0.63 and −0.55, respectively) (fig 5, panels B and C). In our previous report, we showed that a DDT value of 600 ms immediately after coronary reperfusion was the best cut off value to predict viable myocardium, using receiver operating characteristics (ROC) curves.8 In the present study, a DDT value of > 600 ms had a sensitivity of 78% and a specificity of 92% on day 1, and a sensitivity of 78% and a specificity of 84% on day 3 for predicting viable myocardium. At one and two weeks, DDT values of more than 600 ms were sensitive (100% and 100%, respectively), but less specific (46% and 26%, respectively), for predicting viable myocardium.
Figure 5.
Relation between wall motion score index in the anterior wall and the deceleration time of diastolic flow velocity on day 1 (A), day 3 (B), at one week (C), and at two weeks (D) after acute myocardial infarction.
DISCUSSION
In this study, we analysed coronary flow velocity serially using TTDE within two weeks after successful coronary angioplasty in patients with acute anterior myocardial infarcts. Our results show that DDT within three days of recanalisation is predictive of viable myocardium. To the best of our knowledge, this is the first report to investigate serial changes in coronary flow velocity pattern during follow up within two weeks after reperfusion in patients with acute myocardial infarction, and to show the value of coronary flow velocity analysis early after recanalisation.
A recent study using a Doppler guide wire has shown that analysis of the coronary flow spectrum immediately after successful coronary angioplasty is useful for predicting recovery of regional left ventricular function.8 Rapid DDT immediately after reperfusion may reflect an increase in coronary vascular resistance caused by microvascular obstruction resulting from perivascular oedema or capillary leucocyte plugging after myocardial ischaemia.20–25 The Doppler guide wire method, however, is available only in cardiac catheterisation laboratories immediately after coronary angioplasty. Furthermore, there is evidence that the coronary circulation may show serial changes after coronary reperfusion.9,10 Thus the value of coronary flow velocity analysis during short term follow up after reperfusion has not been established. TTDE is non-invasive, relatively inexpensive, and widely used in the clinical setting, and can be employed for serial studies not only in echocardiographic laboratories but also in the coronary care unit. Recently, we have reported that coronary flow velocity can be measured with a high degree of success by TTDE under the guidance of colour flow mapping, using a high frequency transducer.11–13 We therefore applied this non-invasive technique to the serial assessment of coronary flow velocity in the left anterior descending coronary artery after successful coronary recanalisation in patients with acute anterior myocardial infarction.
In our present study, DDT measured three days of recanalisation predicted regional recovery of left ventricular function as effectively as that measured immediately after coronary recanalisation in the recent study cited above.8 A rapid DDT within three days may reflect a greater degree of microvascular damage in the risk area after acute myocardial infarction. This can be explained by a high ratio of perfused myocardium to functioning coronary microvasculature.
According to experimental studies, vascular resistance is thought to be affected by microvascular damage (microvascular obstruction) caused by perivascular oedema and capillary leucocyte plugging after myocardial ischaemia.20–25 Using magnetic resonance imaging in an experimental study, Rochitte and colleagues have showed that the extent of microvascular obstruction increases over the first 48 hours after acute myocardial infarction.26 Furthermore, using the same technique Wu and colleagues have reported that the peak extent of microvascular obstruction occurs two days after reperfusion.27 In the present clinical study, there was no significant difference in DDT at two weeks after recanalisation between a group with viable myocardium and a group with non-viable myocardium. This clinical result may be explained by postulating that the extent of microvascular obstruction increases progressively within the first two days after reperfusion, after which there is gradual recanalisation of the occluded microvessels, causing a progressive decrease in coronary resistance. This mechanism could result in a prolongation of DDT after two weeks of follow up, even in patients with no viable myocardium.
Study limitations
It was difficult to analyse coronary flow velocity data in eight of the 30 patients (27%) because of difficulty in obtaining adequate spectral Doppler recordings of coronary flow in the LAD for coronary flow velocity analysis. To improve the success rate in obtaining adequate coronary flow velocity recordings by this non-invasive method, a peripheral injection of a lung crossing contrast agent may be helpful.28
We applied the present method only to the LAD in patients with anterior infarcts, and it was not applied to the other coronary vessels in other territories involved in acute myocardial infarction. At present, it has not been established whether coronary flow velocity in the other coronary vessels can be assessed successfully using TTDE. However, the LAD is a major coronary artery as it vascularises a large amount of myocardium. Thus the non-invasive diagnosis of myocardial viability in the area supplied by this major vessel should be of value in the follow up of any group of patients with acute myocardial infarction.
Third, we did not assess systolic velocity, although the recent report using a Doppler guide wire showed that a low average systolic peak velocity immediately after coronary angioplasty reflects myocardial damage.7,8 Using TTDE, however, it was difficult to obtain an adequate Doppler envelope during systole for coronary flow velocity analysis in 11 of the 30 patients (37%) because of the lower flow velocity during systole compared with diastole. This results in difficulty in differentiating the coronary flow velocity signal from an artefact signal using the Doppler technique.
In the present study, we did not evaluate the TIMI frame count and TIMI blush score between the patients with and without myocardial viability, although there was no difference in TIMI grade 3 flow between the two study groups. Further investigations are necessary to determine the beneficial effects of coronary intervention on microvasculature function.
Finally, we judged viable myocardium by the wall motion score index at one month using TTDE, because improvement in wall motion is clinically important. However, more quantitative methods such as single photon emission computed tomography or positron emission tomography may be preferred for a more accurate evaluation of viable myocardium.
Conclusions
Using transthoracic Doppler echocardiography, non-invasive assessment of coronary flow velocity in the left anterior descending coronary artery, within three days of successful coronary angioplasty in patients with anterior acute myocardial infarction, is useful in predicting recovery of regional left ventricular function.
Acknowledgments
We gratefully acknowledge the technical assistance of Toshikazu Yagi, sonographer, and the statistical assistance of Robert Sciacca PhD, statistician.
Abbreviations
DDT, diastolic deceleration time
LAD, left anterior descending coronary artery
MDV, mean diastolic velocity
PDV, peak diastolic velocity
TIMI, thrombolysis in myocardial infarction study flow grade
TTDE, transthoracic Doppler echocardiography
WMSI, wall motion score index
REFERENCES
- 1.Chesebro JH, Knatterud G, Roberts R, et al. Thrombolysis in myocardial infarction (TIMI) trial, phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase: clinical findings through hospital discharge. Circulation 1987;76:142–54. [DOI] [PubMed] [Google Scholar]
- 2.The GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction.N Engl J Med 1993;329:1615–22. [DOI] [PubMed] [Google Scholar]
- 3.Simes RJ, Topol EJ, Holmes DR, et al. Link between the angiographic substudy and mortality outcomes in a large randomized trial of myocardial reperfusion: importance of early and complete infarct artery reperfusion. Circulation 1995;91:1923–8. [DOI] [PubMed] [Google Scholar]
- 4.Ito H, Tomooka T, Sakai N, et al. Lack of myocardial perfusion immediately after successful thrombolysis: a predictor of poor recovery of left ventricular function in anterior myocardial infarction. Circulation 1992;85:1699–705. [DOI] [PubMed] [Google Scholar]
- 5.Ito H, Okamura A, Iwakura K, et al. Myocardial perfusion patterns related to thrombolysis in myocardial infarction perfusion grades after coronary angioplasty in patients with acute anterior wall myocardial infarction. Circulation 1996;93:1993–9. [DOI] [PubMed] [Google Scholar]
- 6.Ito H, Iwakura K Oh H, et al. Temporal changes in myocardial perfusion patterns in patients with reperfused anterior wall myocardial infarction: their relation to myocardial viability. Circulation 1995;91:656–62. [DOI] [PubMed] [Google Scholar]
- 7.Iwakura K, Ito H, Takiuchi S, et al. Alteration in the coronary blood flow velocity pattern in patients with no reflow and reperfused acute myocardial infarction. Circulation 1996;94:1269–75. [DOI] [PubMed] [Google Scholar]
- 8.Kawamoto T, Yoshida K, Akasaka T, et al. Can coronary blood flow velocity pattern after primary percutaneous transluminal coronary angioplasty predict recovery of regional left ventricular function in patients with acute myocardial infarction ? Circulation 1999;100:339–45. [DOI] [PubMed] [Google Scholar]
- 9.Villanueva FS, Glasheen WP, Sklenar J, et al. Characterization of spatial patterns of flow within the reperfused myocardium by myocardial contrast echocardiography: implications in determining extent of myocardial salvage. Circulation 1993;88:2596–606. [DOI] [PubMed] [Google Scholar]
- 10.Ambrosio G, Weisman HF, Mannisi JA, et al. Progressive impairment of regional myocardial perfusion after initial restoration of postischemic blood flow. Circulation 1989;80:1846–61. [DOI] [PubMed] [Google Scholar]
- 11.Hozumi T, Yoshida K, Ogata K, et al. Noninvasive assessment of significant left anterior descending coronary artery stenosis by coronary flow velocity reserve using transthoracic color Doppler echocardiography. Circulation 1998;97:1557–62. [DOI] [PubMed] [Google Scholar]
- 12.Hozumi T, Yoshida K, Akasaka T, et al. Noninvasive assessment of coronary flow velocity and coronary flow velocity reserve in the left anterior descending coronary artery by Doppler echocardiography: comparison with invasive technique. J Am Coll Cardiol 1998;32:1251–9. [DOI] [PubMed] [Google Scholar]
- 13.Hozumi T, Yoshida K, Akasaka T, et al. Value of acceleration flow and the prestenotic to stenotic coronary flow velocity ratio by transthoracic color Doppler echocardiography in noninvasive diagnosis of restenosis after percutaneous transluminal coronary angioplasty. J Am Coll Cardiol 2000;35:164–8. [DOI] [PubMed] [Google Scholar]
- 14.Shiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two–dimensional echocardiography: American Society of Echocardiography Committee on Standards, subcommittee on quantitation of two-dimensional echocardiography.J Am Soc Echocardiogr 1989;2:358–67. [DOI] [PubMed] [Google Scholar]
- 15.Lee HH, Davia RV, Ludbrook PA, et al. Dependency of contractile reserve on myocardial blood flow: implications for the assessment of myocardial viability with dobutamine stress echocardiography. Circulation 1997; 96:2884–91. [DOI] [PubMed] [Google Scholar]
- 16.Smart SC, Sawada S, Ryan T, et al. Low-dose dobutamine echocardiography detects reversible dysfunction after thrombolytic therapy of acute myocardial infarction. Circulation 1993;88:405–15. [DOI] [PubMed] [Google Scholar]
- 17.Hausleiter J, Notle CWT, Jost S, et al. Comparison of different quantitative coronary analysis systems: ARTREK, CAAS, and CMS. Cathet Cardiovasc Diagn 1993;88:405–15. [DOI] [PubMed] [Google Scholar]
- 18.TIMI Study Group. The thrombolysis in myocardial infarction (TIMI) trial: phase I findings. N Engl J Med 1985;312:932–6. [DOI] [PubMed] [Google Scholar]
- 19.Rentrop KP, Cohen M, Blanke H, et al. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol 1985;5:587–92. [DOI] [PubMed] [Google Scholar]
- 20.Willerson JT, Watson JT, Hutton I, et al. Reduced myocardial reflow and increased coronary vascular resistance following prolonged myocardial ischemia in the dog. Circ Res 1975;36:771–81. [DOI] [PubMed] [Google Scholar]
- 21.Tranum-Jensen J, Janse MJ, Fiolet WT, et al. Tissue osmolality, cell swelling, and reperfusion in acute regional myocardial ischemia in the isolated porcine heart. Circ Res 1981;49:364–81. [DOI] [PubMed] [Google Scholar]
- 22.Powers ER, Dibona DR, Powell J. Myocardial cell volume and coronary resistance during diminished coronary reperfusion. Am J Physiol 1984;247:467–77. [DOI] [PubMed] [Google Scholar]
- 23.Engler RL, Schmid-Schonbein GW, Pavelec RS. Leukocyte capillary plugging in myocardial ischemia and reperfusion in the dog. Am J Pathol 1983;111:98–111. [PMC free article] [PubMed] [Google Scholar]
- 24.Engler RL, Dahlgren MD, Morris DD, et al. Role of leukocytes in response to acute myocardial ischemia and reflow in dogs. Am J Pathol 1986;251:H314–23. [DOI] [PubMed] [Google Scholar]
- 25.Sheridan FM, Cole PG, Ramage D. Leukocyte adhesion to the coronary microvasculature during ischemia and reperfusion in an in vivo canine model. Circulation 1996;93:1784–7. [DOI] [PubMed] [Google Scholar]
- 26.Rochitte CE, Lima JAC, Bluemke DA, et al. Magnitude and time course of microvascular obstruction and tissue injury after acute myocardial infarction. Circulation 1998;98:1006–14. [DOI] [PubMed] [Google Scholar]
- 27.Wu KC, Kim R, Bluemke DA, et al. Quantitation and time course of microvascular obstruction by contrast-enhanced echocardiography and magnetic resonance imaging following acute myocardial infarction and reperfusion. J Am Coll Cardiol 1998;32:1756–64. [DOI] [PubMed] [Google Scholar]
- 28.Caiati C, Montaldo C, Zedda N, et al. New noninvasive method for coronary flow reserve assessment: contrast-enhanced transthoracic second harmonic echo Doppler. Circulation 1999;99:771–8. [DOI] [PubMed] [Google Scholar]