Abstract
Objective: To evaluate the clinical impact of fetal echocardiography before 16 weeks’ gestation on the management of pregnancies with fetuses at risk of congenital heart disease.
Design and setting: Observational study in a fetal medicine unit.
Participants and methods: 222 consecutive women with high risk pregnancies (230 fetuses) underwent transabdominal fetal echocardiography at a median gestation of 14+1 weeks. For 10%, transvaginal scans were also performed. Criteria for normal scans were normal sequential segmental analysis, symmetrical four chamber view, normal semilunar valves, arterial outflow tracts, and ductal and aortic arches. Early scans were compared with mid-second trimester fetal echocardiography. Postmortem and postnatal data were added. Adverse pregnancy outcomes were diagnosis of a major cardiac or extracardiac abnormality, chromosomal defects, intrauterine death, or termination of pregnancy.
Results: There were 21 abnormal cardiac scans (9%): 14 major structural defects (eight isolated, six with chromosomal or extracardiac abnormalities) in pregnancies resulting in three live births, one intrauterine death, and 10 terminated pregnancies. Seven scans showed asymmetry between right and left sided structures (two isolated, five with chromosomal or extracardiac abnormalities); six of the seven pregnancies were terminated. The scans were normal in 199 cases (87%). Cardiac follow up of 184 of 199 babies (93%) confirmed situs and connections. One case each of pulmonary stenosis and ventricular septal defect requiring postnatal intervention were diagnosed at later scans. In 28 of 199 (14%) babies there was a non-cardiac adverse outcome. First examination was not diagnostic for 10 (4%).
Conclusion: Early fetal echocardiography in high risk pregnancies was diagnostic in 96%. Abnormal cardiac scans (isolated in 48%, major structrual defects in 67%) led to termination of pregnancy in 76%. Most cardiac scans were normal, allowing family reassurance. The high number of adverse outcomes with normal cardiac anatomy stresses the need for a multidisciplinary approach to early fetal echocardiography.
Keywords: echocardiography, heart defects, congenital heart disease, diagnosis, pregnancy
Since our report1 that fetal cardiac anomalies can be identified by transabdominal echocardiography towards the end of the first trimester, this technique has been applied in other centres where fetal nuchal translucency (NT) is routinely measured.2 This echo-free space at the back of the neck is measured at 11–14 weeks’ gestation. An increased thickness (typically > 4 mm) is strongly associated with abnormal chromosomes, with or without congenital heart disease (CHD).3,4 In a recent study by Huggon and colleagues2 cardiac anomalies were confidently identified in 60 of 478 fetuses and suspected in a further 20. Of all their fetuses scanned, 84% had an increased NT thickness or an abnormal ductus venosus Doppler signal and 39.5% had abnormal chromosomes (72.9% of those with cardiac abnormalities). We assessed the impact of early fetal echocardiography on the management of high risk pregnancies, among which the majority of fetuses had normal chromosomes.
METHODS
Study population
The population studied consisted of all consecutive patients who underwent detailed fetal echocardiography at a gestational age ⩽ 16+0 weeks within our Fetal Medicine Unit by a single experienced operator. Between January 1997 and August 2002, 230 fetuses (222 pregnancies) were studied. The indications for fetal echocardiography were a recognised increased risk of CHD as part of the clinical management of high risk pregnancies (increased NT: 102, family history: 95, abnormal findings during early scan: 6, other indications: 27). Verbal informed consent was obtained in all cases before the ultrasound scan.
Fetal echocardiographic examination
Before each examination the reasons for the cardiac scan were explained and the estimated individual relative risks of CHD were discussed (2% for one and 10% for two affected children, and > 2% for increased NT thickness, variable with the specific NT measurement). All patients were informed about the aims of the study. The need for follow up scans and the limitations of first and early second trimester scans related to fetal size (anteroposterior diameter of the fetal chest at 13 weeks of approximately 2.5 cm) and resolution obtainable by the ultrasound equipment were pointed out. The sequential segmental approach to diagnosis was used in all cases.5 The fetal echocardiogram was targeted to visualise the major cardiac structures and was considered normal if the following were imaged: visceral situs solitus and normal cardiac position; normal and symmetrical four chamber view with two separate atrioventricular valves; normal aortic and pulmonary outflow tracts, including the septoaortic continuity; two great arteries of similar size in a spiral spatial relation (that is, normal crossover with the anterior left sided pulmonary artery crossing from left to right in front of the posterior ascending aorta); and evidence of the ductal and aortic arches. Visualisation of the trabecular part of the interventricular septum was variable. Image optimisation was obtained with the use of colour and power Doppler. Colour flow mapping was routinely used to assess intracardiac and great artery blood flow velocities. Pulsed wave Doppler was not routinely used. All studies were carried out transabdominally. Transvaginal scans were offered if an abnormality was detected or if the information obtained by the transabdominal route was not diagnostic. In addition, all fetuses were assessed by a team specialised in fetal medicine to diagnose or exclude major extracardiac malformations and to measure NT thickness, if appropriate. In all cases where a cardiac abnormality was detected, fetal karyotyping was offered if it had not been carried out previously. In the majority of fetuses assessed, because of an increased NT thickness, karyotyping had already been performed before the detailed cardiac scan.
Follow up and counselling
Normal scan group
Follow up appointments were made for fetal echocardiography at 18–22 weeks. This was used as the ideal for the accuracy of the first trimester scan. Additionally, postnatal information from our own or referring hospitals and postmortem data for cases of either termination of pregnancy or intrauterine death were obtained.
Abnormal scan group
When a structural cardiac abnormality was detected, the diagnosis and likely postnatal outcome were discussed with the families. Counselling was an integrated approach between the fetal cardiologist and the specialist in fetal medicine. This was particularly important when criteria for normality of the cardiac scan were not met yet no major structural malformation was detected (for example, asymmetry between right and left sided structures; see Results). Clinical geneticists working within the same department provided additional counselling when necessary, for example, when there was a positive family history or a chromosomal anomaly or syndrome. In all cases of termination of pregnancy or intrauterine death, we stressed the importance of confirmatory postmortem examination and its significance for adequate counselling of subsequent pregnancies. Adverse pregnancy outcomes were diagnosis of a major cardiac or extracardiac malformation, a chromosomal abnormality, intrauterine death, or termination of pregnancy.
Postmortem examination
All specimens were examined with parental consent and in accordance with the guidelines of the Polkinghorne report for the study of fetal tissues.6 The protocol used for fixation and for stepwise microdissection of the heart has been published elsewhere.7 High flow, low pressure perfusion was used to fix the heart in “end diastole”, which was microdissected following the direction of flow. Description of abnormalities followed the sequential segmental approach.
RESULTS
Fetal echocardiography was performed in 230 fetuses at ⩽ 16+0 weeks of gestation. Median gestational age was 14+1 weeks (range 10+1 to 16+0 weeks). In 220 (96%) the scans were diagnostic allowing distinction between 199 normal and 21 abnormal scans. Among the 10 non-diagnostic cases (median gestational age at first examination 11+6 weeks, range 10+1 to 13+6), seven fetuses were shown to be normal on subsequent scans, two pregnancies were terminated (trisomy 18), and one fetus died after laser treatment for twin to twin transfusion syndrome before a repeat scan could be performed (first scan at 10+1 weeks). Transvaginal scans were carried out in 24 cases in addition to the transabdominal route. This combined approach was helpful in three of 10 abnormal cases and in 12 of 14 normal scans.
Normal scans
In 199 cases, criteria for a normal early scan were met and the families were reassured that no major structural cardiac abnormality was detected (fig 1). In 15 the early findings could not be confirmed: five families opted to terminate the pregnancy for non-cardiac fetal abnormalities (four abnormal chromosomes), four fetuses died spontaneously before a second cardiac scan (no postmortem examination), and six were lost to follow up. Of the remaining 184 scans, normal situs and cardiac connections were subsequently confirmed in all. In seven, normality was confirmed at postmortem examination (six terminated pregnancies due to extracardiac and chromosomal abnormalities and one intrauterine death before follow up scan). One fetus, considered to have a normal early scan at 14+6 weeks, had mild valvar pulmonary stenosis on follow up at 21+6 weeks, which progressed throughout gestation and required balloon dilatation in the early neonatal period. Retrospective review of the videotape images suggested mildly abnormal movement of the pulmonary valve leaflets at 14+6 weeks. One fetus was shown to have a large ventricular septal defect (VSD) on follow up. Three other fetuses were found to have a small VSD on the 20–22 week scan. Two VSDs closed spontaneously before delivery and in one case a tiny mid-muscular defect was still present in the neonate. Six liveborn babies had chromosomal defects.
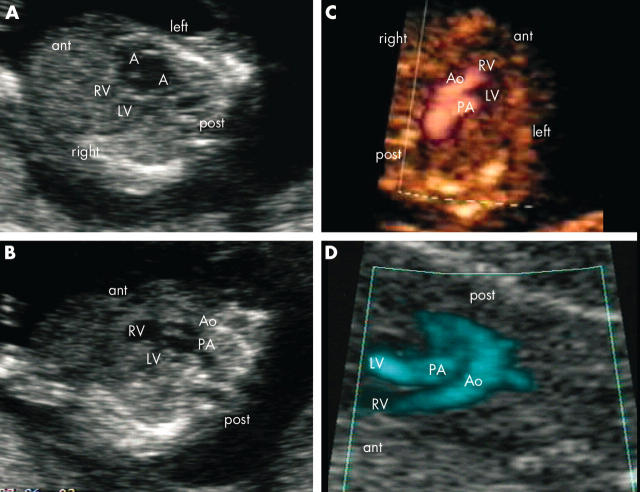
Figure 1.
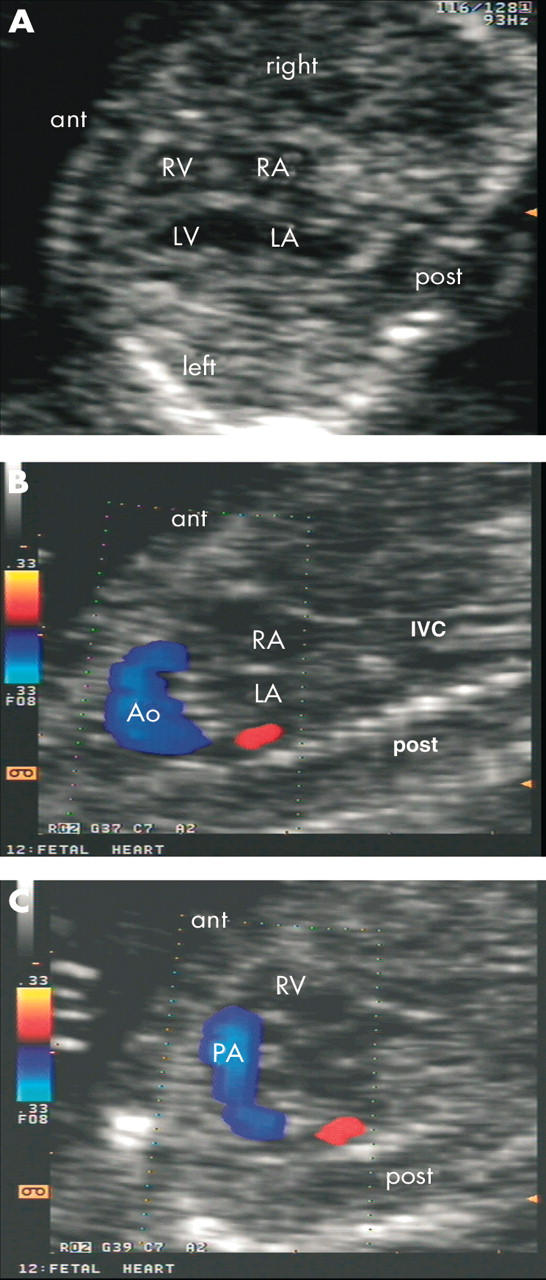
Normal transabdominal fetal echocardiogram from a 13 week fetus. (A) Transverse section of the fetal chest shows a normal four chamber view. Longitudinal sections of the fetus show normal (B) aortic and (C) ductal arches. ant, anterior; Ao, aorta; IVC, inferior vena cava; LA, left atrium; LV, left ventricle; PA, pulmonary artery; post, posterior; RA, right atrium; RV, right ventricle.
Abnormal scans
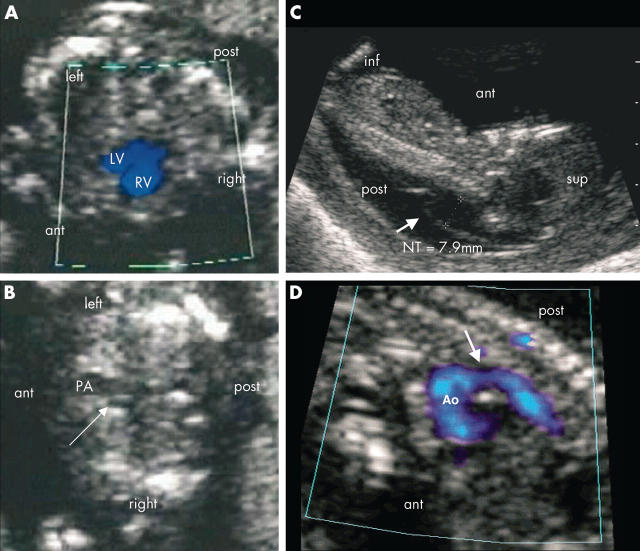
The initial scan was abnormal in 21 cases. Twelve cases showed a major structural malformation of the heart (fig 2). In two with concordant atrioventricular and ventriculoarterial connections, septal defects were suspected (table 1). Scans for the other seven fetuses showed asymmetry between the right and left sided cardiac structures, the left being smaller (table 2).
Figure 2.
(A, B) Transabdominal ultrasound images from a fetus at 12+5 weeks’ gestation with left isomerism. (A) Transverse section of the fetal chest shows a right sided heart and cardiac apex. The four chamber view shows an atrioventricular septal defect, common atrium (A), and common atrioventricular valve. (B) Oblique view shows the parallel arrangement of the great arteries (double outlet right ventricle; anterior, smaller aorta). (C, D) Transabdominal views from a fetus with complete transposition of the great arteries at (C) 13+3 and (D) 14+3 weeks. (C) Upper mediastinal transverse section through the fetal chest shows the abnormal parallel arrangement of the great arteries with an anterior and right sided aorta. (D) Longitudinal section of the fetus shows the aorta and aortic arch connected to the anterior right ventricle and pulmonary artery originating from the posterior left ventricle.
Table 1.
Abnormal cardiac scans showing structural abnormality
| Patient | Indication | GA (weeks+days) | Cardiac findings | Other ultrasound findings | Karyotype | Outcome |
| 1 | Abnormal four chamber scan | 12+1 | Left isomerism, AVSD, two great arteries | Encephalocoele | Normal | TOP at 14+1 weeks, postmortem confirmation; additional interrupted aortic arch |
| 2 | Increased NT, mosaicism for T21 | 14+4 | Possible AVSD (no TV done) | Nil | T21 (mosaicism) | TOP at 14+6 weeks, postmortem AVSD |
| 3 | Increased NT, T21 | 15+5 | AVSD | Nil | T21 | Intrauterine death at 17+6 weeks, no postmortem examination |
| 4 | Increased NT | 12+6 | Hypoplastic left heart syndrome | Hydropic fetus | Normal | TOP at 13 weeks, postmortem confirmation |
| 5 | Bradycardia | 12+5 | Left isomerism, common atrium, AVSD, common valve, DORV (Ao <PA), heart block (rate 60 beats/min) | Nil, normal NT | Normal | TOP at 13+3 weeks, postmortem confirmation; additional severe distal arch hypoplasia |
| 6 | Previous T21, AVSD | 13+2 | Possible VSD (no TV done) | Increased NT, hydropic fetus | T21 | TOP at 13+6 weeks, postmortem perimembranous outlet VSD |
| 7 | Increased NT, T21 | 14+6 | AVSD, pulmonary atresia | Nil | T21 | TOP at 16+4 weeks, no postmortem examination |
| 8 | Increased NT | 13+3 | Complete transposition | Nil | Normal | Live birth, successful neonatal arterial switch procedure |
| 9 | Increased NT | 14+0 | Mitral atresia, VSD, pulmonary atresia | Nil | Normal | TOP at 14+3 weeks, postmortem confirmation |
| 10 | Increased NT, bradycardia | 11+3 | Left isomerism, AVSD, heart block | Nil | Not done | TOP at 12+5 weeks, no postmortem examination |
| 11 | Family history | 14+5 | Small mitral valve, left ventricle, pulmonary atresia | Nil | Not done | TOP at 14 weeks, no postmortem examination |
| 12 | Increased NT | 13+4 | Tricuspid atresia | Nil | Normal | TOP <16 weeks, no postmortem examination |
| 13 | Increased NT, pericardial effusion | 14+4 | Large cardiac diverticulum, pericardial effusion | Hydrops | Normal | Live birth, small RV diverticulum |
| 14 | Increased NT | 15+5 | AVSD | Nil | T21 | Live birth, successful AVSD repair |
Ao, aorta; AVSD, atrioventricular septal defect; DORV, double outlet right ventricle; GA, gestational age; NT, nuchal translucency; PA, pulmonary artery; RV, right ventricular; T21, trisomy 21; TOP, termination of pregnancy; TV, transvaginal scan; VSD, ventricular septal defect.
Table 2.
Abnormal cardiac scans showing asymmetry between right and left sided structures
| Patient | Indication | GA (weeks+days) | Cardiac findings | Other ultrasound findings | Karyotype | Outcome |
| 1 | Increased NT | 13+0 | Asymmetry RV/LV | Increased NT of 7 mm, no other findings | Normal | Planned for serial scans; TOP at 13 weeks, postmortem severely narrowed aortic isthmus (<300 μm). |
| 2. | Family history congenital heart disease (×2) | 13+1 | Asymmetry RV/LV and Ao/PA, right sided heart | Diaphragmatic hernia suspected at 15 weeks; severe diaphragmatic hernia, left heart hypoplasia at 19 weeks | Normal | TOP at 21+3 weeks, postmortem large diaphragmatic hernia with severe lung hypoplasia, hypoplasia of the LV and severely hypoplastic aortic arch |
| 3 | Increased NT, unbalanced translocation | 16+0 | Asymmetry RV/LV | Progressive left ventricular outflow obstruction on subsequent scans | Unbalanced translocation (7/15) | TOP at 23+6 weeks, postmortem severe hypoplasia of LV and aortic arch |
| 4 | Increased NT | 14+1 | Asymmetry RV/LV, right sided heart | Limb abnormality, suspected diaphragmatic hernia | Normal | TOP at 14+2 weeks, no postmortem examination |
| 5 | Increased NT | 13+1 | Small aortic isthmus | Increased NT of 7.9 mm; no other findings | Normal | Planned for serial scans; TOP at 13 weeks, no postmortem examination |
| 6 | Increased NT | 13+3 | Asymmetry RV/LV, distal aortic arch not seen | Cystic hygroma | 45 XO | TOP at 14+0 weeks, postmortem severely narrowed aortic arch and isthmus |
| 7 | Exomphalos | 14+2 | Asymmetry RV/LV and Ao/PA | Exomphalos | Normal | Live birth, successful repair of coarctation and exomphalos |
LV, left ventricle.
Of the 14 fetuses with structural cardiac abnormalities, five had trisomy 21. Two of these families chose termination of pregnancy mainly because of the chromosomal abnormality. In both, NT was increased and the transabdominal scans indicated a complete atrioventricular septal defect (AVSD) in one and a VSD in the other. Transvaginal scans were not carried out, as the families opted for fetal karyotyping before further investigations. Postmortem examination confirmed the ultrasound findings in both. Another fetus with trisomy 21 and an AVSD died spontaneously (no postmortem examination was done). For the remaining fetus with this chromosomal abnormality, the family decided to terminate the pregnancy only after a complete AVSD and pulmonary atresia were diagnosed at 14+6 weeks. In one case with a complete AVSD (no invasive tests), trisomy 21 was confirmed at birth. Of the remaining nine fetuses, identification of a major cardiac defect was the main reason for or contributed to a decision to terminate the pregnancy in seven cases (four consented to postmortem examination, where the cardiac diagnoses were confirmed). Two families continued with the pregnancy after the diagnoses of complete transposition of the great arteries at 13+3 weeks in one (fig 2) and a large cardiac diverticulum with pericardial effusion in another (14+4 weeks) (table 1).
In seven fetuses dissimilar sizes of the ventricles on the four chamber view, of the great vessels, or both were observed (fig 3). In five, the indication for fetal echocardiography was increased NT or cystic hygroma on previous scans. Two had chromosomal abnormalities (one with Turner’s syndrome, one with unbalanced translocation, both with increased NT). Of the five fetuses with normal chromosomes, two had a right sided heart and diaphragmatic hernia (confirmed at postmortem examination in one with normal NT; no postmortem examination was done in another with increased NT and associated limb abnormality), two had greatly increased NT but no additional abnormalities on the early scan, and one had an associated exomphalos. Six families decided to terminate the pregnancy. In two cases this decision was only made after follow up scans in mid-gestation, which showed major hypoplasia of the left side of the heart (one with diaphragmatic hernia, one with unbalanced translocation). Four families consented to a postmortem examination, which showed aortic or left ventricular hypoplasia in all (table 2). Two families declined postmortem examination. In the only ongoing pregnancy in this group, the fetus was later shown to have coarctation of the aorta (table 2).
Figure 3.
(A, B) Transabdominal views of a fetus at 13 weeks of gestation with diaphragmatic hernia. (A) Transverse section through the fetal thorax shows ventricular asymmetry (LV < RV) and heart to the right side. (B) Transverse upper mediastinal view shows a narrow transverse aortic arch (arrow). (C, D) Transabdominal views of a fetus at 13 weeks of gestation with (C) greatly increased nuchal translucency (NT, arrow). (D) Aortic arch imaged on power Doppler shows narrowing at the aortic isthmus (arrow). inf, inferior; sup, superior.
Of the 21 abnormal fetuses, the ultrasound findings were confirmed in 14 (10 postmortem examinations, four postnatal scans). The remaining seven fetuses were not examined after death. Overall, the number of fetal pathologies encountered among the 230 fetuses studied was high. There were 23 with chromosomal abnormalities (10%) in the whole group, which included seven of the 21 (33%) fetuses with cardiac anomalies. Four with an AVSD and one with a VSD had trisomy 21. Of the two with a hypoplastic aortic arch, one had Turner’s syndrome and one had an unbalanced translocation. The remaining 14 (67%) patients with a cardiac abnormality had a normal karyotype. There were 32 terminated pregnancies (14%), nine intrauterine deaths (4%), 23 chromosomal abnormalities (10%), and 16 euploid fetuses with major extracardiac abnormalities (7%).
DISCUSSION
Fetal echocardiography carried out at ⩽ 16+0 weeks on fetuses at risk of CHD allowed distinction between normal and abnormal cardiac appearances in the majority of cases (96%). There was a relatively high number of cardiac abnormalities (9%) but early reassurance was possible for most families. For those with an abnormal early scan, the identification of cardiac defects, in isolation or associated with other fetal abnormalities, contributed to a very high rate of termination of pregnancy (76%). Among 199 fetuses considered to have a normal heart at the time of the first examination, 29 (15%) were subsequently shown to have an adverse outcome related to non-cardiac causes, reflecting the high risk of the population studied.
Most CHD encountered in our study were seen in fetuses who had increased NT thickness (16 of 21 cases). Measurement of NT in the first trimester is a non-invasive way of assessing risks of chromosomal abnormalities.8 It is well established in a number of centres in the UK9 and elsewhere. For chromosomally normal fetuses with increased NT, the risk of CHD increases with NT thickness.4,10–12 Mavrides and colleagues11 have shown that in an unselected population, the risk for major CHD increases from 3.1 cases in 1000 (normal NT thickness < 2.5 mm) to 50 abnormalities in 1000 (5% risk) if NT is above the 99th centile for crown to rump length (NT ⩾ 3.5 mm). The latter is similar to the study of Ghi and colleagues,12 who reported a 7% incidence of major CHD in chromosomally normal fetuses with NT > 3.5 mm.
When the criteria for a normal cardiac scan were met, families could be reassured early during their pregnancy, This, together with extracardiac fetal assessment and exclusion of other major fetal abnormalities, was important for continuation of pregnancy. Follow up data showed no major cardiac defect in all but two fetuses, one of whom had a progressive lesion requiring neonatal intervention and the other a large VSD. The former case confirmed observations made by others regarding the progression of certain lesions during pregnancy13 but accounted for < 1% of all normal early scans. This case does, however, stress the need for later follow up both to ensure continuing adequate growth of all cardiac structures and to confirm the early ultrasound findings of normality. Mid-second trimester scans would provide better definition of the septal structures and ascertainment of normal pulmonary venous connections.
That a complex structural malformation of the heart can be diagnosed accurately in early pregnancy has been confirmed in all cases where the heart was available for postmortem examination. The identification of such defects inevitably contributes to a family’s decision to interrupt the pregnancy wherever this is a legal option. Particularly if there are no other major fetal abnormalities, the need for accuracy in the cardiac diagnosis is imperative. To confirm this, as well as to counsel families adequately for subsequent pregnancies, a request for a postmortem examination should be mandatory. High quality pathological assessment of such small hearts, however, is not widely available. This poses difficulties that will need to be addressed by those undertaking early fetal echocardiography.
A group of fetuses presented with disproportion between the right and left sided structures, the natural history of which is still unknown.14 In this group, the early scan raised the possibility of CHD, which may develop further as pregnancy progresses, yet it provided neither the reassurance of a normal scan nor sufficient information to allow families to decide to interrupt the pregnancy because of a fetal cardiac abnormality alone. In our series, five of seven fetuses that presented with asymmetry between right and left sided structures had greatly increased NT, an associated chromosomal abnormality, or both. Two had diaphragmatic hernia, one with increased NT and one with asymmetry but a normal karyotype and normal NT measurement. In one case, later scans were indicative of coarctation of the aorta. When there is ventricular disproportion, the early scan may or may not allow sufficient delineation of the aortic arch to show associated narrowing of the aortic isthmus. This may only be documented with postmortem examination. Hyett and colleagues3 showed that increased NT and isthmal hypoplasia are associated in early pregnancy but, in the absence of other cardiac abnormalities, it is not possible to predict what the postnatal findings will be if a pregnancy continues.
Imaging the fetal heart in the late first and early second trimester of pregnancy is technically more demanding than in mid-gestation because of the relatively smaller size of the fetus and cardiac structures (the semilunar valves are about 1.2 mm at 13 weeks). The quality of images also depends on maternal size and fetal position. The use of colour flow mapping and power Doppler provides useful additional information that allows pattern recognition of the cardiac connections and valve function. The value of this additional information cannot be underestimated.
Our study confirms the feasibility and utility of early cardiac scans for high risk pregnancies, particularly regarding early reassurance. It stresses the need for a combined fetal medicine approach to include cardiac and extracardiac fetal assessment, particularly if NT is increased, whether or not the fetal karyotype is normal.
Acknowledgments
JSC was partially funded by the Hyman Marks Paediatric Research Fund, Royal Brompton Hospital.
Abbreviations
AVSD, atrioventricular septal defect
CHD, congenital heart disease
NT, nuchal translucency
VSD, ventricular septal defect
REFERENCES
- 1.Carvalho JS, Moscoso G, Ville Y. First-trimester transabdominal fetal echocardiography. Lancet 1998;351:1023–7. [DOI] [PubMed] [Google Scholar]
- 2.Huggon IC, Ghi T, Cook AC, et al. Fetal cardiac abnormalities identified prior to 14 weeks gestation. Ultrasound Obstet Gynecol 2002;20:22–9. [DOI] [PubMed] [Google Scholar]
- 3.Hyett J , Moscoso G, Nicolaides K. Increased nuchal translucency in trisomy 21 fetuses: relationship to narrowing of the aortic isthmus. Hum Reprod 1995;10:3049–51. [DOI] [PubMed] [Google Scholar]
- 4.Hyett J , Perdu M, Sharland G, et al. Using fetal nuchal translucency to screen for major congenital cardiac defects at 10–14 weeks of gestation: population based cohort study. BMJ 1999;318:81–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shinebourne EA, Macartney FJ, Anderson RH. Sequential chamber localization: a logical approach to diagnosis in congenital heart disease. Br Heart J 1976;38:327–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anon. Review of the guidance on the research use of fetuses and fetal material (Polkinghorne report). London: Her Majesty’s Stationery Office, 1989.
- 7.Moscoso G , Pexieder T. Variations in microscopic anatomy and ultrastructure of human embryonic hearts subjected to three different modes of fixation. Pathol Res Pract 1990;186:768–74. [DOI] [PubMed] [Google Scholar]
- 8.Nicolaides KH, Azar G, Byrne D, et al. Fetal nuchal translucency: ultrasound screening for chromosomal defects in first trimester of pregnancy. BMJ 1992;304:867–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Snijders RJ, Noble P, Sebire N, et al. UK multicentre project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10–14 weeks of gestation. Lancet 1998;352:343–6. [DOI] [PubMed] [Google Scholar]
- 10.Hyett JA, Perdu M, Sharland GK, et al. Increased nuchal translucency at 10–14 weeks of gestation as a marker for major cardiac defects. Ultrasound Obstet Gynecol 1997;10:242–6. [DOI] [PubMed] [Google Scholar]
- 11.Mavrides E , Cobian-Sanchez F, Tekay A, et al. Limitations of using first-trimester nuchal translucency measurement in routine screening for major congenital heart defects. Ultrasound Obstet Gynecol 2001;17:106–10. [DOI] [PubMed] [Google Scholar]
- 12.Ghi T , Huggon IC, Zosmer N, et al. Incidence of major structural heart defects associated with increased nuchal translucency but normal karyotype. Ultrasound Obstet Gynecol 2001;18:610–4. [DOI] [PubMed] [Google Scholar]
- 13.Yagel S , Weissman A, Rotstein Z, et al. Congenital heart defects: natural course and in utero development. Circulation 1997;96:550–5. [DOI] [PubMed] [Google Scholar]
- 14.Bronshtein M , Zimmer EZ, Gerlis LM, et al. Early ultrasound diagnosis of fetal small left ventricle with a normal proximal outlet tract: a medical dilemma. Prenat Diagn 1997;17:249–53. [DOI] [PubMed] [Google Scholar]