Swimming and scuba diving can induce pulmonary oedema in people with apparently normal hearts.1–3 Affected individuals are predisposed to developing hypertension1 and one patient, described in our original report, later had high altitude pulmonary oedema (unpublished observation). Subsequently, nine more patients (four with hypertension) have suffered pulmonary oedema induced by scuba diving and swimming. Three of these individuals also had episodes of pulmonary oedema induced by other triggers (emotional stress, sexual intercourse, and exertion in extremely cold conditions). In addition, three non-divers have had pulmonary oedema precipitated by triggers such as emotional stress (two patients) or sexual intercourse. In all six individuals there was no identified cardiac abnormality; two patients were known to have pre-existing hypertension, two were discovered to have hypertension at presentation, and two were normotensive.
CASE 1
One of the patients, a man aged 61 years, had his first episode of pulmonary oedema, with dyspnoea and haemoptysis, precipitated by an argument. He had bilateral pulmonary crepitations and his blood pressure was 170/100 mm Hg. He recovered after receiving an intravenous diuretic. During the next four years he had three more episodes of pulmonary oedema confirmed on chest x rays, which were induced by swimming on one occasion and by arguments on two further occasions. On the fourth occasion the pulmonary oedema was so severe that he required mechanical ventilation. Cardiac enzymes and ECGs were normal on each occasion. An echocardiogram, left heart catheterisation, and coronary angiograms were normal; nephrograms were also normal. A 24 hour ambulatory ECG was normal. Urine and plasma catecholamine concentrations between episodes were normal. He was treated with an angiotensin converting enzyme (ACE) inhibitor, nifedipine, nitrates, and frusemide (furosemide).
CASE 2
A woman aged 41 years had a single episode of pulmonary oedema with dyspnoea and expectoration of bloodstained froth when scuba diving. A chest x ray showed pulmonary oedema. ECGs showed transient T wave inversion in leads I and V6. Cardiac enzymes were normal. She recovered after an intravenous diuretic. She had three similar episodes of pulmonary oedema precipitated by sexual intercourse. An echocardiogram, left and right heart catheterisation, and coronary angiograms were normal. Her blood pressure was consistently normal. Vasodilator treatment was recommended.
CASE 3
An exceptionally fit man had two episodes of radiologically confirmed pulmonary oedema with dyspnoea, expectoration of bloodstained froth, and bilateral pulmonary crepitations. The first occurred when he was 35 years old following strenuous exercise while scuba diving in water at a temperature of 2°C during a research experiment. His ECG was monitored during the experiment and there was no arrhythmia. A second episode occurred two years later while cross-country skiing carrying an 85 lb backpack in the Arctic (air temperature was −13 °C). Blood pressure was consistently normal. ECGs and echocardiograms were normal. Cardiac catheterisation was not performed. A treadmill exercise test was stopped after six stages (18 minutes) of the Bruce protocol without symptoms or changes on the ECG.
CASE 4
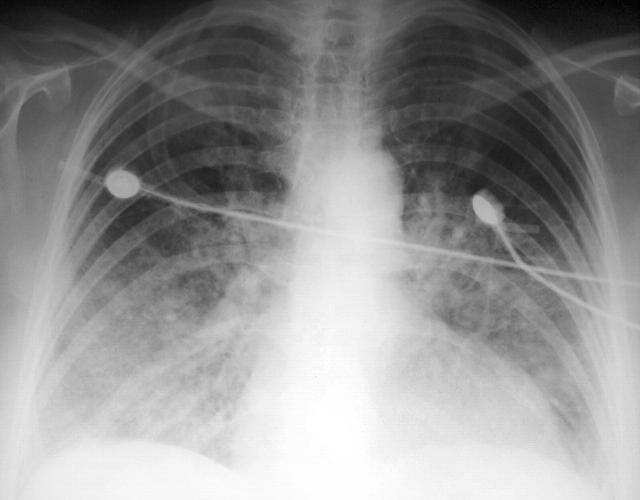
A woman aged 65 years had two episodes of pulmonary oedema in four months; each episode was precipitated by emotional stress whilst driving, once when her car had broken down in a dangerous situation and once when she was verbally abused by another motorist. A chest x ray (fig 1) and arterial hypoxaemia (pO2 7.6 kPa on air) confirmed pulmonary oedema. Her initial ECG showed left bundle branch block. Shortly afterwards there was normal conduction with T wave inversion in V1–V6, I and aVl. The next day the repolarisation abnormality was normal. She had no chest pain and cardiac enzymes did not suggest myocardial infarction. She had previously been hypertensive during pregnancies when aged 26 and 30 years. She was prescribed atenolol for sustained hypertension when aged 57 years. Left heart catheterisation, coronary angiograms, and nephrograms were all normal. An echocardiogram showed mild left ventricular hypertrophy consistent with hypertension. A 24 hour ambulatory ECG was normal. Urinary excretion of catecholamines was normal. She was treated with an ACE inhibitor and nifedipine.
Figure 1.
Chest x ray of case 4.
CASE 5
A woman aged 59 years had a single episode of pulmonary oedema confirmed by chest x ray. An argument with a work manager precipitated dyspnoea with tight chest discomfort. An ECG showed transient T wave inversion in V2-V6, I, II, aVl and aVf. Cardiac enzymes were normal, left heart catheterisation and coronary angiograms were normal, nephrograms were normal, and urinary excretion of catecholamines was normal. Sustained hypertension was confirmed at subsequent follow up. She was treated with an ACE inhibitor and a long acting nitrate.
CASE 6
A man aged 58 years, who had longstanding hypertension, had four episodes of pulmonary oedema precipitated by sexual intercourse. An echocardiogram showed that the left ventricle was mildly dilated but there was no other abnormality. Right and left heart catheterisation also showed that the left ventricle was mildly dilated but contraction was good (ejection fraction 51%). Coronary arteries and left ventricular biopsies were normal. Renal arteriograms were normal. During an exercise test he did nine minutes of the Bruce protocol without pain or ECG abnormality, but his blood pressure rose from 140/80 mm Hg to 270/90 mm Hg. Plasma catecholamines concentrations and an m-iodobenzylguanidine scan were normal. On treatment with an ACE inhibitor, nifedipine, bendrofluazide, and atenolol he was well for three years. After another cardiologist stopped his ACE inhibitor, he had another episode of pulmonary oedema during sexual intercourse.
DISCUSSION
There are a small number of case reports that complement my observations and suggest that pulmonary oedema may be precipitated in some individuals without evidence of heart disease if there is an appropriate trigger such as idiosyncratic emotional stress, sexual intercourse or exercise. Pulmonary oedema has been reported in two athletes during a 90 km race4; cardiac investigations including echocardiography and coronary angiography showed no abnormality. There is a report of haemoptysis during sexual intercourse in a patient with mild mitral regurgitation.5 Another study reports that the emotional stress associated with bereavement mimicked acute myocardial infarction and produced pulmonary oedema in two women with normal coronary arteries.6 In this report both affected women had chest pain; however, only one of my patients experienced chest pain (case 5).
These observations suggest that some individuals who appear to have normal hearts may develop pulmonary oedema during emotional stress, extreme exertion, or sexual intercourse. These individuals appear to be susceptible to pulmonary oedema when swimming or scuba diving and appear predisposed to hypertension. The cause of the episodes of pulmonary oedema is uncertain but left ventricular diastolic dysfunction may contribute. Coronary artery spasm may be involved in the aetiology of the patients who experienced chest pain; however, it seems most probable that in these patients episodes of acute left ventricular failure were precipitated by acute hypertension as a result of neurohumoral stimulation. Flash pulmonary oedema can be produced in individuals with a normal heart if there is massive release of catecholamines from a phaeochromocytoma and also in some individuals with renal artery stenosis. There is no evidence that these patients had either of these pathologies, but a similar neurohumoral mechanism may be involved.
Acknowledgments
I am grateful to colleagues who referred these patients to me for an opinion.
REFERENCES
- 1.Wilmshurst PT, Nuri M, Crowther A, et al. Cold-induced pulmonary oedema in scuba divers and swimmers and subsequent development of hypertension. Lancet 1989;i:62–5. [DOI] [PubMed] [Google Scholar]
- 2.Pons M , Blickenstorfer D, Oechslin E, et al. Pulmonary oedema in healthy persons during scuba-diving and swimming. Eur Respir J 1995;8:762–7. [PubMed] [Google Scholar]
- 3.Weiler-Ravell D , Shupak A, Goldenberg I, et al. Pulmonary oedema and haemoptysis induced by strenuous swimming. BMJ 1995;311:361–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McKechnie JK, Leary WP, Noakes TD, et al. Acute pulmonary oedema in two athletes during a 90-km running race. S Afr Med J 1979;56:261–5. [PubMed] [Google Scholar]
- 5.Maxwell D , Rees PJ. Exertion-induced haemoptysis. Lancet 1993;341:375. [DOI] [PubMed] [Google Scholar]
- 6.Pavin D , Le Breton H, Daubert C. Human stress cardiomyopathy mimicking acute myocardial syndrome. Heart 1997;78:509–11. [DOI] [PMC free article] [PubMed] [Google Scholar]